Hong Kong Med J 2023 Aug;29(4):358.e1-2 | Epub 13 Jul 2023
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PCITORIAL MEDICINE
Chronic prostatitis with recurrent extended spectrum
beta-lactamase–producing Escherichia coli bacteraemia treated with prolonged fosfomycin
Michael Tang, MB, BS; Whitney CT Ip, MRCP (UK); Jacqueline KY Yuen, MD; YF Shea, FHKAM (Medicine)
Geriatrics Medical Unit, Grantham Hospital, Hong Kong SAR, China
Corresponding author: Dr YF Shea (syf321@ha.org.hk)
An 84-year-old man was admitted with his third
episode over 4 months of extended-spectrum
beta-lactamase (ESBL)–producing Escherichia coli
bloodstream infection (BSI). He had hypertension,
diabetes mellitus, benign prostatic hyperplasia,
Parkinson’s disease, ischaemic heart disease, and
severe aortic stenosis treated with transcutaneous
aortic valvular implantation. His most recent
glycohaemoglobin level was 6.4% and he was on a controlled diet. He was not on long-term steroids.
His two initial infections (presenting only with
fever) had each been managed with a 2-week
course of intravenous carbapenem and consequent
normalisation of inflammatory markers, white
blood cell (WBC) count and bacterial clearance
on blood culture. Repeated urine culture and liver
biochemistry were unremarkable. Transthoracic
echocardiogram showed no evidence of vegetation.
The patient was readmitted with a 1-day
history of fever with blood culture showing
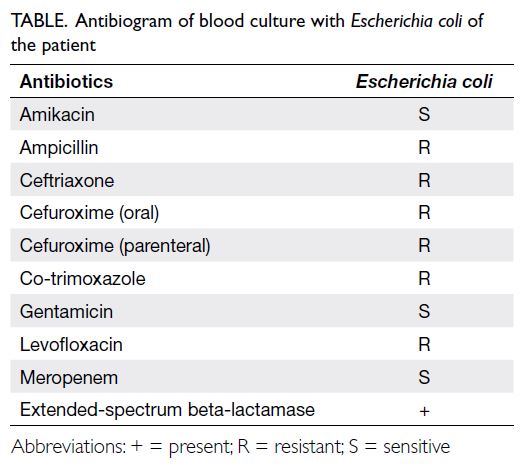
ESBL-producing E coli (refer to the Table for
antibiogram) characterised by leukocytosis (WBC
count=20×109/L). Systemic review revealed no
localising signs or symptoms. We administered
14 days of intravenous meropenem with rapid
defervescence and normalisation of WBC. As a deep-seated
infection was suspected, whole-body gallium
scan was performed and showed intense uptake
over the prostate (Fig a). We decided to treat his
chronic prostatitis with a prolonged regimen of oral
fosfomycin (3 g daily for 1 week, then 3 g every 48
hours for 6 weeks). The patient tolerated fosfomycin
without adverse effects (eg, diarrhoea) and remained
free of reinfection 3 months after discharge; interval
gallium scan showed almost complete resolution of
uptake (Fig b).
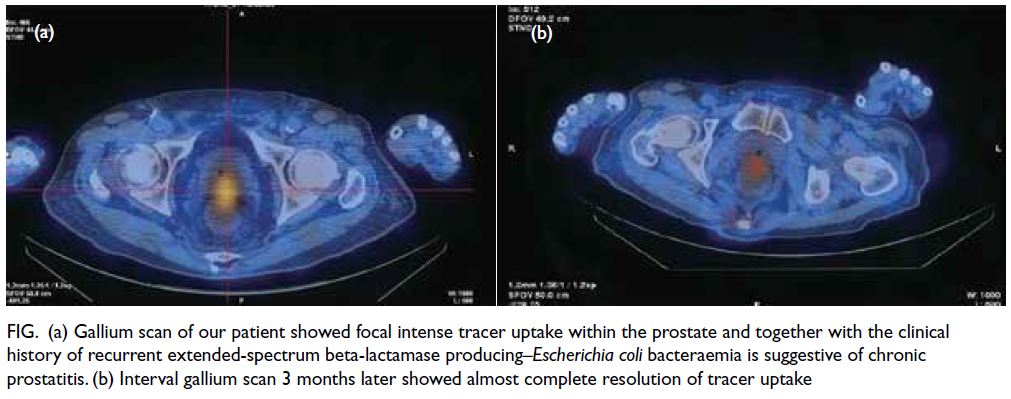
Figure. (a) Gallium scan of our patient showed focal intense tracer uptake within the prostate and together with the clinical history of recurrent extended-spectrum beta-lactamase producing–Escherichia coli bacteraemia is suggestive of chronic prostatitis. (b) Interval gallium scan 3 months later showed almost complete resolution of tracer uptake
The primary site of ESBL-producing E coli BSI is predominantly the urinary tract, but may
include intra-abdominal infections (eg, pyogenic
liver abscess and psoas abscess).1 Typical prostatitis
is diagnosed by a 10-time higher bacterial load in
expressed prostatic fluid or urine sample collected
after prostatic massage than that in a urine
sample without prostatic massage.1 Our patient
was asymptomatic with a negative urine culture;
diagnosis was incidental on gallium scan, confirming
its elusiveness. Once diagnosed, chronic prostatitis
requires prolonged treatment for 4 to 6 weeks with
an appropriate antibiotic.1
Extended-spectrum beta-lactamase–producing
E coli arising from prostatitis has significant
treatment implications. Few oral antibiotics
can adequately penetrate the prostate to be
clinically effective. They include fluoroquinolones,
trimethoprim/sulfamethoxazole, and fosfomycin.2 3
Fosfomycin has a high clinical success rate and
avoids the cardiac and musculoskeletal toxicities
traditionally associated with fluoroquinolones.2 In our centre, it has a striking sensitivity of 97%.4
This report highlights three key points. First,
chronic bacterial prostatitis should be considered in
occult recurrent ESBL-producing Enterobacteriaceae
BSI. Second, oral fosfomycin is an excellent choice for
ESBL-producing E coli. Third, early stepdown from
intravenous to oral antibiotics is effective in real life
and validates historical retrospective studies.2 3 Early
outpatient management is a pragmatic approach that
is especially important within the current context
of the coronavirus disease 2019 pandemic where
healthcare facilities have been often overwhelmed.
Gallium scan or positron emission tomography
should be considered for patients with occult
infection to determine its origin.5
Author contributions
All authors contributed to the concept or design, acquisition of data, analysis or interpretation of data, drafting of the
manuscript, and critical revision of the manuscript for
important intellectual content.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors declared no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patient was treated in accordance with the Declaration of Helsinki and provided informed consent for the treatment/
procedures, and consent for publication.
References
1. Zhanel GG, Zhanel MA, Karlowsky JA. Oral fosfomycin for the treatment of acute and chronic bacterial prostatitis
caused by multidrug-resistant Escherichia coli. Can J
Infect Dis Med Microbiol 2018;2018:1404813. Crossref
2. Tamma PD, Conley AT, Cosgrove SE, et al. Association of 30-day mortality with oral step-down vs continued intravenous therapy in patients hospitalized with Enterobacteriaceae bacteremia. JAMA Intern Med 2019;179:316-23. Crossref
3. Kwan AC, Beahm NP. Fosfomycin for bacterial prostatitis: a review. Int J Antimicrob Agents 2020;56:106106. Crossref
4. Ho PL, Chan J, Lo WU, et al. Prevalence and molecular epidemiology of plasmid-mediated fosfomycin resistance
genes among blood and urinary Escherichia coli isolates. J
Med Microbiol 2013;62:1707-13. Crossref
5. Lin KH, Chen YS, Hu G, Tsay DG, Peng NJ. Chronic bacterial prostatitis detected by FDG PET/CT in a patient
presented with fever of unknown origin. Clin Nucl Med
2010;35:894-5. Crossref