Hong Kong Med J 2022 Dec;28(6):494–5.e1-3
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
A critically ill infant with multi-organ dysfunction due to eczema
KL Hon, MB, BS, MD1; Karen KY Leung, MB, BS, MRCPCH1; WL Lin, PhD, BChinMed2; David CK Luk, MB, ChB, MRCPCH3
1 Department of Paediatrics and Adolescent Medicine, Hong Kong Children’s Hospital, Hong Kong
2 Hong Kong Institute of Integrative Medicine, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong
3 Department of Paediatrics and Adolescent Medicine, United Christian Hospital, Hong Kong
Corresponding author: Dr KL Hon (ehon@hotmail.com)
Eczema is the most prevalent childhood atopic
illness routinely encountered by health professionals
providing care to children.1 Some infants become
critically ill and present to the paediatric intensive
care unit (PICU) with this seemingly trivial
condition.2 This anonymised (no clinical and
laboratory data are presented) case of severe eczema
and multi-organ dysfunction illustrates the extent of multi-organ involvement in eczema and the medical
and psychosocial issues associated with the disease.1 3
A 6-month-old boy with eczema and septic
shock presented to the emergency department. He
was treated with fluid resuscitation and subsequently
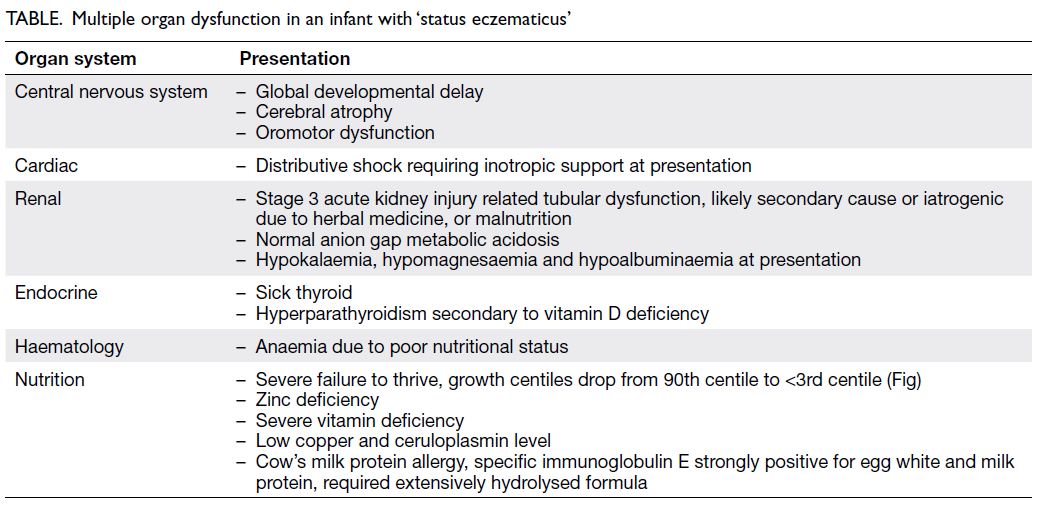
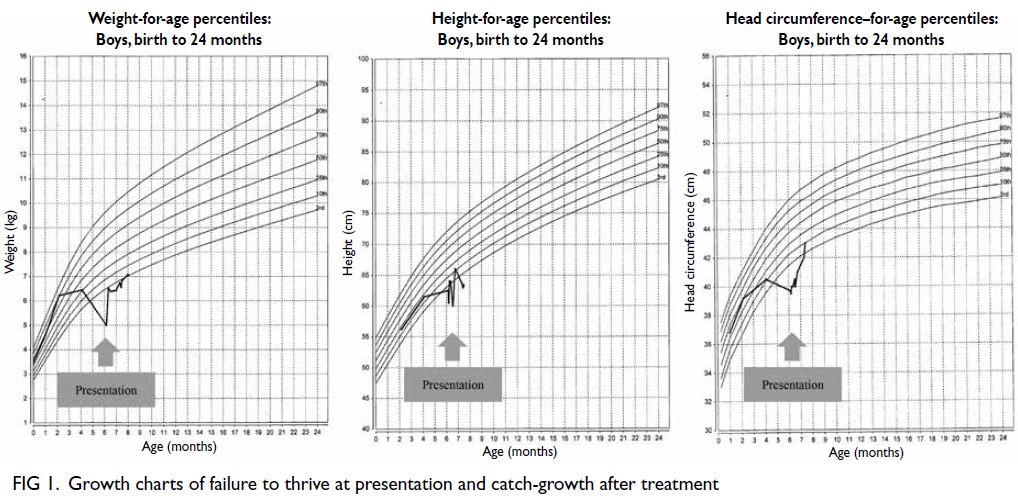
admitted to a PICU. Derangement of multiple
organ functions were identified along with failure to
thrive and poor development (Table, Figs 1 and 2). Dobutamine and broad-spectrum antibiotics were
prescribed. Although his condition improved
rapidly, it became apparent that his parents did
not trust Western medicine and were reluctant to
use emollient and topical steroid to manage their
child’s eczema. The mother frankly admitted that
since the development of eczema at 2 months of
age, she had been giving the infant complementary
herbal medicine remedies. She was also taking
herbal medicine whilst breastfeeding so that her
child would indirectly receive the more ‘effective’
herbal medicine. The parents were interviewed by
healthcare workers from various disciplines but they
remained resolute in their beliefs and phobias about Western medicine. The child was discharged from
PICU after the acute medical issues were resolved.
Extensive investigations have been performed
and apart from persistent peripheral eosinophilia,
slightly low immunoglobulin M level, borderline
CD4:CD8 ratio and borderline low zinc level, all
other investigations including metabolic workup
remain unremarkable to date. Further paediatric
dermatology, genetics and integrative medicine
follow-ups have been arranged.
Our reported case is probably the youngest
patient with critical ‘status eczematicus’ to survive.
All growth parameters were compromised (Fig 1).
Children with severe eczema rarely require admission
to an ICU and there are very few such cases in the
literature. Mortality due to eczema is rare, but we
have previously reported a tragic case of an infant
with eczema who died of group B streptococcus
septicaemia and malnutrition despite expensive
dietary supplements.2 Eczema is a chronic condition
that can significantly affect a child’s quality of life as
well as that of their family if it is not well controlled
due to the potentially significant psychological toll.4
Although ICU is not an ideal setting to manage a
family with multiple phobias, the child must first be
stabilised, and other differential diagnoses of acute
skin failure ruled out.2
Acute treatment of eczema is straightforward
but long-term maintenance treatment is always
challenging. Topical medications should be
considered to prevent exacerbations and therapy
should be proactive. Steroid phobia is prevalent and
often leads to non-compliance.1
Recommendations about dietary avoidance
should be specific and given only in confirmed
cases of food allergy.1 The use of traditional and
proprietary topical and herbal medicine is popular
across many countries in Asia.1 Anxious food-avoiding
parents may purchase multi-vitamin
supplements, prebiotics, probiotic or symbiotics
that claim to be effective. In an extreme case, death
was reported to have a secondary association with
extreme dietary practice.3 Physicians must be tactful
when counselling these anxious parents who are
steroid phobic and mistrusting of modern medicine.
Indirect administration of herbal medicine to an
infant through breastfeeding is not advocated even
in the practice of integration medicine.
Management of eczema can sometimes be
challenging. Apart from strong parental beliefs,
cultural differences might also play a role in
compliance with a prescribed treatment plan or
a tendency to seek alternative therapies instead.
These effects are likely to be underestimated in
our community, especially in the primary care
setting where consultation time might be limited.
Physicians should endeavour to spend more time
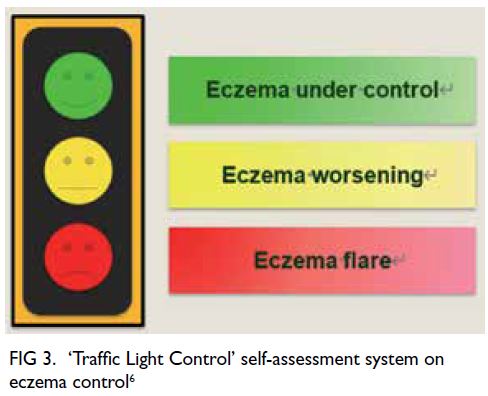
exploring parental beliefs. A practical solution may be to use an objective self/parental assessment to
aid eczema control assessment, eg, ‘Traffic Light
Control’ self-assessment system (Fig 3) and quality
of life assessment, eg, Children’s Dermatology Life
Quality Index.5 An ‘eczema action plan’ can also be
given to parents to remind them of the prescribed
eczema treatment. The treatment plan should be
straightforward and easy to follow, especially if
they perceive a worsening of eczema between clinic
visits.5 A multidisciplinary and perhaps integrative
medicine approach should be adopted where possible
to manage patients and families with eczema, and
education about the disease should be individualised
to improve patient outcomes.
Healthcare providers must be aware of the
mortality and morbidity associated with recalcitrant
eczema and ‘status eczematicus’. These tragic cases
of ‘status eczematicus’ serve to remind us of the
grave consequences if eczema is inappropriately
managed.
Author contributions
All authors contributed to the concept or design, acquisition of data, analysis or interpretation of data, drafting of the
manuscript, and critical revision of the manuscript for
important intellectual content.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
As an editor of the journal, KL Hon was not involved in the peer review process. Other authors have disclosed no conflicts
of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patient was treated in accordance with the tenets of the
Declaration of Helsinki. Ethics approval for publication of
patient information in the paediatric intensive care unit was
obtained from the Hong Kong Children’s Hospital Research
Ethics Committee (Ref No.: HKCH-REC-2019–0011).
References
1. Hon KL, Leong KF, Leung TN, Leung AK. Dismissing
the fallacies of childhood eczema management: Case
scenarios and an overview of best practices. Drugs
Context 2018;7:212547. Crossref
2. Hon KL, Nip SY, Cheung KL. A tragic case of atopic
eczema: malnutrition and infections despite multivitamins
and supplements. Iran J Allergy Asthma Immunol
2012;11:267-70.
3. Hon KL, Kam WY, Leung TF, et al. Steroid fears in children with eczema. Acta Paediatr 2006;95:1451-5. Crossref
4. Hon KL, Kung JS, Wang M, Pong NH, Li AM, Leung TF.
Clinical scores of sleep loss and itch, and antihistamine
and topical corticosteroid usage for childhood eczema. Br
J Dermatol 2016;175:1076-8. Crossref
5. Lam PH, Hon KL, Leung KK, Leong KF, Li CK, Leung TF. Self-perceived disease control in childhood eczema. J
Dermatolog Treat 2022;33:1459-646. Crossref