Hong Kong Med J 2014;20:24–31 | Number 1, February 2014 | Epub 20 Jun 2013
DOI: 10.12809/hkmj133924
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Intensive care unit admission of obstetric
cases: a single centre experience with contemporary update
Vivian KS Ng, MB, ChB, MRCOG1;
TK Lo, MB, BS, FHKAM (Obstetrics and Gynaecology)1; HH
Tsang, MRCP, FHKAM (Medicine)2; WL Lau, MB, BS, FHKAM
(Obstetrics and Gynaecology)1; WC Leung, MD, FHKAM
(Obstetrics and Gynaecology)1
1 Department of Obstetrics
and Gynaecology, Kwong Wah Hospital, Yaumatei, Kowloon, Hong Kong
2 Department of Intensive
Care, Kwong Wah Hospital, Yaumatei, Kowloon, Hong Kong
Corresponding author: Dr VKS Ng (vivian_nks@hotmail.com)
Abstract
Objectives: To review
the characteristics of a series of obstetric patients admitted
to the intensive care unit in a regional hospital in 2006-2010,
to compare them with those of a similar series reported from the
same hospital in 1989-1995 and a series reported from another
regional hospital in 1998-2007.
Design: Retrospective
case series.
Setting: A regional
hospital in Hong Kong.
Patients: Obstetric
patients admitted to the Intensive Care Unit of Kwong Wah
Hospital from 1 January 2006 to 31 December 2010.
Results: From 2006 to
2010, there were 67 such patients admitted to the intensive care
unit (0.23% of total maternities and 2.34% of total intensive
care unit admission), which was a higher incidence than reported
in two other local studies. As in the latter studies, the
majority were admitted postpartum (n=65, 97%), with postpartum
haemorrhage (n=39, 58%) being the commonest cause followed by
pre-eclampsia/eclampsia (n=17, 25%). In the current study,
significantly more patients had had elective caesarean sections
for placenta praevia but fewer had had a hysterectomy. The
duration of intensive care unit stay was shorter (mean, 1.8
days) with fewer invasive procedures performed than in the two
previous studies, but maternal and neonatal mortality was
similar (3% and 6%, respectively).
Conclusion: Postpartum
haemorrhage and pregnancy-induced hypertension were still the
most common reasons for intensive care unit admission. There was
an increasing trend of intensive care unit admissions following
elective caesarean section for placenta praevia and for early
aggressive intervention of pre-eclampsia. Maternal mortality
remained low but had not decreased. The intensive care unit
admission rate by itself might not be a helpful indicator of
obstetric performance.
New knowledge added by this
study
- There was an increasing trend of obstetric intensive care unit (ICU) admissions but with shorter stays.
- Well-planned fertility-sparing treatments for postpartum haemorrhage and placenta praevia may decrease resorting to hysterectomy.
- Other performance indicators in addition to crude ICU admission rates should be established to evaluate obstetric standards.
Introduction
Obstetric admissions to the intensive care
unit (ICU) and maternal mortality continue to have a significant
impact on maternal health care, despite the low rate of such
admissions in developed countries.1
Unlike others, obstetric patients pose a major management
challenge to ICU physicians and obstetricians due to altered
physiology during pregnancy, consideration of fetal wellbeing, and
the unique type of disorders to be dealt with.
Despite ongoing improvements in obstetric
care, more patients were admitted to ICU in the reviewed period
compared with decades earlier.2
Thus, the purpose of this study was to review and compare the
characteristics of obstetric patients admitted to the ICU over the
recent 20 years using historical controls, with respect to their
epidemiology, medical background, antenatal and peripartum risks,
durations of ICU stay, interventions in the ICU, and
predictability of the Acute Physiology and Chronic Health
Evaluation (APACHE II) score, as well as maternal and fetal
outcomes.
Methods
This was a retrospective case series of
obstetric patients admitted to the ICU of Kwong Wah Hospital, Hong
Kong, over a 5-year period from 1 January 2006 to 31 December
2010. Our hospital provides joint care with seven other hospitals
in the Kowloon West Cluster to residents of six districts, which
account for about 1.9 million inhabitants. Our obstetric service
is available for 24 hours each day for women in parts of the
Kowloon West and Wong Tai Sin districts. We provide out-patient
and in-patient services, including antenatal check-ups, prenatal
diagnoses, elective and emergency operations and services that are
supported by a blood bank and various laboratory test facilities
available for patients in hospital and in the community. Moreover,
24-hour midwifery, and perinatal and anaesthetic services are
available in our delivery suite. Our team consists of consultants,
associate consultants, as well as senior and junior residents.
Three staff (one specialist, two residents) are always available
on site for emergency admissions. Annually, we manage 5000 to 6000
deliveries, which is one of the highest delivery rates for a Hong
Kong hospital. Our ICU was established in 1968, currently has 14
beds, and admits 500 to 600 patients every year. The ICU team
consists of a critical care physician, a resident anaesthetist,
medical and surgical residents, and a nursing team with critical
care–registered nurse specialists.
This study was approved by the Ethics
Committee of the Kowloon West Cluster, Hospital Authority. No
patient consent was required as the study only involved review of
medical records.
Obstetric patients from 24 weeks of
gestation onwards to 6 weeks postpartum admitted to the ICU were
reviewed. They were identified via the computerised database
system adopted by the ICU. All corresponding medical records were
reviewed in detail. Supplementary information was retrieved from
the Clinical Management System, Electronic Patient Record, and
Obstetrics Clinical Information System.
Data retrieved for analysis included
patient demographics (age, ethnicity, smoking and drinking status,
parity, order of pregnancy, and body mass index [BMI] at booking
visit), antenatal booking status, number of antenatal visits,
medical history, perinatal risks, gestation at and mode of
delivery, indications for caesarean section, interventions
involved at and after delivery, indications and admission status
to the ICU, and maternal and fetal outcomes. Patient mortality was
predicted by recourse to the APACHE II score.
Indications for ICU admission were divided
into obstetric and non-obstetric causes. Obstetric causes were
those unique to pregnancy or liable to occur within 6 weeks of
delivery. Non-obstetric causes were those not specifically related
in pregnancy.
Interventions provided by ICU physicians
were classified into non-invasive and invasive. Those deemed
non-invasive included insertion of arterial or central lines,
blood product transfusion, use of continuous positive airway
pressure (CPAP) ventilation, and use of inotropes. Invasive
procedures included invasive mechanical ventilation,
cardiopulmonary resuscitation (CPR), defibrillation, and
haemodialysis.
Immediate and long-term complications of
the mothers and neonates were assessed up to 6 to 8 weeks
post-delivery. Maternal and perinatal mortalities were also
calculated.
Data were entered manually into Excel and
analysed using the Statistical Package for the Social Sciences
(SPSS version 17, Chicago [IL], US). The data were compared with
those from the results of a historical review in the same hospital
(1989-1995, by Tang et al2)
and a review in another regional hospital (1998-2007, by Leung et
al3). Chi squared or
Fisher’s exact tests were used to compare proportions and
Student’s t test to compare continuous variables.
Results
In all, 67 relevant patients were admitted
to the ICU and reviewed during the period of 1 January 2006 to 31
December 2010, which amounted to 0.23% of the total hospital
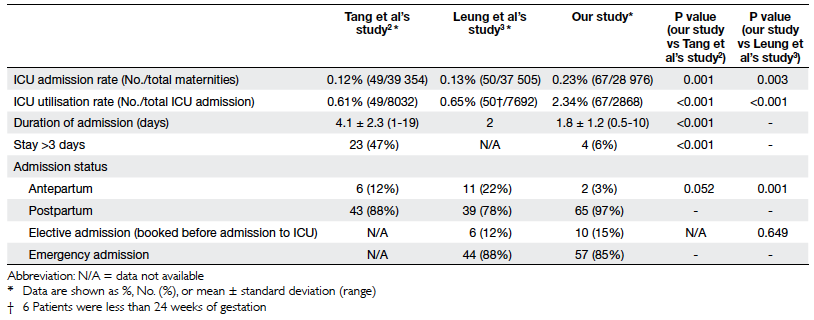
maternities and 2.34% of all ICU admissions (Table 1).
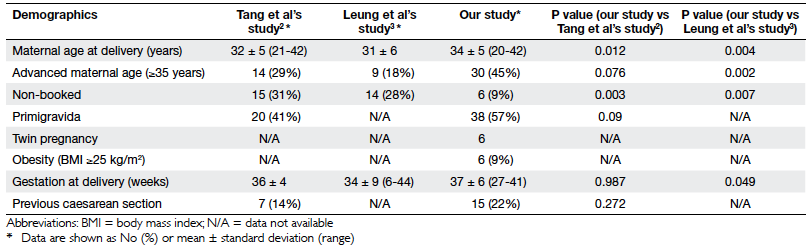
Their demographic features are shown in Table 2. The mean age of women at delivery
was 34 (standard deviation [SD], 5; range, 20-42) years. Thirty
(45%) of the patients were of advanced maternal age (ie age at
confinement of ≥35 years). The majority of them were Chinese
(n=65, 97%), one was Filipino and one an Indonesian. Nine (13%)
patients were visitors from mainland China. Seven (10%) were
smokers, two (3%) drank alcohol regularly and two (3%) had a
history of substance abuse. In all, 38 (57%) were nulliparous and
six (9%) carried twin pregnancies. Most of the patients (n=61,
91%) were booked in our unit; 19 (28%) had three antenatal
check-ups or less.
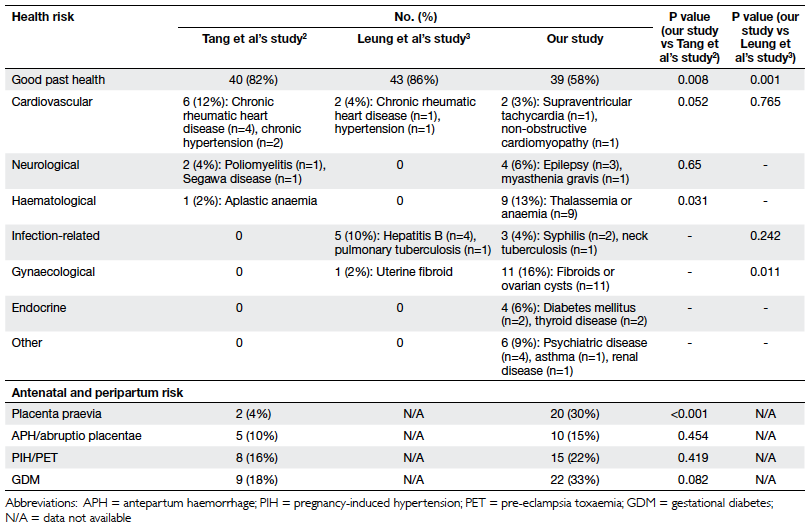
Among these 67 patients, 39 (58%) enjoyed
good past health, and six (9%) had a BMI of more than 25 kg/m2 at
their booking visit. The most common co-existing diseases were
gynaecological (n=11, 16%) and haematological (n=9, 13%). Their
antenatal and peripartum risks are summarised in Table 3.
The mean gestational age at delivery was 37
(SD, 6; range, 27-41) weeks. Most of them were delivered by
emergency caesarean section (n=34, 51%), including one transferred
to us after delivery in the private sector. One patient remained
undelivered and died antenatally. Placenta praevia and
pregnancy-induced hypertensive disorders were the main indications
for elective and emergency caesarean sections, respectively. Other
indications are listed in Table 4.
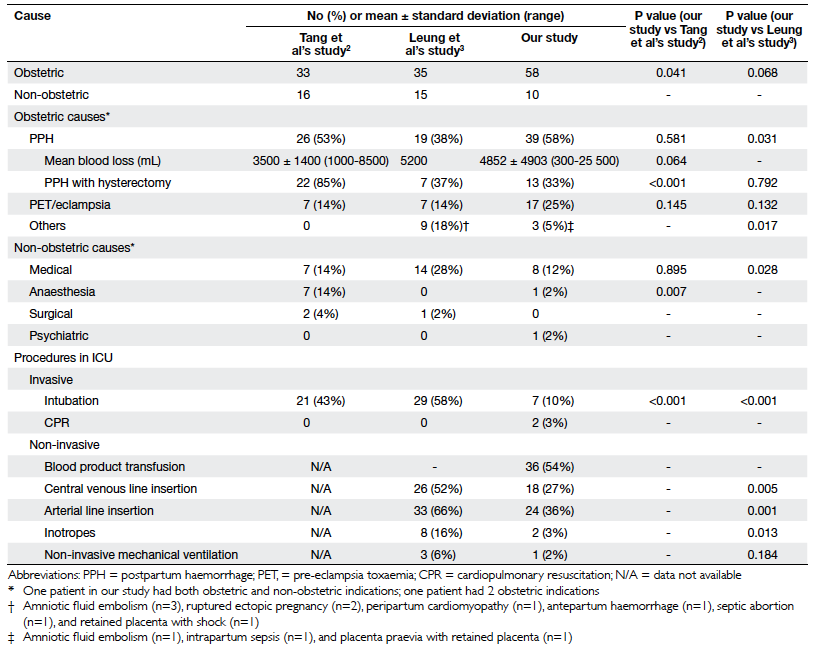
The reasons for ICU admission and
procedures undertaken therein are listed in Table 5.
Most were admitted to the ICU postpartum (n=65, 97%) and for
obstetric problems (n=58, 87%), of which postpartum haemorrhage
(PPH) was the leading cause (n=39, 58%) followed by pre-eclamptic
toxaemia (PET) or eclampsia (n=17, 25%). The mean duration of ICU
stay was 1.8 (SD, 1.2; range, 0.5-10) days; four (6%) of the
patients stayed for more than 3 days.
In all, 39 patients were admitted to the
ICU due to a PPH, the mean estimated blood loss was 4852 mL. Major
causes of PPH were related to placenta praevia (n=16), uterine
atony (n=12), and perineal trauma (n=5). Blood products given
included packed cells (mean, 12 units), platelet concentrate
(mean, 5 units), fresh frozen plasma (mean, 7 units), and
cryoprecipitate (mean, 1 unit). Three patients received
recombinant factor VIIa (NovoSeven; Novo Nordisk A/S, Bagsværd,
Denmark). Procedures to control PPH included compression sutures
(n=10), uterine artery embolisation (n=9), insertion of a
Sengstaken-Blakemore tube (n=6), and uterine artery ligation
(n=2). There were 13 patients who underwent hysterectomy despite
multiple other interventions and use of multiple uterotonics, and
eight patients with PPH were complicated with disseminated
intravascular coagulation, one had a ventricular tachycardia, and
one had a urinary tract injury. One of the patients with a PPH and
anaphylactic shock suffered a cavernous sinus thrombosis and a
cranial nerve VI palsy, for which she received therapeutic doses
of low-molecular-weight heparin. Another patient was admitted 2
weeks after delivery due to delirium secondary to sepsis.
There were 17 patients admitted to the ICU
for PET or eclampsia (9 of whom had eclampsia) and were all
stabilised in the ICU. Two patients had HELLP (haemolysis,
elevated liver enzymes, low platelets) syndrome and two had
hypertensive encephalopathy diagnosed on the basis of computed
tomography. Other complications included acute pulmonary oedema
(n=1), deranged renal function (n=3), deranged liver function
(n=1), and aspiration pneumonitis (n=1). Another eight had
persistent hypertension 6 weeks postpartum and were referred to
physicians.
Regarding the 10 patients (15% of the
cohort) admitted to the ICU for non-obstetric reasons, two had an
epileptic seizure, three had cardiovascular problems
(cardiomyopathy, heart failure, and pulmonary hypertension), and
one each had renal disease, ethanol toxicity, acute pulmonary
oedema, myasthenia gravis, and anaphylactic shock.
Invasive procedures performed in the ICU
were CPR (n=2, 3%) and mechanical ventilation (n=7, 10%).
Non-invasive procedures were blood product transfusions (n=36,
54%), central line insertion (n=18, 27%), arterial line insertion
(n=24, 36%), use of inotropes (n=2, 3%), and CPAP ventilation
(n=1, 2%).
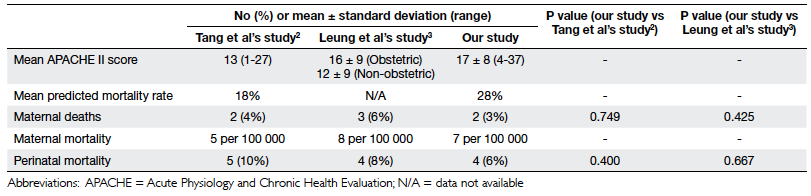
The mean APACHE II score was 17 (range,
4-37) and the mean predicted mortality rate was 28% (range,
4-85%). The actual mortality rate in this series was 3% (Table 6).
The maternal mortality ratio (MMR; actual/predicted mortality) was
0.11.
In our study period, there were two
maternal deaths in the 28 976 maternities or 7 per 100 000 births,
both in ICU patients. One was a patient who enjoyed good health
but suspected to have pulmonary hypertension at 27 weeks of
gestation, who rapidly deteriorated and died 1 day after
admission. Her diagnosis was confirmed at postmortem examination.
The other maternal death ensued in the postpartum period due to
multi-organ failure and brain death, secondary to eclampsia and
intraventricular haemorrhage.
Regarding these ICU admissions, three (5%)
of the fetuses endured intrauterine death (IUD) and one (2%) whose
neonate died (due to necrotising enterocolitis). The IUDs were
associated with abruptio placentae, pulmonary hypertension, and
severe pre-eclampsia with early intrauterine growth restriction.
Discussion
The health care system of Hong Kong aims to
protect/ improve maternal and child health, by means of antenatal,
intrapartum, and postnatal services that are readily available at
very low costs. Whilst the MMR fluctuated between 1.0 and 11.2 per
100 000 live births over the past 31 years,4 5 the
above-mentioned services have contributed to the decreasing and
now very low maternal mortality rates.
Despite advances in obstetric care, the
admission rate to the ICU had doubled compared with a decade ago
(from 0.12% to 0.23%).2
Whereas such ICU utilisation rates for obstetric cases were also
higher compared with Tang et al’s data2
(2.34% vs 0.61%), nevertheless they were low compared to reports
from overseas.6 7 The rates were also higher than those reported
by Leung et al (admission, 0.13%; utilisation, 0.65%).3 One of the reasons for the rise in ICU
admission rates was changes in patient allocation in our hospital,
and over the Hong Kong Special Administrative Region. The number
of beds in our ICU was reduced from 18 to 14 after the severe
acute respiratory syndrome epidemic in 2003. The number of
surgical admissions was also much lower than a decade earlier.
Moreover, the number of trauma cases dropped significantly, since
two other nearby tertiary hospitals became trauma centres.
Changing attitudes of obstetricians and anaesthetists also
contributed to the increase in ICU admission rate. Given the fact
that our patients were most commonly delivered by elective
caesarean section for placenta praevia, a proper preoperative
management plan with a multidisciplinary approach involving
anaesthetist, intensive care physician, and obstetricians should
have been available before the operation, which included booking
of the ICU bed. With the increasing trend of placenta praevia, it
was expected that more and more patients would be admitted to the
ICU electively for monitoring rather than any future active
intervention. The shorter duration of ICU stays, compared with
those detailed earlier by Tang et al,2
is probably consistent with this trend towards elective
admissions.
The mean age of our patients at delivery
was higher than that in the patient series described by Tang et
al2 and Leung et al.3
Indeed, patients of advanced maternal age were more likely to be
admitted to the ICU when compared with our background population,
though this was not shown for such ICU admissions reported by
Selo-Ojeme et al.8
Increasing maternal age implies that our patients were more likely
to have co-existing diseases complicating pregnancy, as reflected
by our data, even though the medical problems in question were
generally mild and stable.
According to Tang et al’s2 and Leung et al’s3
reports about non-booked cases (NBCs), patients from mainland
China used to be admitted via the emergency department very late
when they went into advanced labour. As a result, potential or
present obstetric complications were known to us only when they
were admitted. With the commencement of the policy to allow these
mothers to register and deliver in Hong Kong (since 2007), the
number of NBCs decreased significantly, as did their number of ICU
admissions.
In the literature there are conflicting
data when parity is considered one of the risk factors for ICU
admission. In our study, nulliparity was not related to ICU
admission, which was also what Pollock et al noted.6
During our data analysis, twin pregnancy
was more likely in our ICU patients compared with the background
population. However, such data cannot be retrieved from Tang et
al’s or Leung et al’s reports.2
3 Twin pregnancy is known
to confer a higher risk of gestational diabetes, hypertension,
premature delivery, operative deliveries, and postpartum
complications (including PPH).9
10 Our findings also
supported the need of a specialised twin pregnancy clinic to look
after this high-risk group.
Placenta praevia was the most frequent risk
factor identified in our patient series, being much more common
than in Tang et al’s study.2
Increasing popularity of evaluation by ultrasound has raised the
detection rate of placenta praevia early in the antenatal period.
All our patients with placenta praevia were delivered electively
with proper preoperative arrangements. These entailed booking of
ICU facilities, standby uterine artery embolisation, preparation
of recombinant factor VIIa and Sengstaken-Blakemore tubes, and
involvement of obstetric consultants to make decisions. One
consequence was a significantly higher number of elective
caesarean sections for placenta praevia compared with decades ago,
though the overall section rate remained relatively stable.11 This also correlated with placenta praevia
being the commonest causes of PPH in our ICU patients.
As in Tang et al’s2
and Leung and et al’s3
studies, in our series admissions due to obstetric problems
remained the main cause of obstetric ICU admissions. Postpartum
haemorrhage was consistently the most common indication for ICU
admission, which was also noted in Tang et al’s series.2 Although the mean estimated blood loss of our
patients was apparently higher than that reported by Tang et al,2 and abdominal delivery is
known to increase the risk of hysterectomy following PPH,12 the number of hysterectomies performed was
significantly lower than before. The increasing use of compression
sutures and uterine artery embolisation together with strategies
to retain the placenta in cases of placenta accreta might account
for the decreasing recourse to hysterectomy compared with 20 years
ago.
The current series had more patients with
pre-eclampsia or eclampsia admitted to the ICU than those reported
by Tang et al,2 although
the difference was not statistically significant. As suggested by
the National Institute for Health and Clinical Excellence
guideline,12 our management
protocol was updated to incorporate the more liberal use of
antihypertensives and magnesium sulphate. Our use of the modified
early obstetric warning scoring system allowed early detection of
potential complications to prevent poor obstetric outcomes.
Intensive care is indicated in patients with severe hypertension,
or moderate hypertension with symptoms of impending eclampsia or
any suggestion of organ dysfunction. These innovations lead to the
rising trend of ICU admissions to monitor for pre-eclampsia.
Active involvement of anaesthetists plays a
role in the changing pattern of obstetric ICU admissions. There
was a drastic reduction of admissions for anaesthesia-related
causes compared with those reported by Tang et al.2 Only one of our patients was admitted due to
anaphylactic shock, which can be explained by the significant
improvements in anaesthetic care and mechanical ventilation in our
hospital. Invasive and non-invasive procedures (eg intubation and
insertion of arterial and central venous lines) undertaken in the
ICU were significantly fewer than decades ago, as most of them had
been performed before admission to ICU by anaesthetists.
In our series, the mean duration of ICU
stay was 1.8 days, which was shorter than 4.1 days reported in
Tang et al’s study.2 The
change in attitude and approach to management of both
obstetricians and anaesthetists made ICU admission a more elective
occurrence than before. As a result, patients admitted to the ICU
tended to be more stable and fewer invasive interventions were
warranted. These observations highlight the need for obstetric
high-dependency units to cater for patients requiring more
intensive care, but not to the extent of ICU support.13
When compared with the findings reported by
Leung et al,3 over the
decades there was no significant increase in perinatal mortality,
nor was there an increased rate of fetal loss when compared with
our background population. Nevertheless, maternal mortality had
not decreased. In our series, there were two maternal deaths that
amounted to a mortality rate of 7 per 100 000 maternities. In Tang
et al’s series2 the
maternal mortality was 5 per 100 000, and in the UK it was
reported to be 14 and 11 per 100 000 in 2003-2005 and 2006-2008,
respectively.14 However,
these differences between series were not statistically
significant.
One limitation of our study was that data
collection from the computerised system might have omitted
pregnant women admitted to the ICU from other specialties with
diagnoses that were not obstetrically related. A second limitation
was that the causes of maternal ICU admission may not relate
directly to the causes of maternal mortality. For example,
thromboembolism, one of the leading causes of maternal death in
the UK, was not a major cause of ICU admission. In the UK, only
30% of such maternal deaths were in patients admitted to the ICU,15 and on this issue there
is no global consensus on the optimal indications for ICU
admission. A third limitation was that the frequency of obstetric
ICU admissions is also affected by the standard of obstetric care
and the threshold admission criteria determined by obstetricians,
anaesthetists, and intensive care physicians. As a result, ICU
admissions may not truly reflect the standard of obstetric care.16 A composite performance
indicator of obstetric care by combining the frequency of ICU
admission, numbers of emergency admissions and/or proportions of
emergency/elective admissions, and proportions having prolonged
stays (eg >3 days) could be a more useful measure of the
standard of obstetric practice in the future.
The APACHE II scoring system has been used
as a quantitative predictor of mortality, mainly in medical and
surgical patients admitted to the ICU using several physiological
measures. Its potential has also been evaluated when applied to
obstetric patients. According to different overseas reviews, it
may overestimate risks in pregnant patients, as in them normal
physiology can differ, often in subtle ways, and can undergo
abrupt changes in various emergency conditions.17 18
Thus, to date, there is still no proper screening system for
obstetric emergencies. A specific scoring system for obstetric
patients should be developed and warrants a large-scale
international prospective study for this purpose.
The majority of patients discharged from
our ICU enjoyed satisfactory recoveries in the puerperal period.
In all, eight patients with hypertensive disorder in pregnancy had
persistent hypertension for which they were referred for medical
assessment. In our series, long-term outcome was not determined.
Leung et al3 found that
women admitted to the ICU had lower mean scores for quality of
life than normal Hong Kong females of similar age, but these
authors commented that the relationship of low scores to the
obstetric illnesses was unclear and might be resolved by long-term
patient follow-up.
In some respects, Leung et al’s study3 also provided us with geographical controls.
However, they included patients with gestational ages of <24
weeks, which complicated any comparison of risk factors. Moreover,
being intensive care physicians they emphasised quality of life
after discharge from the ICU. In contrast, we obstetricians looked
for indicators to prevent/reduce maternal ICU admissions, as
advocated in modern obstetrical care guidelines.
Conclusion
Our findings illustrate the various
changes in ICU admission practice of obstetric cases in the last
20 years, and are comparable to those in other developed
countries. Elective caesarean section for placenta praevia and PPH
were the major reasons for ICU admission. More conservative
management of placenta praevia and PPH appeared to reduce
resorting to hysterectomy. These ongoing changes in practice may
make emergency obstetric admissions to the ICU less likely in the
future. Maternal mortality in our unit has remained low over the
years, and can hardly be reduced any further. It is therefore more
important to refine and improve obstetric practice to reduce
maternal morbidity. The ‘near-miss’ in terms of obstetric ICU
admission rates, together with measures targeting the duration of
ICU stay, and a potential obstetric morbidity scoring system will
no doubt better reflect our clinical performance standards in the
future.
References
1. Public Health Agency of Canada.
Make every mother and child count: report on maternal and child
health in Canada. 2005. Available from:
http://publications.gc.ca/collections/
Collection/H124-13-2005E.pdf. Accessed Jun 2010.
2. Tang LC, Kwok AC, Wong AY, Lee
YY, Sun KO, So AP. Critical care in obstetrical patients: an
eight-year review. Chin Med J (Engl) 1997;110:936-41.
3. Leung NY, Lau AC, Chan KK, Yan
WW. Clinical characteristics and outcomes of obstetric patients
admitted to the intensive care unit: a 10-year retrospective
review. Hong Kong Med J 2010;16:18-25.
4. Department of Health, Hong Kong.
Chapter 1: Health of community. Annual Report 2009/2010.
5. Department of Health, Hong Kong.
Number of maternal deaths by major disease group, 2001-2009.
Available from: www.healthyhk.gov.hk/phisweb/reports/2009_01_01_
MOT00101.xls. Accessed Aug 2010.
6. Pollock W, Rose L, Dennis CL.
Pregnant and postpartum admissions to the intensive care unit: a
systematic review. Intensive Care Med 2010;36:1465-74. Crossref
7. Togal T, Yucel N, Gedik E,
Gulhas N, Toprak HI, Ersoy MO. Obstetric admissions to the
intensive care unit in a tertiary referral hospital. J Crit Care
2010;25:628-33. Crossref
8. Selo-Ojeme DO, Omosaiye M,
Parijat Battacharjee P, Kadir RA. Risk factors for obstetric
admissions to the intensive care unit in a tertiary hospital: a
case-control study. Arch Gynecol Obstet 2005;272:207-10. Crossref
9. Liu AL, Yung WK, Yeung HN, et
al. Factors influencing the mode of delivery and associated
pregnancy outcomes for twins: a retrospective cohort study in a
public hospital. Hong Kong Med J 2012;18:99-107.
10. Yung WK, Liu AL, Lai SF, et
al. A specialised twin pregnancy clinic in a public hospital. Hong
Kong J Gynaecol Obstet Midwifery 2012;12:21-32.
11. Department of Obstetrics and
Gynaecology, Kwong Wah Hospital. Annual Report 2006-2010.
12. National Institute for Health
and Clinical Excellence. Caesarean section. NICE Clinical
Guidelines, No 132. 2010.
13. Mirghani HM, Hamed M,
Ezimokhai M, Weerasinghe DS. Pregnancy-related admissions to the
intensive care unit. Int J Obstet Anesth 2004;13:82-5. Crossref
14. Cantwell R, Clutton-Brock T,
Cooper G, et al. Saving mothers’ lives: reviewing maternal deaths
to make motherhood safer: 2006-2008. The eighth report on
confidential enquiries into maternal deaths in the United Kingdom.
BJOG 2011;118(Suppl 1):1S-203S. Crossref
15. Lewis G, Clutton-Brock T,
Cooper G, et al. Saving mothers’ lives: reviewing maternal deaths
to make motherhood safer–2003-2005. The seventh report on
confidential enquiries into maternal deaths in the United Kingdom.
London: CEMACH; 2007.
16. Baskett T, Sternadel J.
Maternal intensive care and near-miss mortality in obstetrics. Br
J Obstet Gynaecol 1998;105:981-4. Crossref
17. Vasquez DN, Estenssoro E,
Canales HS, et al. Clinical characteristics and outcomes of
obstetric patients requiring ICU admission. CHEST 2007;131:718-24.
Crossref
18. Gilbert TT, Smulian JC, Martin
AA, et al. Obstetric admissions to the intensive care unit:
outcomes and severity of illness. Obstet Gynecol 2003;102:897-903.
Crossref