Hong Kong Med J 2022 Aug;28(4):306–14 | Epub 8 Aug 2022
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE (Healthcare in Mainland China)
Utilisation of village clinics in Southwest China:
evidence from Yunnan Province
Y Shi, PhD1; S Song, MA1; L Peng, MA1; J Nie, PhD1; Q Gao, PhD1; H Shi, PhD2; DE Teuwen, MD3; H Yi, PhD4,5
1 Center for Experimental Economics in Education, Shaanxi Normal University, Xi’an, China
2 Business Department Center of Red Cross Society of China, Beijing, China
3 Ghent University Hospital, Department of Neurology, Ghent, Belgium
4 China Center for Agricultural Policy, School of Advanced Agricultural Sciences, Peking University, Beijing, China
5 Institute for Global Health and Development, Peking University, Beijing, China
Corresponding author: Dr Q Gao (gqiufeng820@163.com)
Abstract
Introduction: Primary healthcare in rural China
is underutilised, especially in village clinics in
Southwest China. The aim of this study was to
explore any relationships among the ethnicity of
the healthcare provider, the clinical competence of
the healthcare provider, and the utilisation of village
clinics in Southwest China.
Methods: This cross-sectional survey study
involved 330 village healthcare providers from three
prefectures in Yunnan Province in 2017. Multiple
logistic regressions were adopted to investigate the
utilisation of primary healthcare among different
ethnic healthcare providers.
Results: Primary healthcare utilisation was higher in
village clinics where healthcare providers were Han
Chinese than those where healthcare providers were
ethnic minority (151 vs 101, P=0.008). The logistic
regression analysis showed that clinical competence
was positively associated with the utilisation
of primary healthcare (odds ratio [OR]=1.49,
95% confidence interval [CI]=1.12-2.00; P=0.007)
and that inadequate clinical competence of ethnic
minority health workers may lead to a lag in
the utilisation of primary healthcare (OR=0.45,
95% CI=0.23-0.89; P=0.022).
Conclusion: Our results confirm differences in the utilisation of primary healthcare in rural Yunnan Province among healthcare providers of different
ethnicities. Appropriate enhancements of clinical
competence could be conducive to improving the
utilisation of primary healthcare, especially among
ethnic minority healthcare providers.
New knowledge added by this study
- The results of our study confirmed that differences exist in the utilisation of primary healthcare in rural Yunnan Province among different ethnic minority healthcare providers.
- Significant differences in clinical competence were observed between ethnic minority and Han Chinese majority healthcare providers.
- The underdeveloped clinical competence of ethnic minority healthcare providers likely contributes to the difference in utilisation of village clinics.
- Proper enhancements for ethnic minority providers could be conducive to improving their clinical competence.
- More involvement from the government and adequate in-service training for ethnic minority healthcare providers could help improve the utilisation of primary healthcare.
Introduction
For rural residents, who account for approximately
41% of China’s population, primary healthcare is
the main source of medical care.1 To meet their
healthcare needs, China promoted a tiered medical
system in 2015 to encourage people to fully utilise
primary healthcare.2 3 Nevertheless, while the government invests various resources, primary
healthcare in rural areas remains underused.4 5 6
From 2015 to 2018, the total number of out-patient
visits in rural primary healthcare institutions
decreased from 2.90 billion to 2.70 billion, while the
number of hospital visits increased from 3.10 billion
to 3.60 billion.7
Disparity exists in the utilisation of primary
healthcare across different regions of China.
Compared with rural residents in eastern China,
the utilisation of primary healthcare among those in
western China is relatively low.8 9 The lack of medical
resources and sparseness of the land in western
China contributes to the inconvenience of accessing
primary healthcare among rural residents.10 11 12 In
addition to the difference between eastern and
western China, differences in the utilisation of
primary healthcare exists among the provinces
in western China.11 Although many studies have
reported on the utilisation of primary healthcare
in Southwest China, most have focused on the
perspective of rural residents while neglecting the
importance of providers, who play important
roles in primary healthcare.3 4 Therefore, research
concerning village healthcare providers in Southwest
China could be conducive to understanding the
utilisation of primary healthcare.
Southwest China is home to more ethnic
minority village healthcare providers than other
areas in China.11 To investigate village healthcare
providers in Southwest China, the ethnicity of
providers, which may be linked to the utilisation
of healthcare, is a factor that cannot be ignored.
Previous studies have illustrated that ethnic minority
providers are more likely to attract patients from the
same ethnicity, and this finding has been attributed
to the patients’ preference instead of the capability of
minority providers.13 14 Existing studies were mainly conducted outside China or were related to providers
who performed traditional Chinese medicine.13 14 15
Therefore, knowledge regarding whether differences
exist in the utilisation of primary healthcare among
Chinese ethnic minority providers and Han Chinese
majority providers is limited.
Clinical competence may influence the
utilisation of healthcare and serves as a practical
way to measure a doctor’s working performance
and quality.16 17 Some studies in China have shown
that the ethnicity of medical students might be
related to their future clinical competence.18 19 20 21 22
Studies conducted in Southwest China confirmed
the underdeveloped clinical competence of village
providers, but most studies failed to distinguish the
ethnicity of the healthcare providers.23 24 25 26 Whether
ethnic minority healthcare providers in rural areas
of China have underdeveloped clinical competence
remains unclear.
Considering the above, the purpose of the
present study was to investigate the utilisation of
primary healthcare in western China. In particular,
the aims were to clarify whether the ethnicity of
healthcare providers affects utilisation of primary
healthcare; whether there are differences in clinical
competence among different ethnic groups; and
whether clinical competence of healthcare providers
affects utilisation of primary healthcare.
Methods
Study design, setting and sampling method
This study was a cross-sectional survey conducted
in three prefectures (ie, prefecture-level cities) in
Yunnan Province, an economically developing area
in Southwest China. In 2017, the per capita gross
domestic product in Yunnan Province was US$5068,
which is lower than the national average (US$8777).27
The total population in Yunnan Province was
47.71 million, and the proportion of the rural
population in Yunnan Province was 53.31%, which
is much higher than the overall proportion of rural
population in China (41.48%).27 The three prefectures
included in our study have a total rural population of
6.50 million, accounting for 20.00% of the total rural
population in Yunnan Province.
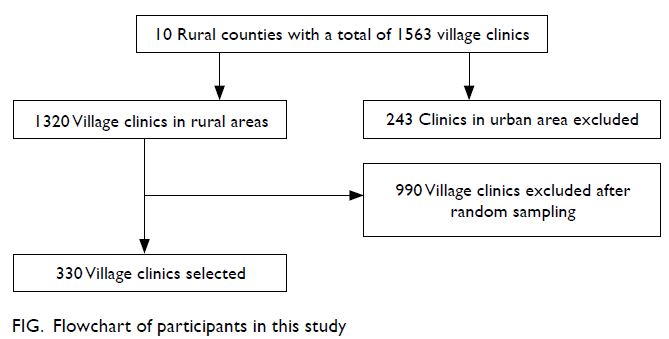
To investigate the utilisation of primary
healthcare in rural China, we conducted a cross-sectional
study in 330 village clinics (VCs),
representing the first tiers of China’s three-tiered
rural health system.4 In summary, we selected a
random sample of 330 healthcare providers from
three prefectures in three steps (Fig). First, we
selected 10 counties (in three prefectures) at random,
after excluding three urban counties and 13 counties
with a minority population greater than 20%. Second,
we used probability proportional to size sampling to
randomly select 330 VCs proportional to the number of VCs in each county. Finally, we asked each clinic
to list all staff serving in the clinic and describe their
responsibilities. Considering the measurement of
different types of medical practitioners, we excluded
healthcare providers other than Western medicine
practitioners (ie, traditional Chinese medicine
practitioners or those responsible for public health
services only). Then, we randomly selected one of
the remaining village healthcare providers as our
sample.
Data collection
The data collection was carried out in July 2017 by trained investigators. The survey consisted of a
clinic form administered to the head of the VC and
a clinician form administered to providers in each
clinic verbally.
The clinic form (Supplementary Table 1)
was used to collect basic information regarding the
VCs, including the number of equipment per clinic,
whether the drugs sold by the clinics met the zero
price difference of medicine (a policy requires no
mark-ups above the cost of drugs),6 the number of
clinics within 5 km, the number of out-patient visits
per clinic, and the number of providers per clinic.
The clinician form (Supplementary Table 2) consisted of two parts. The first part was
used to obtain information regarding the provider’s
demographics, working time allocation and
income. This part included age, sex, ethnicity, basic
salary, local residence (whether he/she was born
and raised in the sample village), and time spent
performing public health services. The second part
was used to obtain detailed information on the
providers’ in-service training participation in 2016
(the year before the survey year) and their clinical
competence, including education level, certificate in
rural medicine or higher, length of experience, and
medical study.
Assessment of the utilisation of village clinics
The primary healthcare system provides generalist clinical care and basic public health services.1 China
has promoted the three-tiered healthcare system
to improve the use of primary healthcare. In rural
China, the three-tiered healthcare system consists of
VCs, township health centres, and county hospitals.
Township health centres and VCs play a role in
primary healthcare, and VCs mainly provide out-patient
services under common clinical conditions.
To assess the utilisation of VCs, the investigators
asked the heads of the VCs to estimate (on average)
the total number of out-patient visits during the
previous month. The utilisation of the VCs was
calculated using data related to the total number
of out-patient visits, intramuscular injection visits,
intravenous infusion visits, and number of healthcare providers in the clinics. Specifically, the utilisation of
VCs in our research is measured on a per-provider
basis. Thus, the utilisation of VCs equals the total
number of out-patient visits divided by the number
of healthcare providers.
Measurement of the providers’ clinical
competence
Providers’ clinical competence is the quality
of healthcare providers pertaining to medical
knowledge, treatment quality, medical experience,
medical study background, and medical training.28
In our study, we evaluated the providers’ clinical
competence in the following dimensions: education
above college level (measured medical knowledge);
attainment of certificates in rural medicine or higher
(measured treatment quality); length of experience
(measured medical experience); participation
in medical studies (measured medical study
background); and completion of in-service training
(measured medical training).
In clinical competence, multiple characteristics
are often correlated; multicollinearity is a limitation
of applying a multiple logistic regression analysis
to measure clinical competence. A principal
component analysis is often used to address this issue
by transforming the data into one or two dimensions
that serve as a summary of the characteristics, such
as constructing an index.29 Therefore, we constructed
the Clinical Competence Index to assess the overall
clinical competence of the providers using a principal
component analysis approach.
Statistical methods
To explore the relationships between the healthcare providers and the utilisation of VCs, we used a
multiple logistic regression. We conducted three
types of regressions, and the outcome variable was
out-patient visits per doctor. In the first regression,
we measured the relationship between the village
providers’ ethnicity and the utilisation of VCs. In the second regression, we included only the variables
measuring the providers’ clinical competence. This
relationship might vary across different ethnicities,
and a heterogeneity analysis is needed. In the third
regression, we performed a heterogeneity analysis by
including the interaction term ‘Clinical Competence
Index ethnic minority providers’ to measure the
providers’ clinical competence and its relationship
with the utilisation of VCs across different ethnicities.
In each regression mentioned above, we
assessed the correlations with a fixed set of facility-level
and provider-level characteristics. These
characteristics included the number of equipment
per clinic, whether the drugs sold by the clinics met
the zero price difference of medicine, the number
of clinics within 5 km, the percentage of minority
residents in the town, the providers’ sex, salary,
local residency, and time spent providing public
health services. Notably, in all regressions, we also
controlled for county-fixed effects.
All statistical analyses were performed using
Stata version 15.0 statistical software (Stata Corp,
College Station [TX], United States). The results
with a P value <0.05 were considered statistically
significant.
Results
Characteristics and the utilisation of village
clinics
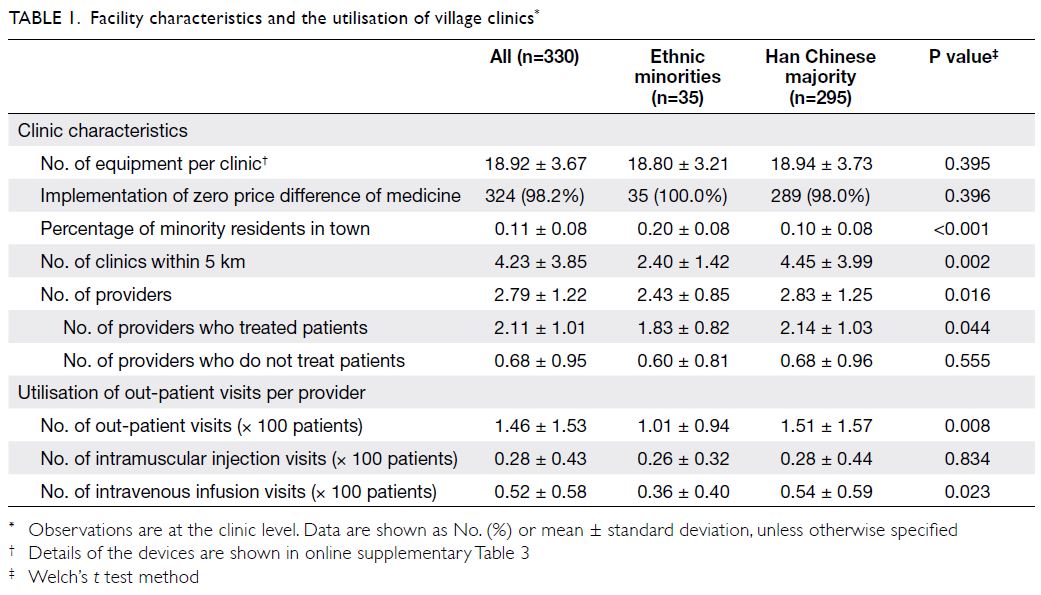
The questionnaire surveys were sent to 330 VCs
and 330 healthcare providers, and valid results
were obtained from all (participation rate 100%).
There were no significant differences in terms of the amount of clinic equipment (P=0.395) and
the implementation of the zero price difference
of medicine (P=0.396) among the VCs (Table 1).
However, the proportion of minority residents in
the towns significantly differed with type of VCs
(P<0.001). We also found that VCs where Han
Chinese providers worked faced more competition,
as the number of clinics within 5 km of these clinics
was significantly higher than that for clinics where
ethnic minority providers worked (P=0.002). The
average number of healthcare providers in the VCs
was 2.79. There was a significant difference in the
number of providers across clinics (P=0.016), and
this difference was mainly due to the number of
providers who treat patients (P=0.044). Among the
330 VCs, mean number of out-patient visits per
doctor was 146. The results indicate that the Han
Chinese providers conducted a significantly higher
average number of out-patient visits than the ethnic
minority providers (151 vs 101; P=0.008) [Table 1].
In addition, we documented intramuscular injection
visits and intravenous infusion visits. There was also
a significant difference between the ethnic minority
and Han Chinese majority providers in intravenous
infusion visits (P=0.023), but no significant
difference was found in intramuscular injection
visits (P=0.834).
Characteristics of the providers and their
clinical competence
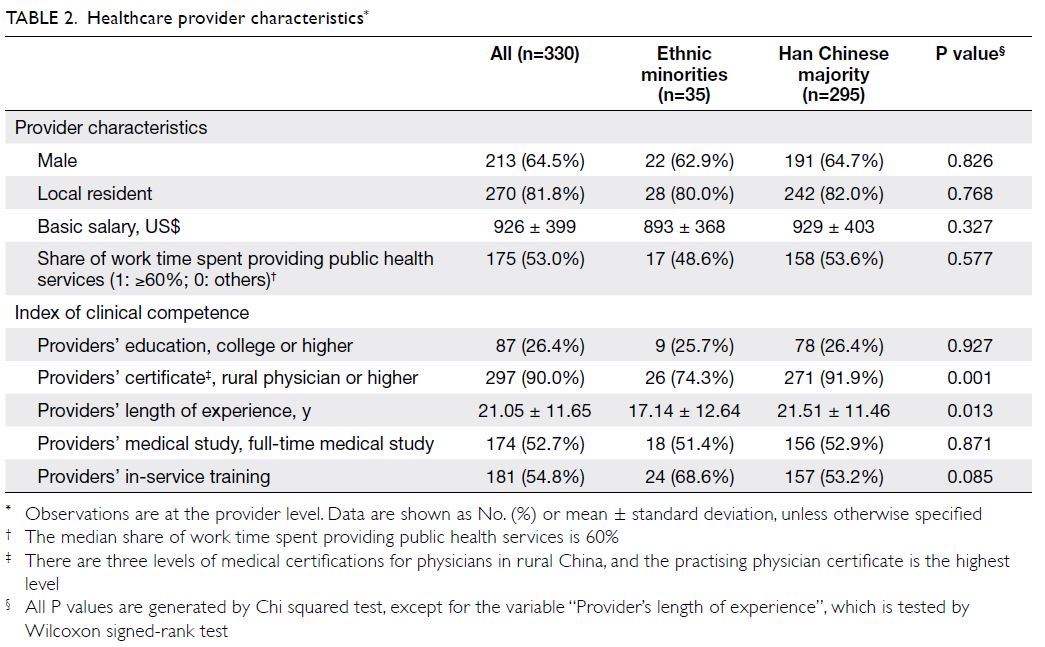
Most healthcare providers were male (64.5%), and 81.8% of providers were local residents (Table 2).
The mean ± standard deviation annual salary of
all providers was US$926±399, with no significant difference between the ethnic minority and Han
Chinese majority providers (P=0.327). More than
half of the healthcare providers devoted close to
60% of their work time to providing public health
services (P=0.577).
Among the 330 providers, 26.4% had a college
degree or higher, and the proportion among the Han
Chinese providers was similar to that (26.4%) among
the ethnic minority providers (25.7%, P=0.927)
[Table 2]. In total, 91.9% of the Han Chinese
providers were confirmed to have at least certificates
in rural medicine; however, the proportion was 74.3%
among the ethnic minority providers (P=0.001).
In addition, the length of experience of the Han
Chinese providers was significantly higher than
that of the ethnic minority providers (P=0.013). The
proportion of full-time medical studies conducted
by all providers was 52.7%, and more ethnic minority
providers than Han Chinese providers received in-service
medical training (P=0.085).
Determinants of the utilisation of village
clinics
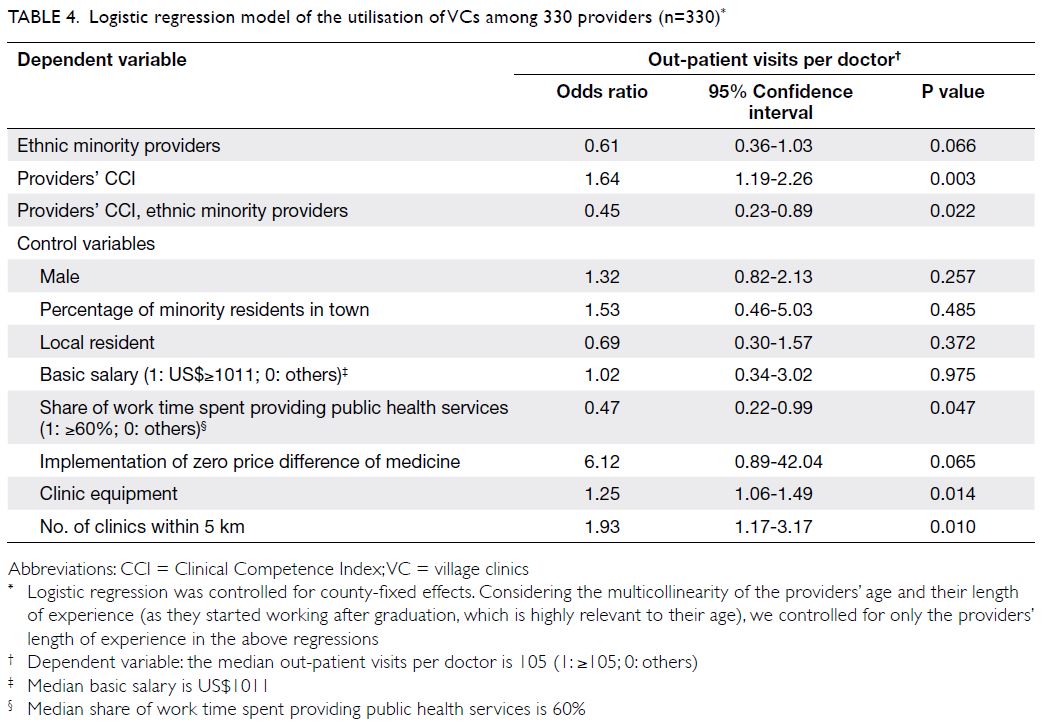
The ethnicity of the providers was negatively
associated with the utilisation of VCs (odds ratio
[OR]=0.53, 95% confidence interval [CI]=0.29-0.96;
P=0.037) [Table 3]; the providers’ clinical competence
was positively associated with the utilisation of VCs
(OR=1.49, 95% CI=1.12-2.00; P=0.007) [Table 3]. To
better examine this relationship, we performed a
heterogeneity analysis (Table 4). The results suggest that ethnic minority providers were likely to have
underdeveloped clinical competence, which could
further limit the utilisation of VCs (OR=0.45, 95%
CI=0.23-0.89; P=0.022) [Table 4]. We also measured
the determinants of intravenous infusion visits,
and the results suggest that the providers’ clinical
competence (OR=1.43, 95% CI=1.16-1.77; P=0.001)
[Supplementary Table 4] was associated with
the utilisation of VCs.
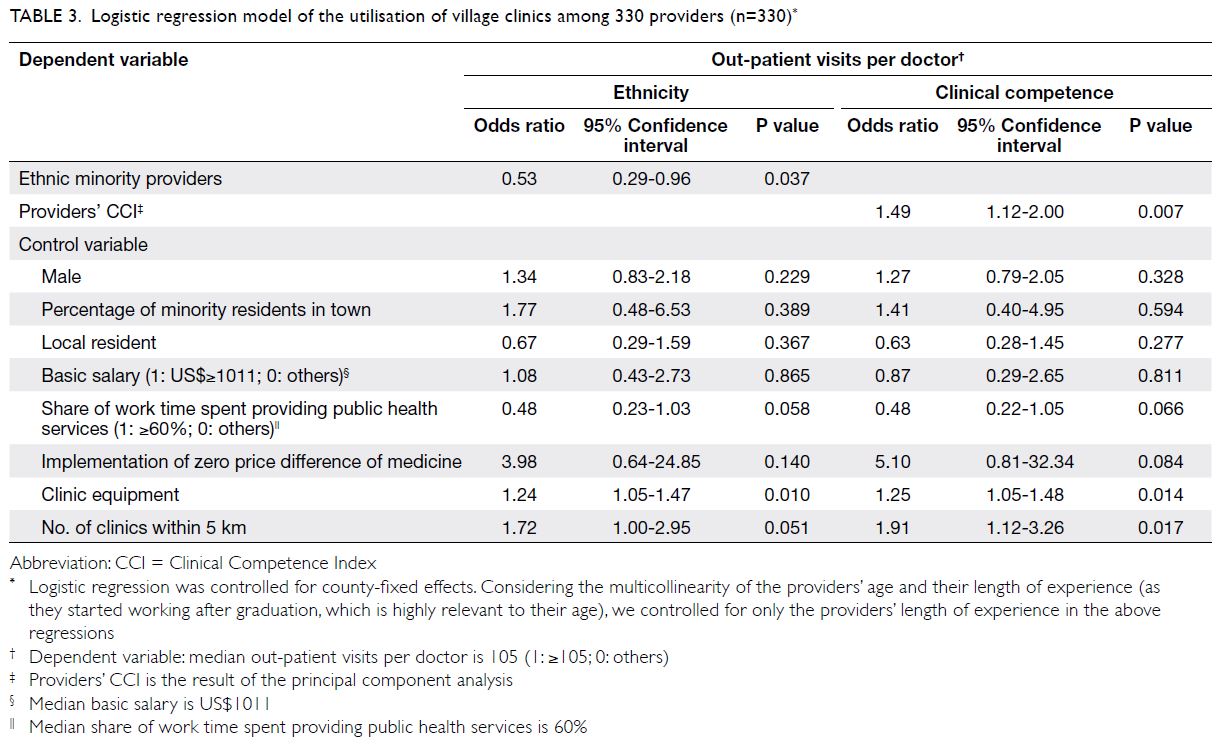
Table 3. Logistic regression model of the utilisation of village clinics among 330 providers (n=330)
Discussion
The data enabled an analysis of the utilisation of
primary healthcare in rural areas in Southwest
China. In general, there are three key findings in
this study. First, we found significant differences
between Han Chinese and ethnic minority providers
in the utilisation of VCs. Second, compared with
Han Chinese providers, ethnic minority providers in
our sample had poorer clinical competence in two
dimensions (possession of rural physician certificate
or length of experience). Finally, our results indicate
that underdeveloped clinical competence is a factor
responsible for the lower utilisation of VCs among
ethnic minority providers.
Our survey data show that the average number
of out-patient visits in the sampling VCs is 146 per
month per doctor, which is lower than the number of
out-patient visits in eastern China (188 per month per
doctor, 2017).9 Consistent with previous studies, we
believe that the inconvenience of accessing primary
healthcare among rural residents contributes to this difference.23 Compared with Yunnan Province
(116 per month per doctor, 2017), the utilisation
of VCs in the sampling area was higher.9 Based on
our investigation, the high utilisation of VCs in
the sampling area could be explained by both the
population density and local economic development.
According to the China Statistical Yearbook, the
rural residents in the three prefectures we studied
accounted for 20.00% of the total rural residents in
Yunnan Province, which is quite large compared
with the rate in other regions.30 The gross domestic
product of the sampling area is also relatively high in
Yunnan Province.27
However, the number of out-patient visits to
VCs where the main providers are ethnic minorities
is significantly lower than that of VCs where the main
providers are Han Chinese individuals. Previous
studies have shown that patients visiting providers of
their own race were more satisfied and deliberately
chose providers of their own race because of personal
preference and language issues.13 14 In contrast
to these studies, we excluded the preference and
language issues of patients. First, their studies were
generally conducted in large hospitals with many
providers, but the average number of providers in
our sampled VCs was approximately two, limiting the
patients’ choices. Second, regarding language, most
(81.8%) providers in our study were local residents
who were fluent in the local dialect. These providers
rarely have communication problems with their
patients. After the above exclusions, an investigation
of the characteristics of different ethnic providers
was performed. Consistent with previous studies,
there was no significant difference in provider
characteristics and income, and the amount of
clinic equipment and implementation of zero price
difference of the medicine did not differ.19 20
Furthermore, we find significant differences
between ethnic minority and Han Chinese village
providers in their clinical competence. As a crucial
aspect of primary healthcare services in rural China,
village providers are obligated to provide qualified
medical services, which require abundant clinical
competence.31 32 However, based on our evidence,
even if rural patients in Southwest China were asked
to follow the instructions of policymakers and seek
care primarily in VCs, they would visit higher-level
facilities with a relatively high cost considering the
local providers’ poor clinical competence. In fact,
this type of situation is already very common in rural
China.3 16 25
Under such circumstances, our findings imply
that the difference in the utilisation of VCs might be
related to ethnic minority providers’ underdeveloped
clinical competence. Despite the small number of
previous studies, the current evidence is consistent
with the main findings.1 24 On the one hand, early
studies suggested that the quality of health providers limited the utilisation of primary healthcare.3 4 16 On
the other hand, ethnic minority providers usually
experience less supportive learning environments
during their medical studies, which might help
explain the lag in their clinical competence.33 34 35
Therefore, we believe that uniformly improving the
clinical competence of village providers, especially
that of ethnic minority village providers, is conducive
to improving the utilisation of primary healthcare.1 36
The Government of the People’s Republic of
China understands the benefits of improving the
clinical competence of village providers. A series of
human resource policies for health launched in 2010
had a positive impact in rural China.37 Among these
policies, the encouragement of external training
for healthcare providers has been proven effective
and necessary.36 38 39 In-service training for village
providers could help these providers be informed of
the latest knowledge and skills to manage diseases,
which could significantly improve the quality of their
medical services.36 The government has implemented
actions to encourage the training of ethnic minorities
since 2009.40 Thus, the appropriate introduction of
re-education and more medical training should be
adopted among ethnic minority providers.
Considering previous studies with analyses
based mainly on the utilisation of healthcare from
the patient perspective, our study might be the
first investigation to examine healthcare providers’
ethnicity and clinical competence.10 11 32 In addition,
our quantitative data include a rich set of detailed
information of VCs regarding out-patient visits
and providers’ clinical competence. We hope that
our findings offer key insights into the utilisation of
primary healthcare in rural China.
Our study has two main limitations. First, the
participants in this study were recruited from rural
Southwest China, so unavoidably, the nationwide
validity of our findings is limited. Second, the results
were limited by the cross-sectional nature of the
study, and no causal effect between the providers’
clinical competence and the utilisation of primary
healthcare was detected. Future research could
investigate how different ethnic providers influence
the utilisation of VCs and seek to adopt multiple
measures to reduce bias in investigations.
Conclusions
In conclusion, this study reveals differences in the utilisation of primary healthcare between ethnic
minority providers and Han Chinese providers at
VCs in rural areas in Southwest China. Notably, the
results indicate that higher clinical competence is
more likely to drive the utilisation of VCs. We believe
that the results of this study provide compelling
evidence that ethnic minority healthcare providers
in Southwest China require further enhancement
with respect to their clinical competence.
Author contributions
Concept or design: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
As an adviser of the journal, Y Shi was not involved in the peer review process. Other authors have disclosed no conflicts of interest.
Funding/support
H Yi received funding for this study from the Health and Hope
Fund of the Business Development Center of the Red Cross
Society of China and UCB of Belgium. Y Shi received funding
from 111 Project (Grant number B16031), and Q Gao received
funding from Innovation Capability Support Program of
Shaanxi (Grant number 2022KRM007). The funders had no
role in study design, data collection/analysis/interpretation,
or manuscript preparation.
Ethics approval
The study was approved by the Peking University Institutional
Review Board (Ref IRB 00001052-17033). The board approved
the verbal consent procedure. Informed consent from all
respondents as a requirement for completing the survey.
References
1. Li X, Lu J, Hu S, et al. The primary health-care system in
China. Lancet 2017;390:2584-94. Crossref
2. Liu Q, Wang B, Kong Y, Cheng KK. China’s primary healthcare
reform. Lancet 2011;377:2064-6. Crossref
3. Li YN, Nong D, Wei B, Feng QM, Luo HY. The impact of
predisposing, enabling, and need factors in utilization of
health services among rural residents in Guangxi, China.
BMC Health Serv Res 2016;16:592. Crossref
4. Sylvia S, Xue H, Zhou C, et al. Tuberculosis detection
and the challenges of integrated care in rural China: A
cross-sectional standardized patient study. PLoS Med
2017;14:e1002405. Crossref
5. Dong X, Liu L, Cao S, et al. Focus on vulnerable populations
and promoting equity in health service utilization—an
analysis of visitor characteristics and service utilization of
the Chinese community health service. BMC public health
2014;14:503. Crossref
6. Li Z. Healthcare reform and the development of China’s
rural healthcare: a decade’s experience [in Chinese].
Chinese Rural Economy 2019;9:1-22.
7. National Bureau of Statistics of China, PRC Government.
China Statistical Yearbook 2019. Available from: http://www.stats.gov.cn/tjsj/ndsj/2019/indexch.htm. Accessed 20
Oct 2020.
8. Sun J, Luo H. Evaluation on equality and efficiency of
health resources allocation and health services utilization
in China. Int J Equity Health 2017;16:127. Crossref
9. China Statisitcs Press. China Health Statistical Yearbook
2018. Available from: https://data.cnki.net/area/Yearbook/Single/N2019030282?z=D09. Accessed 9 May 2020.
10. Zhang X, Wu Q, Shao Y, Fu W, Liu G, Coyte PC. Socioeconomic inequities in health care utilization in
China. Asia Pac J Public Health 2015;27:429-38. Crossref
11. Wang M, Fang H, Bishwajit G, Xiang Y, Fu H, Feng Z.
Evaluation of rural primary health care in Western China:
a cross-sectional study. Int J Environ Res Public Health
2015;12:13843-60. Crossref
12. Shi Y, Xue H, Wang H, Sylvia S, Medina A, Rozelle S.
Measuring the quality of doctors’ health care in rural
China: an empirical research using standardized patients
[in Chinese]. Studies in Labor Econ 2016;4:48-71.
13. van Zanten M, Boulet JR, McKinley DW. The influence of
ethnicity on patient satisfaction in a standardized patient
assessment. Acad Med 2004;79(10 Suppl):S15-7. Crossref
14. LaVeist TA, Nuru-Jeter A, Jones KE. The association of
doctor-patient race concordance with health services
utilization. J Public Health Policy 2003;24:312-23. Crossref
15. Li Z, Li Y, Cui J. Development history of Chinese minority
traditional medicine [in Chinese]. Med Philosophy
(Humanistic & Soc Med Ed) 2011;32:78-81.
16. Wu D, Lam TP. Underuse of primary care in China: the scale, causes, and solutions. J Am Board Fam Med
2016;29:240-7. Crossref
17. Sandberg J. Understanding human competence at work: an interpretative approach. Acad Manage J 2000;43:9-25. Crossref
18. Liu W, Ding Y, Yang X. The determinants of rural labor migration in minority regions [in Chinese]. Population J 2015;37:102-12.
19. Shi L, Sai D. An empirical analysis of income inequality
between a minority and the majority in urban China: the
case of Ningxia Hui Autonomous Region. Rev Black Polit
Econ 2013;40:341-55. Crossref
20. Li L, Li XG. Ethnicity, social capital and income gap: a
comparative study of the Northwest ethnic group and
the Western Han nationality [in Chinese]. J Sun Yat-sen
University (Social Science Edition) 2016;56:161-71.
21. Gustafsson B, Sai D. Temporary and persistent poverty
among ethnic minorities and the majority in rural China.
Rev Income Wealth 2009;55:588-606. Crossref
22. China National Knowledge Infrastructure. BMJ;
Why are ethnic minority doctors less successful
than white doctors? Available from: https://schlr.cnki.net/en/Detail/index/SPQDLAST/SPQD48BA99708EE31C6710E1A02B2C34186A. Accessed 12 Jun 2020.
23. Li Y, Chi I, Zhang K, Guo P. Comparison of health services
use by Chinese urban and rural older adults in Yunnan
province. Geriatr Gerontol Int 2006;6:260-9. Crossref
24. Anand S, Fan VY, Zhang J, et al. China’s human resources
for health: quantity, quality, and distribution. Lancet
2008;372:1774-81. Crossref
25. Meng Q, Liu X, Shi J. Comparing the services and quality of
private and public clinics in rural China. Health Policy Plan
2000;15:349-56. Crossref
26. Zhang Q, Chen J, Yang M, et al. Current status and job
satisfaction of village doctors in western China. Medicine
(Baltimore) 2019;98:e16693. Crossref
27. Chinese Statistics Press. National Accounts. In: China
Statistical Yearbook 2017. Available from: http://www.stats.gov.cn/tjsj/ndsj/2017/indexeh.htm. Accessed 6 Jun 2020.
28. Wass V, Van der Vleuten C, Shatzer J, Jones R. Assessment of clinical competence. Lancet 2001;357:945-9. Crossref
29. Lever J, Krzywinski M, Altman N. Principal component analysis. Nat Methods. 2017;14:641-2. Crossref
30. Chinese Statistics Press. Population. In: China Statistical Yearbook 2017. Available from: http://www.stats.gov.cn/tjsj/ndsj/2017/indexch.htm. Accessed 14 Jun 2020.
31. Li X, Liu J, Huang J, Qian Y, Che L. An analysis of the
current educational status and future training needs of
China’s rural doctors in 2011. Postgrad Med J 2013;89:202-8. Crossref
32. Dias SF, Severo M, Barros H. Determinants of health care
utilization by immigrants in Portugal. BMC Health Serv
Res 2008;8:207. Crossref
33. Myers SL, Xiaoyan G, Cruz BC. Ethnic minorities, race, and
inequality in China: a new perspective on racial dynamics.
Rev Black Polit Econ 2013;40:231-44. Crossref
34. Esmail A, Everington S. Racial discrimination against
doctors from ethnic minorities. BMJ 1993;306:691-2. Crossref
35. Iacobucci G. Specialty training: ethnic minority doctors’ reduced chance of being appointed is “unacceptable”. BMJ 2020;368:m479. Crossref
36. Zhang M, Wang W, Millar R, Li G, Yan F. Coping and
compromise: a qualitative study of how primary health
care providers respond to health reform in China. Human
Resour Health 2017;15:50. Crossref
37. Tan X, Liu X, Shao H. Healthy China 2030: a vision for
health care. Value Health Reg Issues 2017;12:112-4. Crossref
38. Windish DM, Reed DA, Boonyasai RT, Chakraborti C,
Bass EB. Methodological rigor of quality improvement
curricula for physician trainees: a systematic review and
recommendations for change. Acad Med 2009;84:1677-92. Crossref
39. Yi H, Wu P, Zhang X, Teuwen DE, Sylvia S. Market
competition and demand for skills in a credence goods
market: evidence from face-to-face and web-based non-physician
clinician training in rural China. PLoS One
2020;15:e0233955. Crossref
40. People Television. Training of ethnic minority grassroots
doctors in the central and western regions launched
[in Chinese]. Available from: http://tv.people.com.cn/n/2012/0915/c14645-19017341.html. Accessed 16 Jul 2020.