© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Primary pulmonary mucosa-associated lymphoid
tissue lymphoma with radiological presentation of middle lobe syndrome diagnosed by bronchoscopy: a case report
H Zhou, MD1; Z Yang, MD2; S Wu, MD1
1 Cancer Center, Department of Pulmonary and Critical Care Medicine, Zhejiang Provincial People’s Hospital (Affiliated People’s Hospital, Hangzhou Medical College), PR China
2 Cancer Center, Department of Pathology, Zhejiang Provincial People’s Hospital (Affiliated People’s Hospital, Hangzhou Medical College), PR China
Corresponding author: Dr S Wu (wushengchang@126.com)
Case report
In March 2018, a 49-year-old woman was admitted to
our respiratory medicine ward with a 2-year history
of recurrent productive cough. Symptoms first
developed after the patient underwent laparoscopic
myomectomy and subsequently developed a fever (around 38°C). Chest computed tomography (CT)
revealed patchy opacity in the right middle lobe
(Fig 1a and b). Based on these symptoms, she was
diagnosed with “pneumonia” for which antibiotics
were prescribed. Her fever resolved but cough
persisted so she was prescribed cough suppressants and antibiotics intermittently. These therapies were
likewise ineffective.
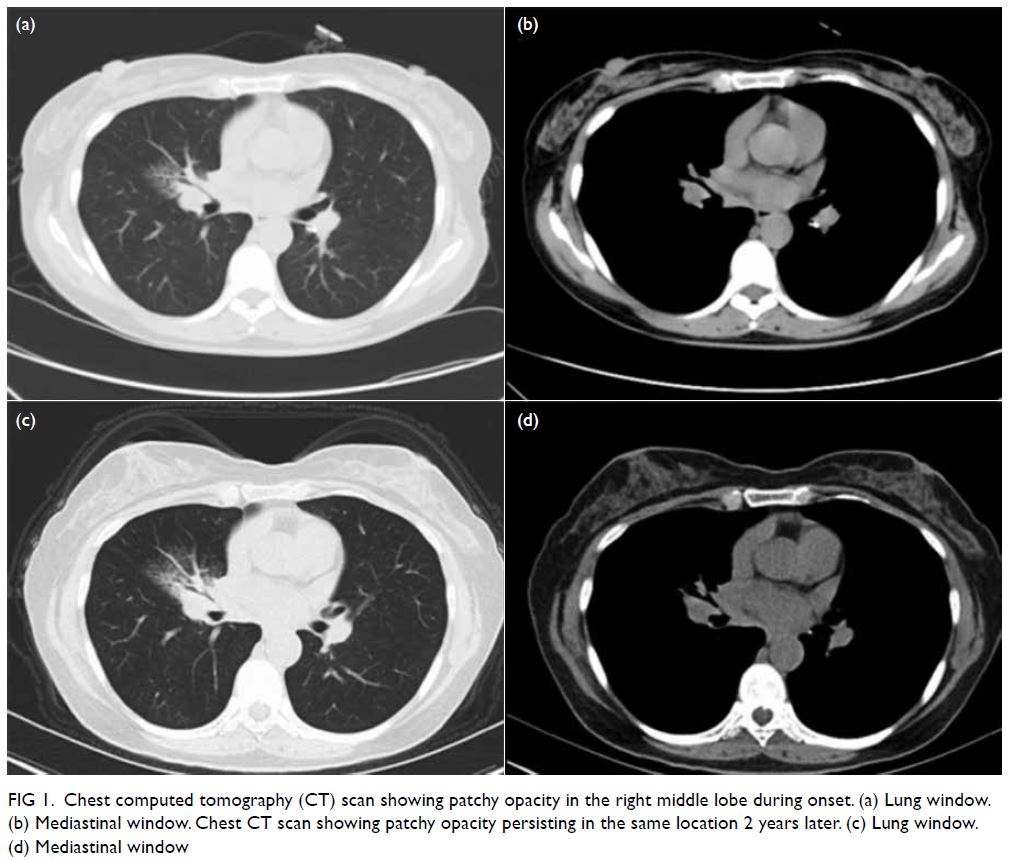
Figure 1. Chest computed tomography (CT) scan showing patchy opacity in the right middle lobe during onset. (a) Lung window. (b) Mediastinal window. Chest CT scan showing patchy opacity persisting in the same location 2 years later. (c) Lung window. (d) Mediastinal window
A series of tests and examinations conducted
during hospitalisation revealed no definitive cause
and symptoms again persisted. A new chest CT scan
revealed no change to the right middle lobe opacity
compared with previous CT scan and stenosis of the
middle bronchus (Fig 1c and d).
In the absence of any treatment response, the
patient was advised to undergo bronchoscopy that
revealed a narrowed lumen and rough mucosa of
the middle bronchus. Pathological examination
of mucosal tissue biopsy from the lesion revealed
infiltration of large numbers of lymphocytes
(Fig 2a and b) suggestive of diagnosis of lymphoma.
Further immunohistochemistry examination confirmed that the lesion was caused by mucosa-associated
lymphoid tissue (MALT) lymphoma.
These lymphoma cells tested positive for CD20,
CD79a and CD43 (Fig 2c-f). Further examinations
including positron emission tomography–computed
tomography and gastroscopy revealed no evidence
of lymphoma elsewhere.
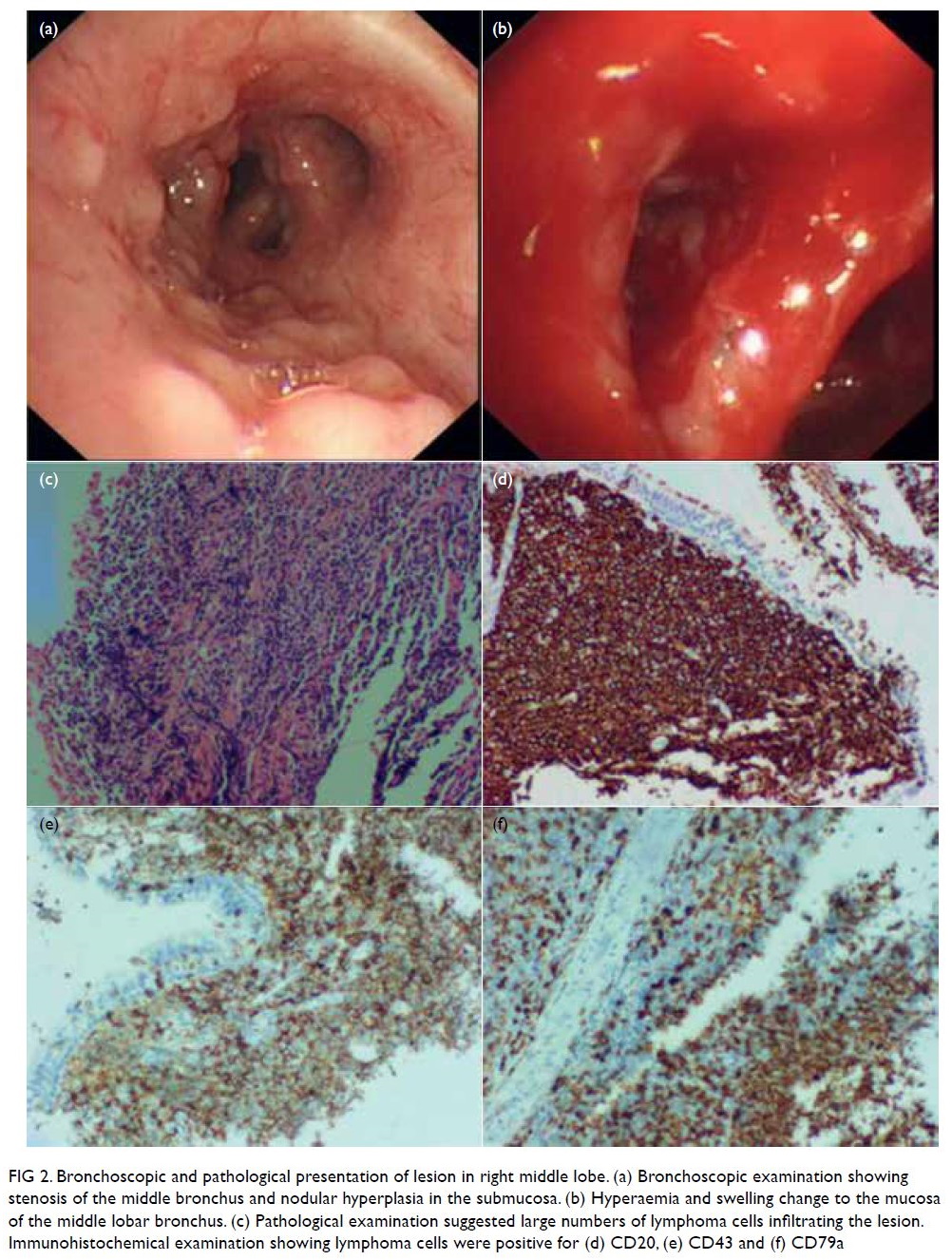
Figure 2. Bronchoscopic and pathological presentation of lesion in right middle lobe. (a) Bronchoscopic examination showing stenosis of the middle bronchus and nodular hyperplasia in the submucosa. (b) Hyperaemia and swelling change to the mucosa of the middle lobar bronchus. (c) Pathological examination suggested large numbers of lymphoma cells infiltrating the lesion. Immunohistochemical examination showing lymphoma cells were positive for (d) CD20, (e) CD43 and (f) CD79a
The patient underwent radiotherapy about
6 months after final diagnosis, with a total dose of
3960 cGy. After the last radiotherapy treatment,
chest CT confirmed that the lesion in the right
middle lobe had nearly disappeared. In addition,
symptoms of cough and expectoration had improved
significantly. The patient was followed up once every
3 months. Chest CT scan at the most recent follow-up
examination indicated no sign of relapse and her
symptoms had resolved.
Discussion
Primary pulmonary lymphoma belongs to a group of lymphoproliferative diseases, and accounts for 0.5%
to 1% of all pulmonary tumours.1 Mucosa-associated
lymphoid tissue lymphoma is the most common
pathological type of primary pulmonary lymphoma.2
However, the disease may not be diagnosed until
pathological examinations are conducted due to a
lack of clinical and radiological characteristics.
Previous study suggests that about half of patients with MALT lymphoma are asymptomatic
and some are diagnosed by accident.3 In patients
with symptoms, respiratory symptoms are more
frequently observed than B symptoms, including
fever, fatigue and weight loss.3 Our patient presented
with a transient B symptom of fever, but a chronic
respiratory symptom of cough.
The radiological presentation of this disease is diverse and includes nodules, masses, consolidation
and group glass opacity. Multiple lesions, which
are often bilaterally distributed, can be detected
by CT scan in most cases, but a solitary lesion is
less common in patients with MALT lymphoma.4
In addition, MALT lesions may occur in any lung
lobe or large airway including the trachea and main
bronchus.4 5 In our patient, the right middle lobe was affected, and middle lobe syndrome (MLS) was the
major radiological feature.
Middle lobe syndrome was first mentioned
several decades ago by Graham6 to describe
atelectasis of the right middle lobe. The syndrome is
usually caused by extrinsic compression or intrinsic
stricture of the middle lobe bronchus.6 However,
there is no uniform definition of this term. Broadly
speaking, MLS is defined as damage to the right
middle lobe due to any cause. The most common
causes are bronchiectasis, non-specific inflammation,
tuberculosis and tumours. Lung cancer is the most
common type of tumour affecting the middle lobe. As a haematological disease, MALT lymphoma can
affect any organ or tissue although in our patient, it
affected only the right middle lobe with consequent
misdiagnosis for more than 2 years. It is particularly
rare for MALT lymphoma to present as MLS. Only
one similar case has been reported: in 2004, Toishi
et al7 reported a 70-year-old male patient with a
radiological change of MLS who was diagnosed with
MALT lymphoma by right middle lobectomy. In
our case, the final diagnosis was obtained by biopsy
during bronchoscopy, not surgery.
Given that the clinical and radiological
features of MALT are non-specific, its definitive
diagnosis relies on pathology. Diffuse infiltration of
small lymphocytes into the bronchiolar mucosa is a
major histological characteristic. Moreover, reactive
lymphoid follicles and lymphoepithelial lesions are
commonly observed by microscopy.4 The molecular
markers of MALT are CD20, CD79a, CD43, as
observed in our case. CD5, CD10 and cyclin D are
always negative and may help to discriminate other
types of lymphoma. It was difficult to distinguish
this disease from infectious diseases and benign
lymphoproliferative diseases in the absence of
pathological examination.
Generally, MALT lymphoma is a tumour of
low-grade malignancy and patients have a rather good
prognosis. The 5-year survival rate for patients with
MALT lymphoma is >80%.4 The main treatments
for the disease are chemotherapy, radiotherapy,
target therapy and immunotherapy. Radiotherapy
is the first choice in patients with localised lesions.
It has been estimated that >90% of patients can
achieve a complete response after radiotherapy.8
Surgery may be indicated when the lesion is isolated
in certain organs, such as lung, thyroid gland, and
spleen. However, if MALT lymphoma progresses to
an advanced stage, or patients have a high tumour
burden, systemic therapy is recommended. Anti-CD20 combined with chemotherapy is considered
first-line treatment.7 In the present case, the patient
refused chemotherapy and agreed to radiotherapy
that relieved her symptoms with no obvious adverse
effects.
In summary, we first report MALT lymphoma
as a rare cause of MLS that was confirmed using a
minimally invasive approach. Mucosa-associated
lymphoid tissue lymphoma should be considered
a differential diagnosis when investigating the
aetiology of MLS.
Author contributions
Concept or design: H Zhou, S Wu.
Acquisition of data: Z Yang, S Wu.
Analysis or interpretation of data: H Zhou, Z Yang.
Drafting of the manuscript: H Zhou, S Wu.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: Z Yang, S Wu.
Analysis or interpretation of data: H Zhou, Z Yang.
Drafting of the manuscript: H Zhou, S Wu.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Ethics approval
The patient was treated in accordance with the Declaration of Helsinki. The patient provided written informed consent for all treatment and procedures and for publication of this
paper.
References
1. Cardenas-Garcia J, Talwar A, Shah R, Fein A. Update in primary pulmonary lymphomas. Curr Opin Pulm Med 2015;21:333-7. Crossref
2. Borie R, Wislez M, Antoine M, Copie-Bergman C, Thieblemont C, Cadranel J. Pulmonary mucosa-associated lymphoid tissue lymphoma revisited. Eur Respir J
2016;47:1244-60. Crossref
3. Zhang MC, Zhou M, Song Q, et al. Clinical features and outcomes of pulmonary lymphoma: a single center
experience of 180 cases. Lung Cancer 2019;132:39-44. Crossref
4. Sirajuddin A, Raparia K, Lewis VA, et al. Primary
pulmonary lymphoid lesions: radiologic and pathologic
findings. Radiographics 2016;36:53-70. Crossref
5. Kawaguchi T, Himeji D, Kawano N, Shimao Y, Marutsuka K.
Endobronchial mucosa-associated lymphoid tissue
lymphoma: a report of two cases and a review of the
literature. Intern Med 2018;57:2233-6. Crossref
6. Graham EA, Burford TH, Mayer JH. Middle lobe syndrome. Postgrad Med 1948;4:29-34. Crossref
7. Toishi M, Miyazawa M, Takahashi K, et al. Mucosa-associated lymphoid tissue lymphoma; report of two cases [in Japanese]. Kyobu Geka 2004;57:75-9.
8. Lumish M, Falchi L, Imber BS, Scordo M, von Keudell G, Joffe E. How we treat mature B-cell neoplasms (indolent B-cell lymphomas). J Hematol Oncol 2021;14:5. Crossref

