© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Fracture incidence and fracture-related mortality
decreased with decreases in population mobility during the early days of the COVID-19 pandemic: an epidemiological study
Janus SH Wong, MB, BS, MRCSEd1; Christian X Fang, FRCSEd, FHKCOS1; Alfred LH Lee, MB, BS, MRCP2; Dennis KH Yee, FRCSEd, FHKCOS3; Kenneth MC Cheung, FRCS (Eng), FHKCOS1; Frankie KL Leung, FRCSEd, FHKCOS1
1 Department of Orthopaedics and Traumatology, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong
2 Department of Microbiology, Prince of Wales Hospital, Hong Kong
3 Department of Orthopaedics and Traumatology, Alice Ho Miu Ling Nethersole Hospital, Hong Kong
Corresponding author: Dr Christian X Fang (cfang@hku.hk)
Abstract
Introduction: We investigated the impact of
coronavirus disease 2019 (COVID-19) social
distancing measures on fracture incidence and
fracture-related mortality, as well as associations
with population mobility.
Methods: In total, 47 186 fractures were analysed
across 43 public hospitals from 22 November 2016
to 26 March 2020. Considering the smartphone
penetration of 91.5% in the study population,
population mobility was quantified using Apple
Inc’s Mobility Trends Report, an index of internet
location services usage volume. Fracture incidences
were compared between the first 62 days of social
distancing measures and corresponding preceding
epochs. Primary outcomes were associations
between fracture incidence and population mobility,
quantified by incidence rate ratios (IRRs). Secondary
outcomes included fracture-related mortality rate
(death within 30 days of fracture) and associations
between emergency orthopaedic healthcare demand
and population mobility.
Results: Overall, 1748 fewer fractures than
projected were observed during the first 62 days of
COVID-19 social distancing (fracture incidence:
321.9 vs 459.1 per 100 000 person-years, P<0.001);
the relative risk was 0.690, compared with mean
incidences during the same period in the previous
3 years. Population mobility exhibited significant associations with fracture incidence (IRR=1.0055,
P<0.001), fracture-related emergency department
attendances (IRR=1.0076, P<0.001), hospital
admissions (IRR=1.0054, P<0.001), and subsequent
surgery (IRR=1.0041, P<0.001). Fracture-related
mortality decreased from 4.70 (in prior years) to
3.22 deaths per 100 000 person-years during the
COVID-19 social distancing period (P<0.001).
Conclusion: Fracture incidence and fracture-related
mortality decreased during the early days of the
COVID-19 pandemic; they demonstrated significant
temporal associations with daily population mobility,
presumably as a collateral effect of social distancing
measures.
New knowledge added by this study
- A significant reduction in fracture incidence was observed during the early days of the coronavirus disease 2019 pandemic.
- Daily fracture incidence was temporally associated with population mobility.
- Data regarding population mobility could facilitate estimation of fracture incidence and be used (along with many other factors) to estimate clinical service demand for timely management of public health responses involving changes in population mobility.
- As digital literacy increases, population digital usage patterns could support epidemiological investigations and address gaps in conventional data sources.
Introduction
The coronavirus disease 2019 (COVID-19)
pandemic, which began in early 2020, has resulted
in unprecedented large-scale public health responses. Stringent regional social distancing
measures (eg, quarantine, school closures, and
restrictions at work and recreation destinations)
were rapidly implemented during the early days of the pandemic as forms of non-pharmacological
intervention.1 Although there is evidence that such
measures can temporarily contain the spread of
severe acute respiratory syndrome coronavirus 2,2
collateral effects among non–COVID-19–related
conditions have also been reported.3 Trauma is the
leading cause of death and disability among young
adults worldwide,4 but the effects of the COVID-19
pandemic on injuries and fracture incidence within
Hong Kong have not been fully elucidated. This
uncertainty has hindered healthcare resource
deployment and clinical service demand estimation
in times of stringency. We sought to address this
problem using ‘big data’ sources and regional clinical
data repositories, which allow researchers to rapidly
delineate epidemiological associations with potential
applications in forecasting models, while avoiding
resource-intensive collection of conventional
epidemiological information and protecting patient
anonymity.
We presumed that restrictions on citizen
mobility, in concert with social distancing, were
associated with reductions in musculoskeletal
injuries during the early days of the COVID-19
pandemic. Specifically, we hypothesised that reduced population mobility was associated with reductions
in fracture incidence and fracture-related healthcare
needs during the early days of the pandemic. We
investigated these relationships by analysing daily
multicentre hospital data registries in Hong Kong,
along with digital population mobility datasets
published by a technology company. Our main
outcome measurement was skeletal fractures, which
served as a specific surrogate for musculoskeletal
trauma.
Methods
Data collection
This study was conducted in Hong Kong, a highincome
region (with gross domestic product per
capita of HK$357 667 in 20205) that was among the
first areas affected by COVID-19; social distancing
measures were implemented during the early days of
the pandemic.
Using the Clinical Data Analysis and Reporting
System of the Hospital Authority, anonymised patient
records were retrieved from all 43 public hospitals in
Hong Kong for the period from 22 November 2016 to
20 May 2020. In Hong Kong, up to 90% of hospital bed-days
occur in public hospitals, which manage nearly
all critical emergencies in the region.6 Anonymised
clinical data were retrieved, including time of initial
injury presentation, emergency department triage,
trauma category, hospital admission, diagnosis,
and surgical procedures. Diagnoses and procedures
were encoded in accordance with the International
Classification of Diseases, Ninth Revision, Clinical
Modification (ICD-9-CM) by treating physicians
based on clinical and radiological investigations,
intraoperative findings, and date of hospital
discharge. The ICD-9-CM codes that met the
inclusion criteria (which included fractures under
the purview or commonly admitted under the care
of orthopaedic and traumatology service) were all
codes from 805 to 829 (inclusive). Duplicate records
from fracture reassessment related to follow-up
attendances, hospitalisation after emergency
department attendance, and elective hospital re-admissions
(ie, episodes assigned to the same patient
unique identifier with identical diagnostic codes,
which occurred within 30 days of the index episode)
were regarded as a single event to avoid double
counting. Pathological fractures and records with
missing diagnosis codes or admission times were
excluded from the analysis.
Time intervals
The ‘COVID-19 epoch’ was defined as 25 January
2020 (activation of the government’s ‘emergency’
response and commencement of social distancing
policies7) to 26 March 2020; this arbitrarily chosen
62-day period included all patients with fractures who presented during that period. This epoch was
compared with the 9 weeks preceding the onset of
the COVID-19 pandemic (ie, 22 November 2019 to
24 January 2020), as well as the same period over
the past 3 years to adjust for seasonality-related
variations8 (ie, 25 January to 26 March in 2017, 2018,
and 2019). Differences between actual and projected
daily fracture incidences were calculated based on
mean values at the same time of year over the past
3 years. Fracture-related mortality rates, defined as
the numbers of deaths within 30 days after initial
fracture presentation per 100 000 person-years, were
compared. The Chi squared test was used to detect
differences in fracture incidence and fracture-related
mortality during the COVID-19 pandemic and pre-pandemic
epochs.
Quantifying population mobility
Surrogate data concerning population mobility
were retrieved from Mobility Trends Reports9—an
aggregate daily measure of geographical direction
requests on Apple Maps, a service established by
Apple Inc, which holds the largest market share of
electronic mobile devices (including smartphones
and tablets) in Hong Kong.10 Walking index was
regarded as an index of population mobility,
considering the smartphone penetration of 91.5%11
among the 7.50 million residents of Hong Kong.12
Data analysis
Associations between daily fracture incidence and
population mobility were determined by incidence
rate ratios (IRRs) using quasi-Poisson regression.
Secondary analysis involved associations between
mobility index and fracture repair surgeries, all types
of orthopaedic emergency department attendances,
orthopaedic hospital admissions, and emergency
orthopaedic surgeries.
Because medical records were timestamped in
Hong Kong time (8 hours ahead of Greenwich Mean
Time), they were converted to Pacific Time to match
the time intervals listed in Mobility Trends Reports;
this conversion ensured that data were temporally
matched for analysis.
To determine whether mobility associations
simply reflected health-seeking behaviour, we
included analyses of diseases which lacked a
physiological basis and were not associated with
population mobility—these ‘controls’ included
appendicitis, cellulitis, and abscess (ICD-9-CM
diagnosis codes 540 and 682). Statistical analysis
was performed using R software, version 3.6.2 (R
Foundation for Statistical Computing, Vienna,
Austria). Quasi-Poisson regression was used to
model the relationship between the population
mobility index and the daily incidences of fractures
and fracture-related events; the population mobility
index was the explanatory variable, whereas the
daily incidences of various events were response
variables. A quasi-Poisson distribution was
preferred over a Poisson distribution, considering
the presence of significant overdispersion among
some response variables (in the form of count data)
when a dispersion parameter was included. In
accordance with standard statistical methods, the
natural logarithm was utilised as the link function.
Incidence rate ratios were reported and represented
by the following formula:
Estimated incidence = IRRPMI × BIR
where IRR represents the incidence rate ratio, PMI represents the population mobility index, and BIR
represents the baseline incidence rate. The IRR, which
quantifies the relationship between the mobility
index and fracture incidence, is multiplicative in
nature—for every unit increase in the mobility index,
there is a corresponding multiplicative increase in
the IRR. If the IRR is <1, it is expected to decrease
in a multiplicative manner for every unit decrease
in the mobility index. Multiple comparisons were
adjusted by Bonferroni correction, and the threshold
for statistical significance was regarded as P<0.00227
(0.05/22).
Results
In total, 59 931 fracture-related medical records from
orthopaedic emergency department attendances,
hospital admissions, and surgeries were reviewed.
After exclusion of 11 498 linked episodes, 284
pathological fractures, 786 follow-up attendances,
175 hospital re-admissions, and two episodes with
missing admission times, 47 186 fractures were
included in the analysis. Descriptive statistics
regarding daily fracture incidences, controls, and
fracture-related surgeries during COVID-19 social
distancing are shown in Table 1. Intra-year and inter-year
comparison cohorts are presented in Table 2.
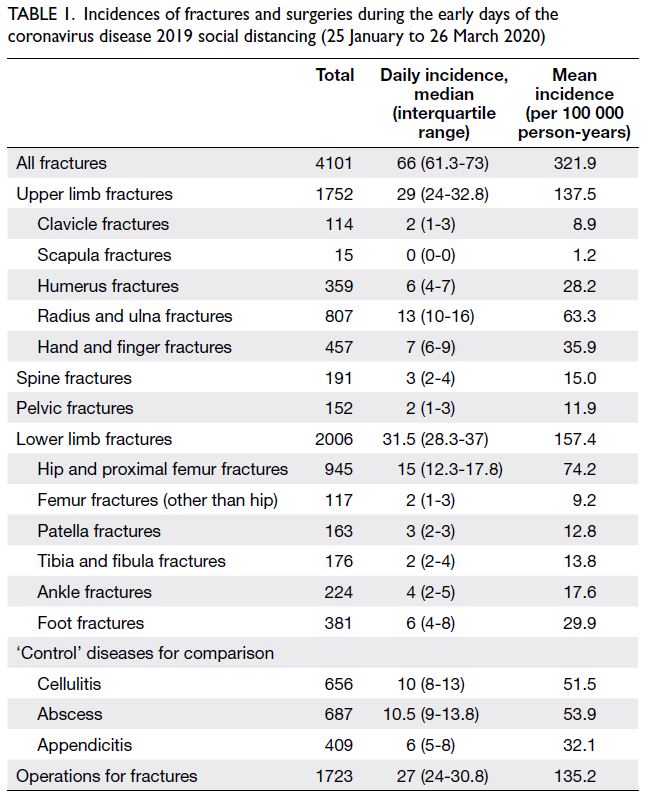
Table 1. Incidences of fractures and surgeries during the early days of the coronavirus disease 2019 social distancing (25 January to 26 March 2020)
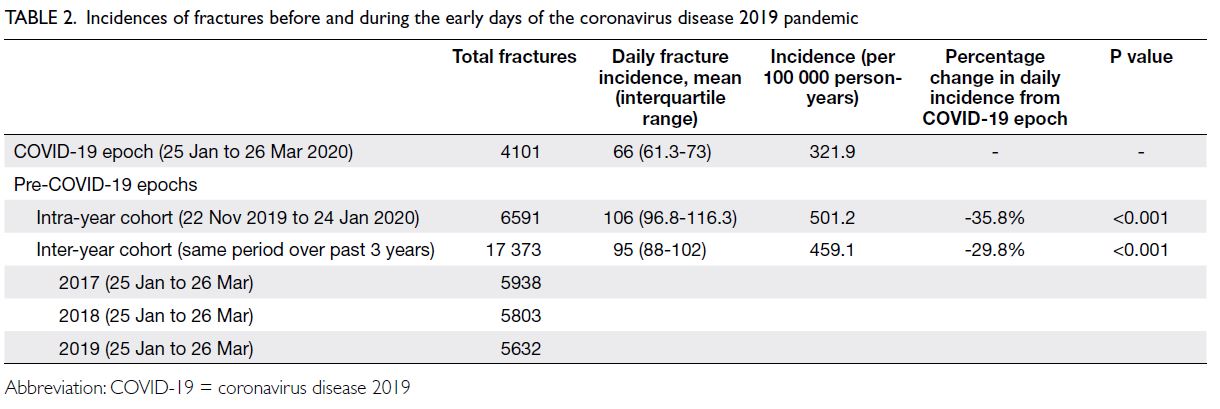
Table 2. Incidences of fractures before and during the early days of the coronavirus disease 2019 pandemic
Fracture incidence during COVID-19 social
distancing
A reduction of 1748 fractures in the actual versus
projected incidence (321.9 vs 459.1 per 100 000
person-years, P<0.001) was observed during the
COVID-19 epoch; the relative risk was 0.690 (95%
confidence interval [CI]=0.678-0.702), compared
with mean incidences in the previous 3 years (ie,
inter-year cohort) [Table 2]. Differences in fracture
incidence between the pandemic and pre-pandemic
epochs are shown in Figure 1.
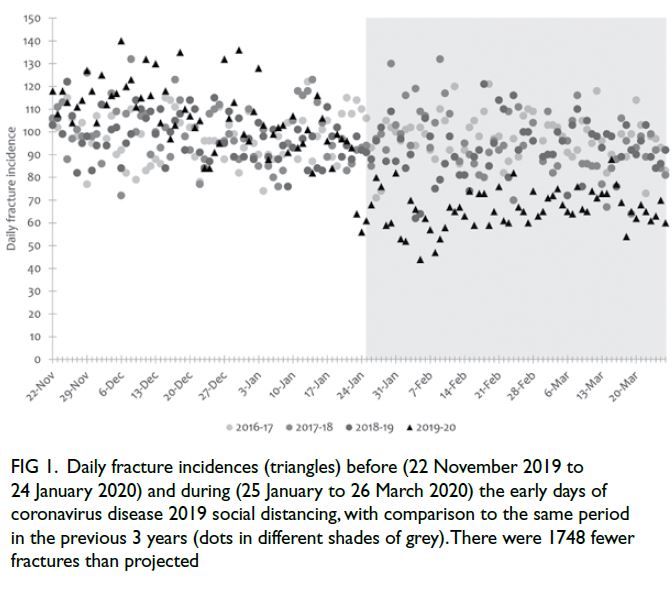
Figure 1. Daily fracture incidences (triangles) before (22 November 2019 to 24 January 2020) and during (25 January to 26 March 2020) the early days of coronavirus disease 2019 social distancing, with comparison to the same period in the previous 3 years (dots in different shades of grey). There were 1748 fewer fractures than projected
Fracture incidences, population mobilities,
and controls are depicted in Figure 2. The first two
COVID-19 cases in Hong Kong were reported on 23
January 202013; three additional cases were reported
on 24 January 2020. Social distancing measures were
implemented on 25 January 2020; these included
suspension of schools, initiation of ‘work from home’ measures among civil servants, and suspension of
hospital visitations. Mandatory border quarantine
was enforced on 8 February 2020. The sharpest
decrease in mobility was observed on 24 January
2020; population mobility subsequently remained at low levels, in conjunction with cancellations of
large-scale social and sporting events, as well as the
imposition of travel restrictions with quarantine
measures for returning travellers.7
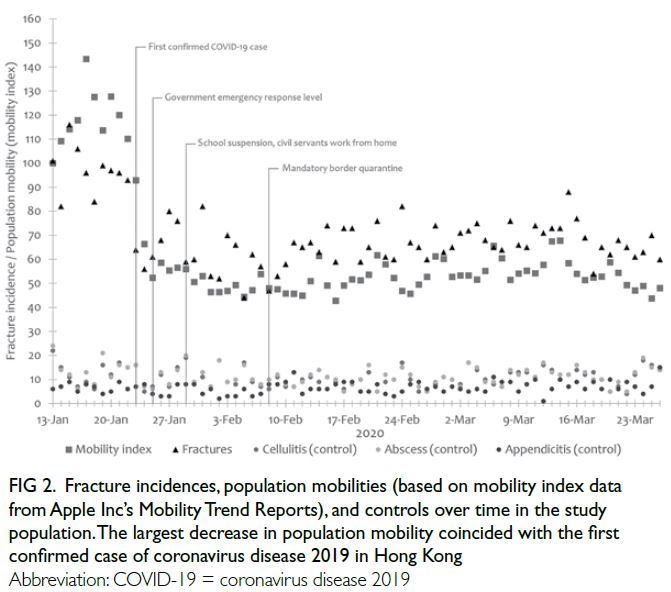
Figure 2. Fracture incidences, population mobilities (based on mobility index data from Apple Inc’s Mobility Trend Reports), and controls over time in the study population. The largest decrease in population mobility coincided with the first confirmed case of coronavirus disease 2019 in Hong Kong
Associations of fracture incidence with
population mobility
Fracture incidence was positively associated with
the population mobility index (IRR=1.0055, 95%
CI=1.0044-1.0066, P<0.001). Analyses of fracture
incidence according to anatomical location revealed
associations of the population mobility index with
upper limb fractures (IRR=1.0073, 95% CI=1.0057-1.0088, P<0.001) and lower limb fractures
(IRR=1.0045, 95% CI=1.0030-1.0060, P<0.001) [Fig 3].
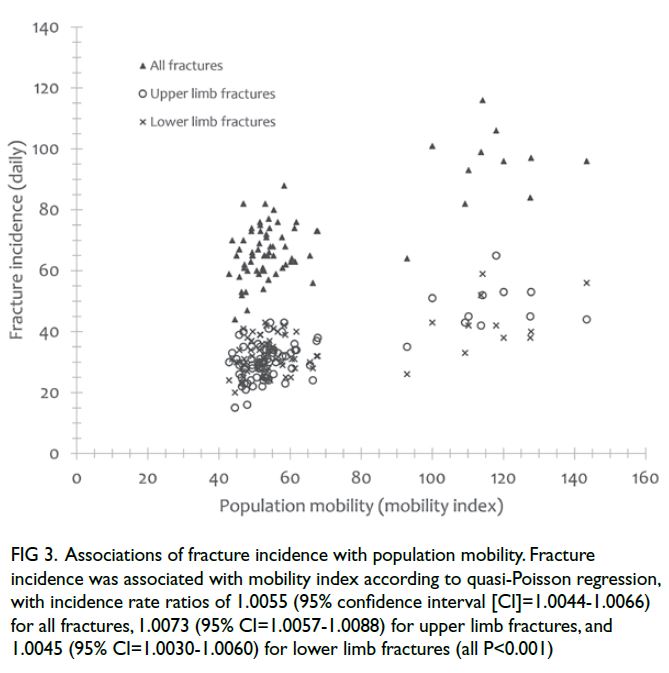
Figure 3. Associations of fracture incidence with population mobility. Fracture incidence was associated with mobility index according to quasi-Poisson regression, with incidence rate ratios of 1.0055 (95% confidence interval [CI]=1.0044-1.0066) for all fractures, 1.0073 (95% CI=1.0057-1.0088) for upper limb fractures, and 1.0045 (95% CI=1.0030-1.0060) for lower limb fractures (all P<0.001)
The population mobility index was associated
with the incidences of fractures involving the
radius and ulna (IRR=1.0079, 95% CI=1.0057-1.0101, P<0.001), hand and fingers (IRR=1.0069,
95% CI=1.0039-1.0098, P<0.001), femoral neck
(IRR=1.0065, 95% CI=1.0035-1.0095, P<0.001),
and tibia and fibula (IRR=1.0097, 95% CI=1.0044-1.0151, P<0.001) [Fig 4]. However, after Bonferroni
correction, the population mobility index did not
exhibit statistically significant associations with
trochanteric hip fractures (IRR=1.0008, P=0.683),
spine fractures (IRR=0.996, P=0.183), or pelvic
fractures (IRR=1.0064, P=0.00799).
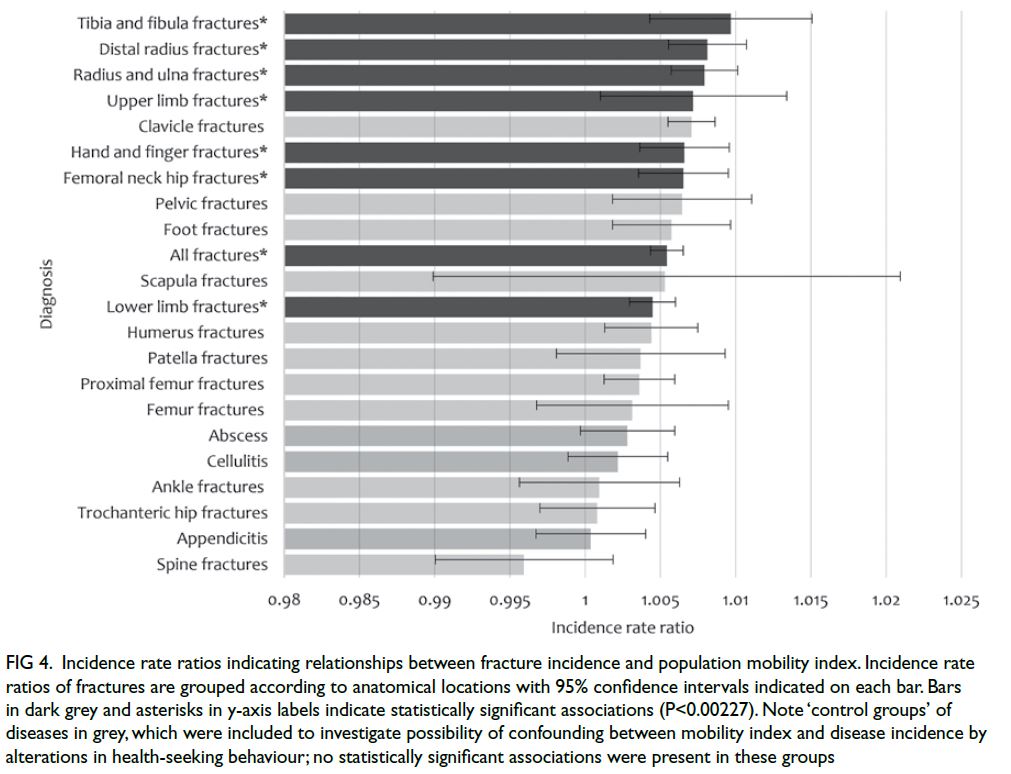
Figure 4. Incidence rate ratios indicating relationships between fracture incidence and population mobility index. Incidence rate ratios of fractures are grouped according to anatomical locations with 95% confidence intervals indicated on each bar. Bars in dark grey and asterisks in y-axis labels indicate statistically significant associations (P<0.00227). Note ‘control groups’ of diseases in grey, which were included to investigate possibility of confounding between mobility index and disease incidence by alterations in health-seeking behaviour; no statistically significant associations were present in these groups
Stronger associations were observed among
fractures, such that some patients presented at a
younger age (eg, patients with tibia, fibula, hand, and
finger fractures), whereas other patients presented
at an older age (eg, patients with femoral neck
fractures). Digital literacy, manual dexterity and
visual acuity, and higher internet and smartphone
usage among younger residents11 are among the
factors that cause the population mobility index to
have increased sensitivity for analysis in such age-groups.
The incidences of cellulitis, abscesses, and
appendicitis were not associated with the population
mobility index (P>0.00227). These findings support
the hypothesis that changes in associations between
fracture incidence and population mobility were
not solely caused by changes in health-seeking
behaviour; if they had been caused by changes in
such behaviour, corresponding reductions in those
conditions would have been observed.
Secondary exploratory analysis of surgeries,
emergency department attendances, and
hospital admissions
The daily population mobility index was associated
with the number of patients admitted on a particular
day who subsequently underwent fracture repair
surgeries (IRR=1.0041, 95% CI=1.0020-1.0062,
P<0.001). The population mobility index was also
associated with all types of emergency orthopaedic
surgeries (IRR=1.0040, 95% CI=1.0021-1.0058,
P<0.001), attendances at orthopaedic emergency
departments (IRR=1.0076, 95% CI 1.0064-1.0087,
P<0.001), and emergency orthopaedic hospital
admissions (IRR=1.0054, 95% CI=1.0043-1.0064,
P<0.001). Additionally, the numbers of orthopaedic
patients triaged as critical, emergent, and urgent
(ie, patients who require physician attention within
30 minutes of attendance) were also associated
with the population mobility index (IRR=1.0063,
95% CI=1.0054-1.0073, P<0.001). Whereas the
numbers of traffic-related and sports-related trauma
cases were associated with the population mobility
index (IRR=1.008, 95% CI=1.0063-1.0097 and
IRR=1.013, 95% CI=1.0092-1.0158, respectively,
both P<0.001), the number of assault-related trauma
cases was not (P=0.238).
Fracture-related mortality rate
Forty-nine patients with fractures died within
30 days of presentation during the COVID-19 epoch.
This constituted a mortality rate of 3.22 deaths per
100 000 person-years, which was lower than the rate
of 4.70 deaths per 100 000 person-years during the
period before the pandemic (P<0.001); thus, there
were around 19 fewer fracture-related deaths in
the Hong Kong population during the 62-day study
period. Four patients with fractures had COVID-19 (ie, they had positive results in nasopharyngeal
swab reverse transcriptase-polymerase chain
reaction tests for severe acute respiratory syndrome
coronavirus 2) and survived beyond 30 days after
initial fracture presentation. The change in mortality
was presumably explained by reduced fracture
incidence: 30-day mortality among patients with
fractures did not significantly differ between the
COVID-19 epoch (1.2%, 49 deaths in 4101 patients)
and the preceding period (1.0%, 175 deaths in 17 198
patients) [P=0.305].
Discussion
This study analysed 47 186 fractures in Hong Kong,
prior to and during the early days of the COVID-19
pandemic. Population mobility was assessed through
aggregate digital footprints using the volume of
location service requests as a surrogate marker, considering the high smartphone and internet
penetration in Hong Kong11; importantly, datasets of
aggregate digital footprints have been published to
facilitate efforts to control COVID-19.9 The findings
support our hypothesis in terms of the relationship
between fracture incidence and population mobility.
Fractures incur substantial healthcare costs;
for example, fragility fracture-related costs incurred
costs of 37.5 billion euros, along with the loss of 1.0
million quality-adjusted life years, among the six
largest European countries in 2017.14 Some fractures
(eg, hip fractures) warrant early surgical management
to mitigate the morbidity and mortality associated
with surgical delays.15 Guidance regarding early
surgical management remained in effect, even during
the early days of the COVID-19 pandemic.16 Despite
the best available tools, fracture prediction remains
difficult; there are additional challenges associated
with epidemiological projections of specific time
points when such fractures occur. Accordingly,
hospitals and public health entities experience
difficulties in terms of estimating emergency trauma
service load and allocating limited healthcare
resources. Our findings suggest that population
mobility indices, which are freely and publicly
accessible, can provide insights regarding fracture incidence. Population mobility may be useful in
quantitative modelling of fracture-related inpatient
and surgical theatre service demand, using the IRRs
described in this study.
Although there is evidence to support the
efficacy of social distancing measures with respect to
COVID-19 transmission,2 our findings emphasise the
collateral impacts of pandemic-related interventions
on non-communicable diseases. We found that
fracture incidence decreased when population
mobility was hindered by social distancing measures;
the relative reduction in overall fractures appeared to
be similar to the effect of established pharmacological
interventions on fragility fractures.17 Although this
relationship appears to contradict the common
notion that physical activity confers a protective
effect against fractures in both young and old age-groups,
18 19 associations of increased fracture risk
with specific types of exercises (eg, bicycling), or
regular participation in other exercise and sports
activities, have been described.20 Thus, long-term
benefits (eg, increased bone mineral density) may
be accrued at the expense of increased exposure
to fracture risk when engaging in physical activity.
Although the long-term impact of reduced
population mobility on fracture incidence remains
unclear, vitamin D deficiency caused by prolonged
time indoors (ie, without sunlight exposure) is an
established risk factor for future fractures.21
The strengths of our study include its inclusion
of data from all public hospitals in Hong Kong,
which allowed extensive analysis of rare events
such as fractures. Our database has a high (>96%)
positive predictive value for fractures,22 presumably
because data entry is conducted by impartial
registered medical practitioners. Furthermore, high
internet and smartphone penetration increased the
sensitivity of the population mobility analysis, such
that the mobility index was geographically specific
to the study population. Pedestrian and road traffic
densities, which are indirectly represented by the
population mobility index, could also precipitate
accidents, falls, and subsequent fracture risk.
Additionally, potential confounding based on
health-seeking behaviour was partially mitigated
by the inclusion of ‘control’ groups. Fortunately,
all hospitals involved in the study maintained
full emergency service during the early days of
the COVID-19 pandemic23; this maintenance of
emergency service minimised potential confounding
by hospitals that were unable to provide service to
patients with fractures.
Limitations of the study involved deficiencies
in the population mobility index. For example,
travel between familiar places and travel where
navigation guidance is unnecessary, as well as the
usage of alternative electronic service providers,
were not considered. Therefore, the population mobility index served as a more specific (rather than
sensitive) tool for assessment of population mobility.
Global positioning system (GPS)–based mobility
tracking would theoretically allow more extensive
data collection, thus providing greater detection
sensitivity; however, such mobility tracking would
cause substantial privacy issues, resulting in legal
and ethical challenges.
Notably, older adults are less adept in
smartphone usage (62.2% of residents aged ≥65
years reported internet usage in 202011), and
the digital population mobility index does not
adequately illustrate this division in the population.
Furthermore, fractures in older adults are largely
caused by osteoporosis, whereas high-energy injury
mechanisms are observed in younger individuals.24
Therefore, social distancing may have a negligible
effect on the incidences of osteoporotic fractures
sustained indoors. We caution against using
population mobility data as the sole source of
estimates for health service planning because that
approach could underestimate fragility fracture
service demand.
Additionally, the use of fracture incidence data
from a public healthcare database only included
approximately 90% of the population health
demand. During the early days of the COVID-19
pandemic, instances of diversion to the private
sector, attendances in private clinics, and visits to
alternative practitioners were not coded; the lack
of these data may have led to underestimation of
total fracture incidence. Finally, we caution against
generalising these findings to regions with less
internet and smartphone penetration.
Conclusion
During the early days of the COVID-19 pandemic,
fracture incidence and fracture-related mortality
considerably decreased with the implementation of
government social distancing measures that targeted
population mobility. This unique opportunity
enabled the identification of collateral associations
and revealed that population mobility could be used
(along with many other factors) to estimate clinical
service demand.
Author contributions
Concept or design: JSH Wong, DKH Yee.
Acquisition of data: JSH Wong.
Analysis or interpretation of data: JSH Wong, ALH Lee, DKH Yee, CX Fang.
Drafting of the manuscript: JSH Wong, ALH Lee, CX Fang.
Critical revision of the manuscript for important intellectual content: CX Fang, DKH Yee, FKL Leung, KMC Cheung.
Acquisition of data: JSH Wong.
Analysis or interpretation of data: JSH Wong, ALH Lee, DKH Yee, CX Fang.
Drafting of the manuscript: JSH Wong, ALH Lee, CX Fang.
Critical revision of the manuscript for important intellectual content: CX Fang, DKH Yee, FKL Leung, KMC Cheung.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
Ethics approval was granted by the Institutional Review Board of The University of Hong Kong/ Hospital Authority
Hong Kong West Cluster (HKU/HA HKW IRB Ref No.: UW
20-275), and investigations were carried out in accordance
with the Declaration of Helsinki. The requirement for patient
informed consent was waived by the Board because the study
used anonymised data and the risk of identification was low.
References
1. Leung K, Wu JT, Liu D, Leung GM. First-wave COVID-19
transmissibility and severity in China outside Hubei after
control measures, and second-wave scenario planning: a
modelling impact assessment. Lancet 2020;395:1382-93. Crossref
2. Cousins S. New Zealand eliminates COVID-19. Lancet 2020;395:1474. Crossref
3. De Filippo O, D’Ascenzo F, Angelini F, et al. Reduced rate
of hospital admissions for ACS during Covid-19 outbreak
in Northern Italy. N Engl J Med 2020;383:88-9. Crossref
4. Krug EG, Sharma GK, Lozano R. The global burden of injuries. Am J Public Health 2000;90:523-6. Crossref
5. Census and Statistics Department, Hong Kong SAR
Government. Table 31: Gross Domestic Product (GDP),
implicit price deflator of GDP and per capita GDP. 2020.
Available from: https://www.censtatd.gov.hk/en/web_table.html?id=31. Accessed 26 Apr 2020.
6. Food and Health Bureau, Hong Kong SAR Government.
Report of the Strategic Review on Healthcare Manpower
Planning and Professional Development. 2017. Available
from: https://www.fhb.gov.hk/en/press_and_publications/otherinfo/180500_sr/srreport.html. Accessed 20 May 2020.
7. Leung GM, Cowling BJ, Wu JT. From a sprint to a marathon in Hong Kong. N Engl J Med 2020;382:e45. Crossref
8. Yee DK, Fang C, Lau TW, Pun T, Wong TM, Leung F. Seasonal variation in hip fracture mortality. Geriatr
Orthop Surg Rehabil 2017;8:49-53. Crossref
9. Apple Inc. COVID-19–mobility trends reports. Available from: https://www.apple.com/covid19/mobility. Accessed 26 Apr 2020.
10. Statcounter GlobalStats. Mobile & tablet vendor market
share Hong Kong. Jan – Mar 2020. Available from: https://gs.statcounter.com/vendor-market-share/mobile-tablet/hong-kong/#monthly-202001-202003. Accessed 26 Apr 2020.
11. Census and Statistics Department, Hong Kong SAR Government. Thematic Household Survey Report No. 69: Personal Computer and Internet Penetration. 2020.
Available from: https://www.ogcio.gov.hk/en/about_us/facts/doc/householdreport2020_69.pdf. Accessed 5 May 2020.
12. Census and Statistics Department, Hong Kong SAR
Government. Population– Overview. 2020. Available
from: https://www.censtatd.gov.hk/hkstat/sub/so20.jsp. Accessed 12 Apr 2020.
13. Centre for Health Protection, Department of Health,
Hong Kong SAR Government. Latest situation of novel
coronavirus infection in Hong Kong. Available from: https://chp-dashboard.geodata.gov.hk/covid-19/en.html. Accessed 12 Apr 2022.
14. Borgström F, Karlsson L, Ortsäter G, et al. Fragility fractures
in Europe: burden, management and opportunities. Arch
Osteoporos 2020;15:59. Crossref
15. Leung F, Lau TW, Kwan K, Chow SP, Kung AW. Does timing
of surgery matter in fragility hip fractures? Osteoporos Int
2010;21 Suppl 4:S529-34. Crossref
16. British Orthopaedic Association. COVID BOAST-Management
of patients with urgent orthopaedic
conditions and trauma during the coronavirus pandemic.
Available from: https://www.boa.ac.uk/resources/covid-19-boasts-combined1.html. Accessed 13 Feb 2023.
17. Tsuda T, Hashimoto Y, Okamoto Y, Ando W, Ebina K.
Meta-analysis for the efficacy of bisphosphonates on hip
fracture prevention. J Bone Miner Metab 2020;38:678-86. Crossref
18. Fritz J, Cöster ME, Nilsson JA, Rosengren BE, Dencker M,
Karlsson MK. The associations of physical activity with
fracture risk—a 7-year prospective controlled intervention
study in 3534 children. Osteoporos Int 2016;27:915-22. Crossref
19. Morseth B, Ahmed LA, Bjørnerem Å, et al. Leisure time
physical activity and risk of non-vertebral fracture in men
and women aged 55 years and older: the Tromsø study. Eur
J Epidemiol 2012;27:463-71. Crossref
20. Appleby PN, Allen NE, Roddam AW, Key TJ. Physical
activity and fracture risk: a prospective study of 1898
incident fractures among 34,696 British men and women. J
Bone Miner Metab 2008;26:191-8. Crossref
21. Nilson F, Moniruzzaman S, Andersson R. A comparison
of hip fracture incidence rates among elderly in Sweden
by latitude and sunlight exposure. Scand J Public Health
2014;42:201-6. Crossref
22. Sing CW, Woo YC, Lee AC, et al. Validity of major
osteoporotic fracture diagnosis codes in the Clinical
Data Analysis and Reporting System in Hong Kong.
Pharmacoepidemiol Drug Saf 2017;26:973-6. Crossref
23. Hospital Authority, Hong Kong SAR Government. HA adjusts service provision to focus on combatting epidemic.
2020. Press Release. Available from: https://www.info.gov.hk/gia/general/202002/10/P2020021000711.htm.
Accessed 20 May 2020.
24. Bergh C, Wennergren D, Möller M, Brisby H. Fracture
incidence in adults in relation to age and gender: a study of
27,169 fractures in the Swedish Fracture Register in a well-defined
catchment area. PLoS One 2020;15:e0244291. Crossref

