Hong Kong Med J 2023 Feb;29(1):82-3 | Epub 13 Jan 2023
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
COMMENTARY
Impact of COVID-19 on the mortality of dialysis
patients and kidney transplant recipients during the Omicron fifth wave in Hong Kong
KM Chow, MB, ChB, FRCP1; John YH Chan, MB, ChB, FRCP2; Sunny SH Wong, MB, BS, FRCP3; SK Yuen, MB, ChB, FRCP4; PN Wong, MB, ChB, FRCP5; YL Cheng, MB, ChB, FRCP6; CC Szeto, MB, ChB, MD1
1 Department of Medicine and Therapeutics, Prince of Wales Hospital, The Chinese University of Hong Kong, Hong Kong
2 Department of Medicine, Queen Elizabeth Hospital, Hong Kong
3 Department of Medicine and Geriatrics, United Christian Hospital, Hong Kong
4 Department of Medicine and Geriatrics, Caritas Medical Centre, Hong Kong
5 Department of Medicine and Geriatrics, Kwong Wah Hospital, Hong Kong
6 Department of Medicine, Alice Ho Miu Ling Nethersole Hospital, Hong Kong
Corresponding author: Dr KM Chow (chow_kai_ming@alumni.cuhk.net)
During the fifth wave of novel coronavirus disease 2019 (COVID-19) caused by the Omicron variant
of severe acute respiratory syndrome coronavirus 2
(SARS-CoV-2) in Hong Kong, the reported mortality
rate of 37.7 per million population was one of the
highest worldwide.1 This pandemic wave provided
a unique opportunity to assess the impact of
COVID-19 on the mortality of patients receiving
peritoneal dialysis, haemodialysis or kidney
transplantation. Among them, peritoneal dialysis
patients had been perceived to be less vulnerable to
SARS-CoV-2 infection because their treatment was
home-based with better protection by self-isolation.
On the contrary, in-centre haemodialysis patients
were perceived to have a higher likelihood of
infection due to practical challenges of maintaining
social distancing within a crowded dialysis unit.2 3 4 5
Estimates of SARS-CoV-2 incidence are
heavily influenced by the frequency and intensity of
surveillance. As such, the prevalence of COVID-19
infection may have been underestimated for
peritoneal dialysis patients compared with that of
haemodialysis patients. Furthermore, peritoneal
dialysis patients are less likely to be hospitalised
after infection so the exact disease burden might
not be easily assessed. Collider bias, therefore, is
a problem encountered when both the risk factor
(haemodialysis) and the factor on the pathway to
the outcome of interest (for instance, hospitalisation
on the pathway to death) influence the mechanisms
behind selection into a study sample population.6 7
To overcome this bias, we determined the mortality
of COVID-19 for all patients separately for each
mode of renal replacement therapy (instead of the
infected population). We retrospectively analysed
six large renal units in Hong Kong and included
patients between 1 October 2021 and 30 April
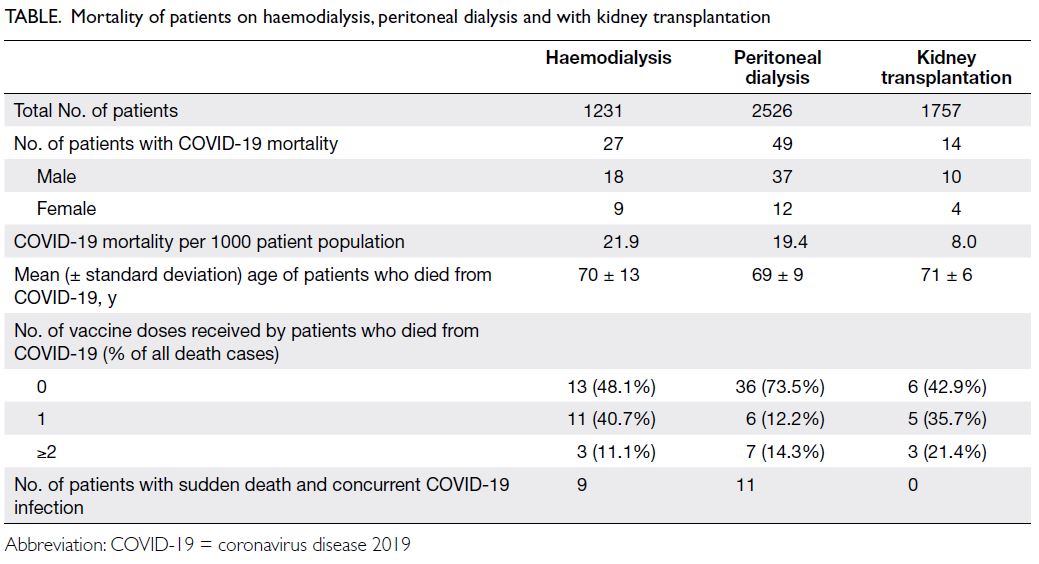
2022. Of the 5514 patients, 1231 (22.3%) were
on haemodialysis, 2526 (45.8%) on peritoneal dialysis, and 1757 (31.9%) were kidney transplant
recipients. Mortality of COVID-19, defined as
death due to COVID-19 infection in the absence of
a clear alternative cause (such as peritonitis),8 was
estimated from death registry and chart review.
Data for uncertain causes of death, including those
with sudden death with concurrent COVID-19
infection, were also captured. A total of 90 patients
from our cohort died of COVID-19. Similar to
deaths reported for the whole population during
a similar period,1 over 60% of deaths in dialysis or
kidney transplant patients occurred in unvaccinated
persons. An imbalance of unvaccinated patients was
noted for those on peritoneal dialysis, representing
73% of those on peritoneal dialysis who succumbed
to COVID-19. As shown in the Table, the peritoneal
dialysis and haemodialysis populations had similarly
high mortality attributable to COVID-19, with
19.4 and 21.9 deaths per 1000 dialysis population,
respectively.
Our results contrast with the previous
observation of strikingly lower COVID-19 cases and
deaths per population in Asian countries.4 Although
we cannot exclude confounding factors such as
frailty and age, the results of a high mortality burden
among peritoneal dialysis patients should caution
nephrologists who give advice about vaccination
of dialysis patients. It should be emphasised that a
perceived lower risk of infection might have caused
a more relaxed attitude among peritoneal dialysis
patients. Potential explanations for the relatively high
mortality in the peritoneal dialysis cohort are lower
adherence to hand hygiene, mask wearing, social
distancing, and most significantly, vaccine uptake.
The observation of lower vaccine coverage among
death cases in peritoneal dialysis patients supports
the hypothesis although we did not have population-level
data of vaccination coverage among all dialysis
patients. Our findings are therefore important for patient information and COVID-19 infection preparedness in the nephrology community.
Author contributions
Concept or design: All authors.
Acquisition of data: KM Chow, JYH Chan, SSH Wong, SK Yuen, PN Wong.
Analysis or interpretation of data: KM Chow, YL Cheng, CC Szeto.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: KM Chow, YL Cheng, CC Szeto.
Acquisition of data: KM Chow, JYH Chan, SSH Wong, SK Yuen, PN Wong.
Analysis or interpretation of data: KM Chow, YL Cheng, CC Szeto.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: KM Chow, YL Cheng, CC Szeto.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The study adhered to the tenets of the Declaration of Helsinki.
References
1. Smith DJ, Hakim AJ, Leung GM, et al. COVID-19 mortality and vaccine coverage–Hong Kong Special Administrative
Region, China, January 6, 2022-March 21, 2022. MMWR
Morb Mortal Wkly Rep 2022;71:545-8. Crossref
2. Corbett RW, Blakey S, Nitsch D, et al. Epidemiology of COVID-19 in an urban dialysis center. J Am Soc Nephrol 2020;31:1815-23. Crossref
3. Yau K, Muller MP, Lin M, et al. COVID-19 outbreak in an urban hemodialysis unit. Am J Kidney Dis 2020;76:690-5.e1. Crossref
4. Robinson BM, Guedes M, Alghonaim M, et al. Worldwide early impact of COVID-19 on dialysis patients and staff
and lessons learned: a DOPPS roundtable discussion.
Kidney Med 2021;3:619-34. Crossref
5. Hsu CM, Weiner DE, Aweh G, Salenger P, Johnson DS,
Lacson E Jr. Epidemiology and outcomes of COVID-19 in
home dialysis patients compared with in-center dialysis
patients. J Am Soc Nephrol 2021;32:1569-73. Crossref
6. Griffith GJ, Morris TT, Tudball MJ, et al. Collider bias
undermines our understanding of COVID-19 disease risk
and severity. Nat Commun 2020;11:5749. Crossref
7. Mahalingasivam V, Su G, Iwagami M, Davids MR,
Wetmore JB, Nitsch D. COVID-19 and kidney disease:
insights from epidemiology to inform clinical practice. Nat
Rev Nephrol 2022;18:485-98. Crossref
8. International Statistical Classification of Diseases,
World Health Organization. International guidelines for
certification and classification (coding) of COVID-19
as a cause of death. Available from: https://cdn.who.int/media/docs/default-source/classification/icd/covid-19/guidelines-cause-of-death-covid-19-20200420-en.pdf. Accessed 1 May 2022.