Hong Kong Med J 2022 Apr;28(2):107–15 | Epub 31 Mar 2022
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE CME
Surgical treatment of pelvic organ prolapse in
women aged ≥75 years in Hong Kong: a multicentre retrospective study
Daniel Wong, MB, BS, FHKAM (Obstetrics and Gynaecology)1; YT Lee, MB, ChB, FHKAM (Obstetrics and Gynaecology)2; Grace PY Tang, MB, BS, FHKAM (Obstetrics and Gynaecology)3; Symphorosa SC Chan, MD, FRCOG4
1 Department of Obstetrics and Gynaecology, Pamela Youde Nethersole
Eastern Hospital, Hong Kong
2 Department of Obstetrics and Gynaecology, Prince of Margaret Hospital,
Hong Kong
3 Department of Obstetrics and Gynaecology, Kwong Wah Hospital, Hong
Kong
4 Department of Obstetrics and Gynaecology, Prince of Wales Hospital,
Hong Kong
Corresponding author: Dr Daniel Wong (dlwhk@yahoo.com)
Abstract
Introduction: Pelvic organ prolapse (POP) is
common among older women. With the increasing
lifespan and emphasis on quality of life worldwide,
older women increasingly prefer surgical treatment
for POP. We reviewed the surgical treatment of
POP in older women to characterise its safety,
effectiveness, and the type most often selected.
Methods: This multicentre, retrospective study
was conducted at four hospitals between 2013 and
2018. Included patients were aged ≥75 years and
had undergone POP surgery. We compared patient
demographic characteristics, POP severity, and
surgical outcomes between reconstructive and
obliterative surgeries; these comparisons were also
made among vaginal hysterectomy plus pelvic floor
repair (VHPFR), transvaginal mesh surgery (TVM),
vaginal hysterectomy (VH) plus colpocleisis, and
colpocleisis alone.
Results: In total, 343 patients were included; 84.3%
and 15.7% underwent reconstructive and obliterative
surgeries, respectively. Overall, 246 (71.7%), 43
(12.5%), 20 (5.8%), and 34 (9.9%) patients underwent
VHPFR, TVM, VH plus colpocleisis, and colpocleisis
alone, respectively. Patients who were older (81.9 vs
79.6 y; P=0.001), had vault prolapse (38.9% vs 3.5%;
P<0.001), and had medical co-morbidities (37%
vs 4.8%; P<0.001) chose obliterative surgery more frequently than reconstructive surgery. Obliterative
surgeries had shorter operative time (73.5 min vs
107 min; P<0.001) and fewer surgical complications
(9.3% vs 28.0%; P=0.003). Vaginal hysterectomy plus
pelvic floor repair had the highest rate of surgical
complications (most were minor), while colpocleisis
alone had the lowest rate (30.1% vs 8.8%; P=0.01).
Conclusions: Pelvic organ prolapse surgeries were safe and effective for older women. Colpocleisis may be appropriate as primary surgery for fragile older women.
New knowledge added by this study
- The most common type of pelvic organ prolapse (POP) surgery was vaginal hysterectomy plus pelvic floor repair. Patients who were older (81.9 vs 79.6 y; P=0.001), had medical co-morbidities (37% vs 4.8%; P<0.001), had a history of pelvic floor repair surgery (13% vs 1.7%; P=0.001), and had vaginal vault prolapse (38.9% vs 3.5%; P<0.001) chose obliterative surgery more frequently than reconstructive surgery.
- Because all types of POP surgery were associated with no mortality and generally had self-limiting surgical complications, they are safe for women aged ≥75 years. However, fluid replacement should be cautiously administered in fragile patients and in patients susceptible to fluid overload.
- Colpocleisis alone had the shortest operative time (60 min; P<0.001), least blood loss (50 mL; P<0.001), and fewest surgical complications (8.8%; P=0.01). Moreover, 76.5% of procedures comprising colpocleisis alone were performed under spinal anaesthesia (P<0.001).
- All four types of POP surgeries are safe and effective for the treatment of POP in older women.
- The incidence of carcinoma of the corpus uteri (Ca corpus) was 0.3% in this study. To reduce the risk of missing Ca corpus, preoperative transvaginal ultrasound (to assess endometrial thickness) and endometrial aspiration should be considered women who plan to undergo uterine-preserving surgery.
- Comparison of vaginal hysterectomy plus colpocleisis and colpocleisis alone showed that the combined treatment had a longer operative time and greater blood loss, but a comparable rate of complications. Therefore, vaginal hysterectomy plus colpocleisis remains a valid treatment option. Both methods involving colpocleisis lead to difficulty in assessment of the cervix and uterus regardless of pathology.
- Colpocleisis alone had the shortest operative time, least blood loss, and fewest surgical complications. These excellent results suggest that colpocleisis may be appropriate as primary surgery for fragile older women who do not engage in sexual intercourse.
Introduction
The incidence of pelvic organ prolapse (POP) is
reportedly near 50% and the lifetime risk of POP
requiring surgery is approximately 20%.1 2 With the
increasing lifespan and emphasis on quality of life
worldwide, older women increasingly prefer surgical
treatment, instead of vaginal pessaries, as definitive
treatment for POP.3 Surgical treatment options are
either reconstructive or obliterative. Reconstructive
surgery comprises native tissue repair (mainly
vaginal hysterectomy [VH]), pelvic floor repair, and
mesh-related repair; obliterative surgery comprises
colpocleisis with or without concomitant VH.
Older women who undergo urogynaecological
surgery have a higher surgical risk, regardless of
fragility index; they have lower risks of prolapse
recurrence and repeated surgery.4 Although the
World Health Organization has defined old age as
≥65 years,5 a threshold of ≥75 years may be more
appropriate for older women in terms of fragility and
need for care. A previous Hospital Authority ageing
projection6 indicated that the number of individuals
aged 75 to 84 years will substantially increase in
Hong Kong, while the numbers of individuals aged
≥85 years or ≤74 years will remain comparatively
stable. A threshold of ≥75 years for geriatric medicine
may be reasonable because most chronic, complex disabling disease occurs among individuals in this age-group.7
To our knowledge, despite the increasing
number of women aged ≥75 years and the need for
surgical treatment of POP among these individuals,
there is limited evidence regarding the risks and
benefits of the available surgical options. This
multicentre, retrospective study was performed
to review the surgical treatment of POP in women
aged ≥75 years; we aimed to characterise its safety,
effectiveness, and the type most often selected. We
hope that the findings will help clinicians to counsel
older women with POP who are considering surgical
treatment.
Methods
Patients
This multicentre, retrospective cohort study was
conducted at Kwong Wah Hospital, Pamela Youde
Nethersole Eastern Hospital, Princess Margaret
Hospital, and Prince of Wales Hospital. We included
patients aged ≥75 years, all of whom underwent
surgical treatment of POP in one of the above four
gynaecological units between 2013 and 2018. We
reviewed patient information from the Clinical
Data Analysis and Reporting System and Clinical
Medical System; for patients with incomplete data
in the Clinical Medical System, we reviewed paper-based
medical records. Ethical approvals were
obtained from the Institutional Review Boards of
all four Clusters including Hong Kong East Cluster,
Kowloon Central Cluster, Kowloon West Cluster
and New Territories East Cluster.
Examination and treatment selection
Demographic data and symptoms of prolapse
were collected during each patient’s first visit
to a participating gynaecology unit. Physical
examinations were conducted to confirm POP,
stage of prolapse, and the compartments involved;
all examinations were performed using the
International Continence Society Pelvic Organ
Prolapse Quantification (POP-Q) staging system.7
Patients were offered vaginal pessary management
or surgical treatment. Patients who opted for surgical
treatment were scheduled for surgery with or without
a trial period of vaginal pessary management.
Preoperative urodynamics studies were performed if
indicated. During the preoperative assessment, each
patient underwent a comprehensive evaluation that
included patient-reported symptoms of prolapse,
as well as urinary, intestinal, and sexual statuses;
they also underwent prolapse assessment using
POP-Q staging. Thorough counselling was provided
regarding reconstructive and obliterative treatment
options, including a discussion of the potential
benefits and risks of both procedures, as well as the need for concomitant VH or mid-urethral sling transobturator tape (TVT-O) for urodynamic stress incontinence.
Surgical procedures
Reconstructive procedures involved native tissue
repair and mesh-related surgery. Native tissue repair
mainly comprised vaginal hysterectomy followed
by pelvic floor repair (VHPFR; eg, anterior and/or
posterior colporrhaphy). In addition, sacrospinous
ligament fixation was performed for stage ≥III
uterine prolapse or vaginal vault prolapse. Patients
with stage ≥III anterior compartment prolapse were
offered anterior vaginal mesh repair. Obliterative
surgery comprised colpocleisis with or without
concomitant VH. Anterior vaginal mesh repair
and colpocleisis were only offered to patients who
were sexually inactive before surgery or agreed not
to engage in sexual intercourse. Combinations of
concomitant procedures were performed in the
following order, using only the procedures selected
by each patient and their surgeon: VH, mesh
placement and sacrospinous fixation, native tissue
repair, and TVT-O placement. All native tissue
repair procedures were performed or supervised by
a gynaecological specialist; all sacrospinous ligament
fixation or anterior vaginal mesh repair procedures
were performed or supervised by urogynaecologists.
One dose of prophylactic intravenous antibiotic
was administered during anaesthesia induction.
In patients who underwent reconstructive surgery,
one piece of vaginal gauze was placed to achieve
haemostasis for 1 day. A Foley catheter was placed
to ensure urinary drainage for 1 to 2 days according
to the procedures used in each unit. Operative
time, intra-operative blood loss, perioperative
complications, and postoperative adverse events
were recorded. Postoperative fever was defined as
≥2 readings of temperature ≥38°C with no positive
culture or identifiable cause. A diagnosis of urinary
tract infection was made on the basis of positive
midstream urine culture results. A diagnosis of
urinary retention was made when a patient could not
void and required catheterisation. All instances of
postoperative haematoma were diagnosed by imaging
(ultrasound or computed tomography scan). When
available, pathology reports were also reviewed.
Postoperative assessments
All patients underwent the same postoperative
assessment, which was structured using a
standardised datasheet. Follow-up visits were
scheduled at 6 to 12 weeks and 1 year after surgery,
then annually until 5 years after surgery. Each follow-up
visit evaluation included assessments of urinary
and intestinal function; symptoms of prolapse,
vaginal pain and dyspareunia; and symptoms of mesh erosion. Vaginal examinations and POP-Q
assessments were performed to identify instances
of POP recurrence or mesh-related complications,
in accordance with the recommendations of
the International Continence Society and the
International Urogynecological Association.9
Prolapse recurrence was defined as the presence of
subjective symptoms of prolapse or a POP-Q stage
of ≥II in a clinical examination.
Statistical analysis
We compared patient demographic characteristics,
POP severity, and surgical outcomes between two
groups: reconstructive and obliterative surgeries.
These comparisons were also made among four
subgroups: VHPFR, transvaginal mesh surgery
(TVM), VH plus colpocleisis, and colpocleisis alone.
Statistical analyses were performed using SPSS
(Windows version 26.0; IBM Corp, Armonk [NY],
United States). Descriptive statistics were used to
summarise demographic and clinical characteristics.
Continuous variables were expressed as mean
(standard deviation) or median (interquartile
range); they were analysed by independent-samples
t tests or the Mann-Whitney U test (comparison
of two groups)/one-way analysis of variance or
Kruskal–Wallis H test (comparison of ≥3 groups),
depending on the normality of the data assessed by
Shaprio–Wilk test. Categorical data were expressed
as numbers and percentages; the Chi squared test
and Fisher’s exact test were used for categorical
data analysis. A P value of <0.05 was considered
statistically significant.
Results
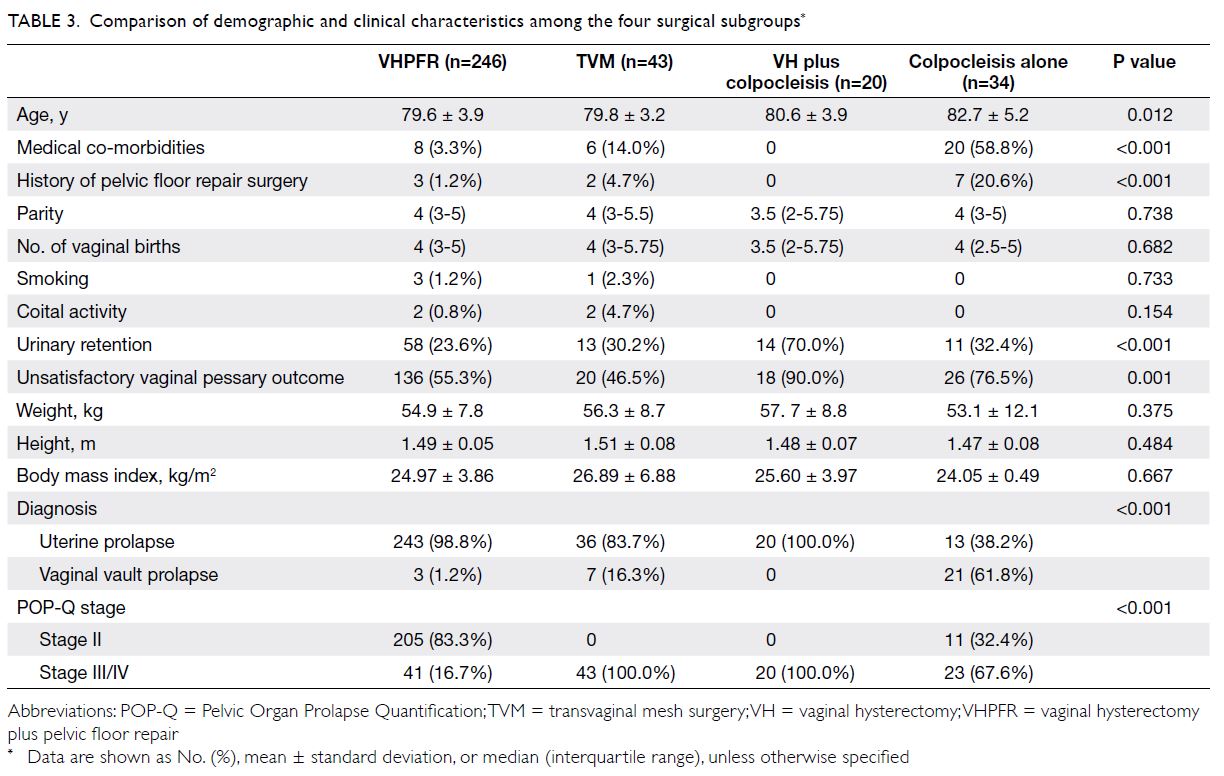
In total, 343 patients underwent surgery for POP
from 2013 to 2018 in the study hospitals. The types
of surgical treatment at each hospital are shown
in Table 1. Vaginal hysterectomy plus pelvic floor repair procedures were evenly distributed among all
four hospitals. However, 93% of TVM procedures,
95% of VH plus colpocleisis procedures, and 50%
of procedures comprising colpocleisis alone were
performed in Prince of Wales Hospital, Princess
Margaret Hospital, and Pamela Youde Nethersole
Eastern Hospital, respectively.
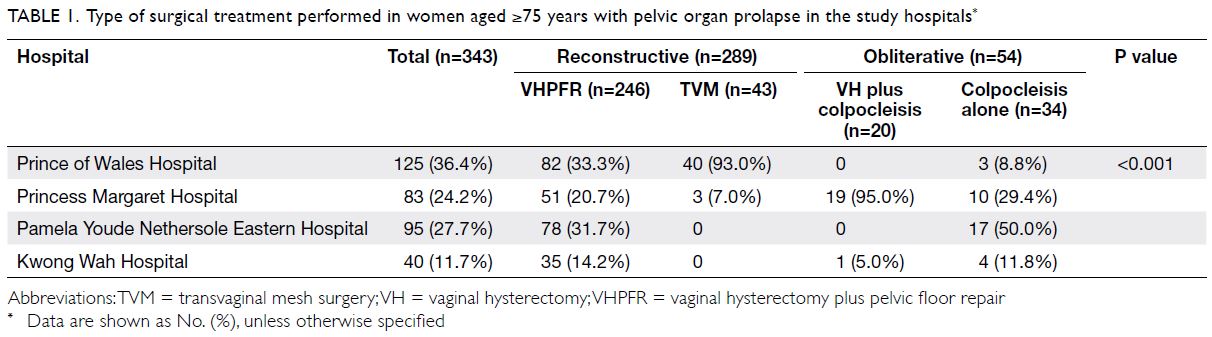
Table 1. Type of surgical treatment performed in women aged ≥75 years with pelvic organ prolapse in the study hospitals
Among the 343 patients, 216 (63%), 90 (26.2%),
and 37 (10.8%) had stages II, III, and IV POP,
respectively (Table 2). Furthermore, 289 (84.3%)
patients underwent reconstructive surgery and
54 (15.7%) patients underwent obliterative surgery.
Of the 289 reconstructive surgeries, 246 (71.7%) were
native tissue repair procedures (mainly VHPFR),
while 43 (12.5%) were TVM (36 had concomitant
VH); among the 54 obliterative surgeries, 20 (5.8%)
were colpocleisis plus VH, while the remaining
34 (9.9%) were colpocleisis alone (Table 3).
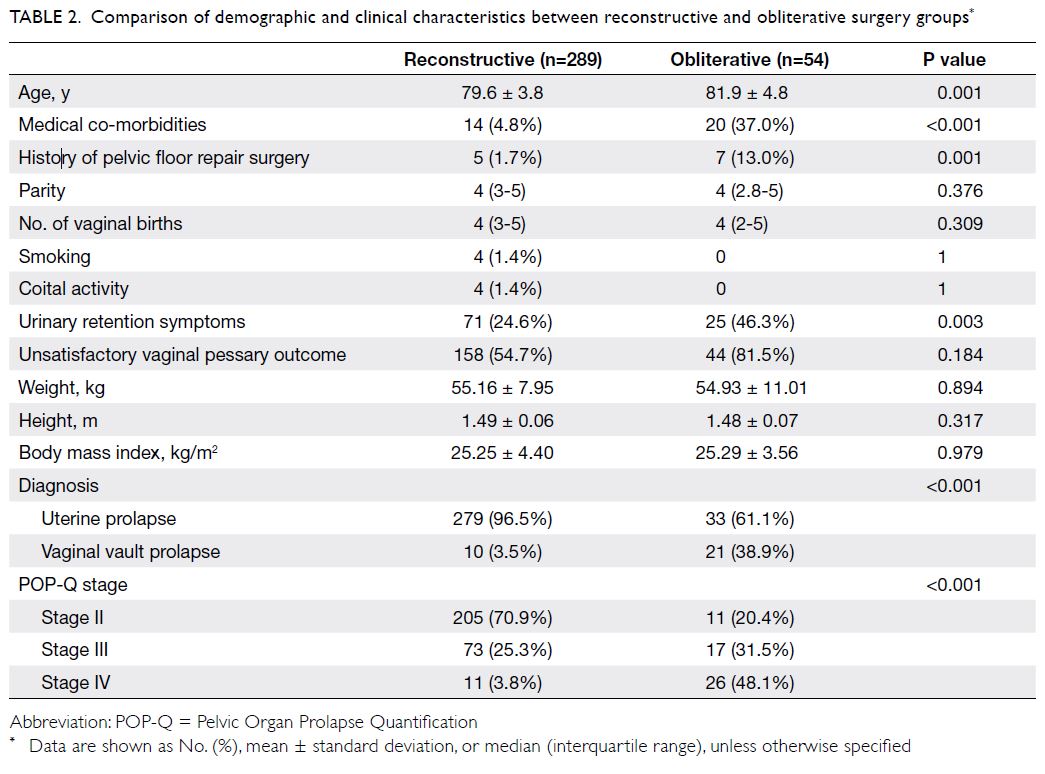
Table 2. Comparison of demographic and clinical characteristics between reconstructive and obliterative surgery groups
Table 2 compares demographic and clinical
characteristics between the reconstructive and
obliterative surgery groups. Patients with more
advanced age chose obliterative surgery, rather than
reconstructive surgery (81.9 vs 79.6 y; P=0.001).
Other variables including parity, number of vaginal
births, number of instrumental deliveries, body mass
index, smoking, and coital activity were comparable
between the two groups.
More patients with vaginal vault prolapse opted
for obliterative surgery, rather than reconstructive surgery (38.9% vs 3.5%; P<0.001) [Table 2]. The
difference was more striking when the colpocleisis
alone group was compared with all patients who
underwent reconstructive surgery (61.8%; P<0.001)
[Table 3]. Moreover, the number of patients who had
medical co-morbidities (eg, hypertension, diabetes
mellitus, heart disease, or history of stroke) was
greater in the obliterative surgery group than in the
reconstructive surgery group (37% vs 4.8%, P<0.001)
[Table 2].
Concerning patients with stage III/IV POP, more patients underwent TVM, rather than VHPFR,
in the reconstructive surgery group (100% vs 16.7%;
P<0.001); in the obliterative surgery group, more
patients with stage III/IV POP underwent VH plus
colpocleisis, rather than colpocleisis alone (100% vs
67.6%; P<0.004) [Table 3].
One case of carcinoma of the corpus uteri
(Ca corpus) was confirmed from the pathology report
of a patient who underwent VH. Thus, the incidence
of Ca corpus was 0.3% (1/312). The affected woman
was an asymptomatic patient in the TVM group; she
had incidental findings of endometrial thickening
during preoperative assessment. The results of
endometrial aspiration could not exclude a diagnosis
of hyperplasia. The patient underwent postoperative
contrast-enhanced computed tomography of the
abdomen and pelvis 2 months after surgery; there
were no signs of distant metastasis. After detailed
counselling, the patient refused further surgery or
adjuvant therapy. For 25 months of follow-up, the
patient’s cancer has remained in remission.
Table 4 shows surgical outcomes in both
groups and all subgroups. Compared with
obliterative surgeries, fewer reconstructive surgeries
were performed under spinal anaesthesia (57.4%
vs 38.1%; P=0.008). Notably, 76.5% of procedures comprising colpocleisis alone were performed under
spinal anaesthesia (P<0.001). Obliterative surgeries
had a shorter operative time (73.5 min vs 107 min;
P<0.001) and fewer surgical complications (9.3% vs
28.0%; P=0.003) than did reconstructive surgeries.
Among the four subgroups, colpocleisis alone had
the shortest operative time (60 min; P<0.001) and
least blood loss (50 mL; P<0.001).
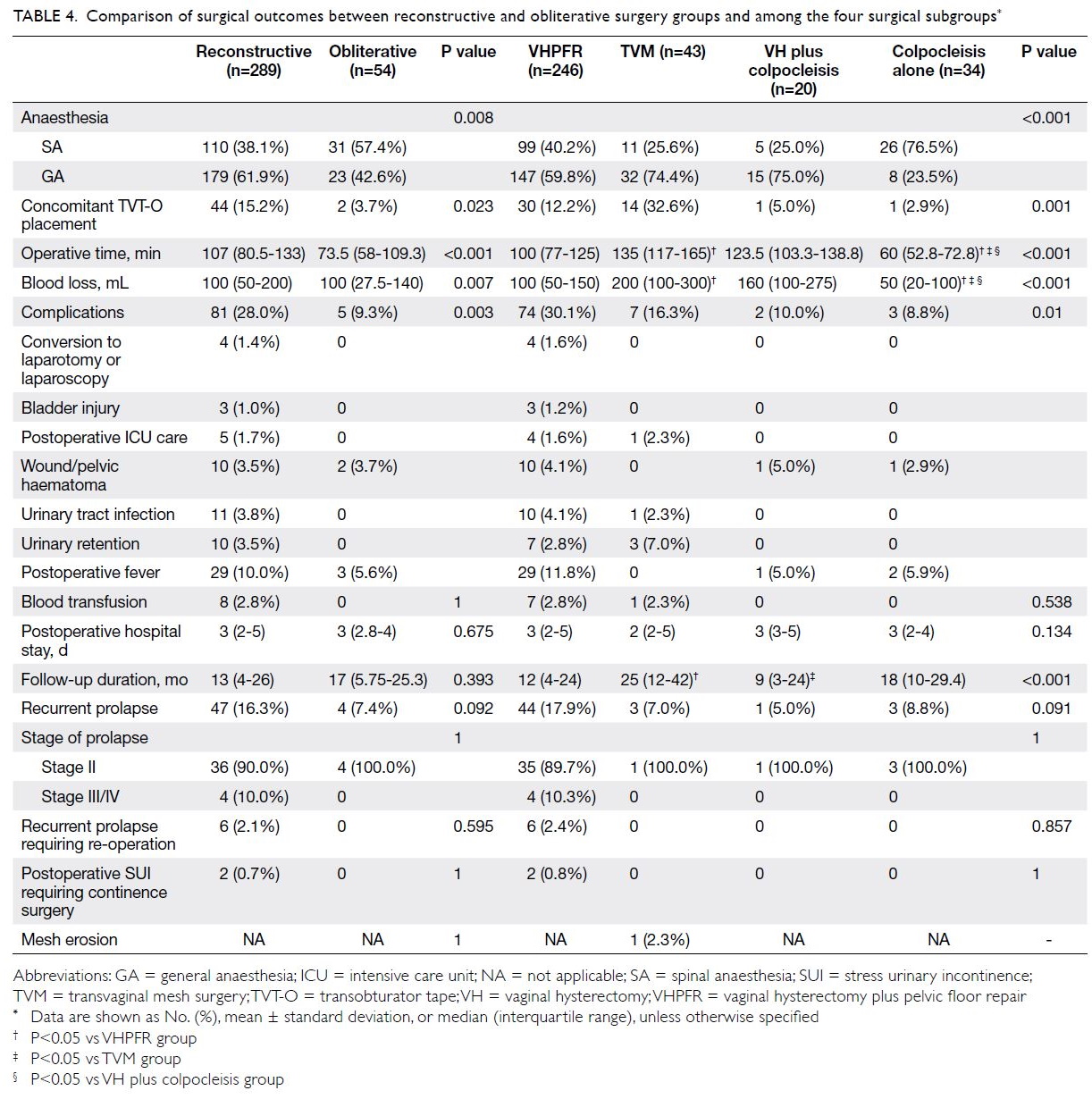
Table 4. Comparison of surgical outcomes between reconstructive and obliterative surgery groups and among the four surgical subgroups
Analysis of surgical complications (Table 4)
showed that the VHPFR group had the highest
intra- and peri-operative complication rate (30.1%;
P=0.01), compared with the other subgroups. In
the VHPFR group, four (1.6%) patients required
conversion to laparoscopy/laparotomy (two had
dense adhesion, one had large uterine size, and one
had difficulty achieving haemostasis). There were
three (1.2%) bladder injuries; all underwent primary
repair with good recovery and did not experience
long-term consequences. Four (1.6%) patients in the
VHPFR group required intensive care unit (ICU)
admission after surgery (one had fluid overload, one
had respiratory acidosis, one had cardiac problems,
and one had metabolic acidosis). In all, 29 (11.8%)
patients had fever of unknown cause; 90% of them
resolved by oral antibiotics. Ten (4.1%) patients had
postoperative wound or pelvic haematoma, and 10 (4.1%) patients had urinary tract infection. In
the TVM group, one (2.3%) patient required ICU
admission because of fluid overload, while three (7%)
patients had urinary retention after surgery. The VH
plus colpocleisis and colpocleisis alone groups both
included one patient with wound haematoma. In
the TVM group, 32.6% of patients had concomitant
TVT-O placement; 12.2%, 5%, and 2.9% of patients
had concomitant TVT-O placement in the VHPFR,
VH plus colpocleisis, and colpocleisis alone groups, respectively (P=0.001) [Table 4].
The median durations of follow-up were 13
and 17 months in the reconstructive and obliterative
surgery groups, respectively (Table 4). The TVM
group had a significantly longer median follow-up
duration (25 months; P<0.001); this was consistent
with the need to monitor any mesh complications.
There was only one patient was lost to follow-up
throughout the study period. Although there tended
to be fewer instances of recurrence in the obliterative surgery group than in the reconstructive surgery
group (7.4% vs 16.3%; P=0.092), the difference was
not statistically significant. There also tended to be
a higher rate of prolapse recurrence in the VHPFR
group than in the TVM, VH plus colpocleisis, or
colpocleisis alone groups (VHPFR 18%, TVM 7%,
VH plus colpocleisis 5%, and colpocleisis alone
8.8%), but this trend was not statistically significant
(P=0.091). Finally, few patients in each group
underwent surgery for prolapse recurrence or stress
urinary incontinence after surgery.
Discussion
To our knowledge, this is the first multicentre
retrospective study in Hong Kong concerning
POP surgery for women aged ≥75 years. Overall
analysis of demographic characteristics indicated
that most patients underwent VHPFR because the
largest proportion of patients had stage II POP.
Most patients were sexually inactive (only four of
343 patients reported sexual activity), multiparous
(median of four births overall), and had a history
of exclusively vaginal delivery. The mean body
mass index overall was 25.3 kg/m2. Compared with
reconstructive surgery, obliterative surgery was
more frequently selected by patients who were
older, had medical co-morbidities, had a history of
pelvic floor repair surgery, and had vaginal vault
prolapse.
In this study, we found that surgical treatment
was a safe option for older women who sought
to improve their quality of life. The postoperative
mortality rate was zero, consistent with the low
mortality rate 4.1% in a previous study.4 Notably,
prior studies10 11 in Chinese populations suggested
that poor quality of life and complications associated
with vaginal pessary management lead to an
increased likelihood of surgical treatment. In our
study, over 80% of patients in the obliterative surgery
group had an unsatisfactory vaginal pessary outcome;
nearly half of the patients also had urinary retention.
Therefore, it is reasonable that these patients chose
POP surgery, despite their advanced age.
In studies from other countries, the reported
rates of surgical complications associated with POP
surgery in women aged ≥75 years were 30% to 40%.12 13
Although the VHPFR group had the highest rate of
surgical complications among all subgroups in the
present study, the rate of 30.1% was comparable to
the rates in studies from other countries. However,
1.7% of patients in the reconstructive surgery group
were admitted to the ICU after surgery; this was
higher than the reported rate of 0.45% in a large
cohort study with a mean patient age of 62.7 years.14
Because older women are more likely to experience
fluid overload—it was present in 40% of the patients
who required postoperative ICU care in our study—perioperative fluid replacement should be cautiously administered.
Patients in the obliterative surgery group had
fewer surgical complications than did patients in
the reconstructive surgery group. When the four
types of surgeries were compared, the proportion
of surgeries performed under spinal anaesthesia
was greatest for procedures comprising colpocleisis
alone; these procedures also had the least blood loss,
shortest operative time, and fewest complications.
Furthermore, the hospital stay in the colpocleisis
alone group was comparable with the lengths in other
groups, although significantly larger proportions of
patients in the colpocleisis alone group had medical
co-morbidities and were older.
Theoretically, colpocleisis with concomitant
VH is superior to colpocleisis alone because it
avoids the possibility of missing Ca corpus during
surgery or later in the patient’s life15 16; however,
it is associated with a longer operative time and
increased blood loss.17 18 Our results were consistent
with the findings in previous studies from other
countries. Patients aged ≥75 years are beyond the
peak incidence of Ca corpus: according to the Hong
Kong Cancer Registry, the median age of patients
with Ca corpus is 55 years.19 In the present study, one
patient in the TVM group had Ca corpus; thus, the
rate of incidental malignancy was 0.3%, which was
comparable to the rate of 0.26% previously reported
in Hong Kong.20 Currently, pelvic ultrasound is not
a routine component of preoperative assessment. To
reduce the risk of missing Ca corpus, preoperative
transvaginal ultrasound (to assess endometrial
thickness) and endometrial aspiration should be
considered in women who have abnormal vaginal
bleeding or plan to undergo uterine-preserving
surgery.20
Although TVM is a more complex surgery
than VHPFR, the rate of perioperative surgical
complications was lower in the TVM group; hospital
stays were comparable between the two groups.
However, the operative time was longer and blood
loss was greater in the TVM group. Compared
with patients in the VHPFR group, patients in the
TVM group had a lower rate of POP recurrence (all
recurrences occurred in patients with stage III/IV
POP) and a significantly longer follow-up duration.
The mesh erosion rate in this study (2.3%) was
lower than in another study in Hong Kong (8.9%),
which had a longer follow-up duration of 40 months
and included younger patients.21 When proper
counselling is provided, TVM is a safe option for
healthier patients with stage III/IV POP because
stage III/IV POP is a risk factor for recurrence.22
Strengths and limitations
Notable strengths of this study included its multicentre design and focus on POP surgery among
older women in the Hong Kong Chinese population,
which has not been previously explored. Patients in
this study included all women aged ≥75 years who
underwent POP surgery in a 6-year period at four
hospitals; these hospitals are jointly accredited as
a single urogynaecological training centre under
the Hong Kong College of Obstetricians and
Gynaecologists, and they have extensive experience
performing all types of POP surgery (Table 1).
Furthermore, the electronic medical record system
of the Hospital Authority facilitated complete data
collection and retrieval. However, there were a few
limitations in this study. First, it was a retrospective
study. Second, we did not perform quality of life
assessment or investigate the presence of guilt
concerning colpocleisis surgery. Because few patients
reported sexual activity before surgery, we presume
that most older women in Hong Kong would not
regret the selection of colpocleisis because of its
effects on sexual activity. Third, although the median
follow-up period was <18 months, it may have been
insufficient to fully characterise prolapse recurrence
and gynaecological malignancy. Finally, the levels of
independence and family support may be important
factors for older women to consider before making
any surgical decision; however, we did not have
access to such data. These factors could be examined
in future studies.
Conclusion
This multicentre retrospective study showed that
multiple types of POP surgeries were safe and
effective for women aged ≥75 years. Most surgical
complications were self-limiting and the recurrence
rate was low. The excellent results suggest that
colpocleisis may be appropriate as primary surgery
for fragile older women. These findings will facilitate
preoperative counselling for older women with POP
who are considering surgical treatment.
Author contributions
Concept or design: D Wong, SSC Chan
Acquisition of data: All authors.
Analysis or interpretation of data: D Wong, SSC Chan.
Drafting of the article: D Wong, SSC Chan.
Critical revision for important intellectual content: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: D Wong, SSC Chan.
Drafting of the article: D Wong, SSC Chan.
Critical revision for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
We would like to express our gratitude to Ms LL Lee, Dr TH Chan and Dr CW Chu for data collection and entry.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This study was approved by the Hong Kong East Cluster Ethics
Committee (HKECREC-2020-069), the Kowloon Central
Cluster Ethics Committee (KC/KE-20-0223/ER-2), the
Kowloon West Cluster Ethics Committee (EX-20-108[150-02]), and the New Territories East Cluster Ethics Committee
(NTEC-2020-138).
References
1. Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL.
Epidemiology of surgically managed pelvic organ prolapse
and urinary incontinence. Obstet Gynecol 1997;89:501-6. Crossref
2. Smith FJ, Holman CD, Moorin RE, Tsokos N. Lifetime risk
of undergoing surgery for pelvic organ prolapse. Obstet
Gynecol 2010;116:1096-100. Crossref
3. Griebling TL. Vaginal pessaries for treatment of pelvic
organ prolapse in elderly women. Curr Opin Urol
2016;26:201-6. Crossref
4. Sung VW, Weitzen S, Sokol ER, Rardin CR, Myers DL.
Effect of patient age on increasing morbitity and mortality
following urogynecologic surgery. Am J Obstet Gynecol
2006;194:1411-7. Crossref
5. World Health Organization. Global recommendations
on physical activity for health. 2010. Available from:
https://www.who.int/publications/i/item/9789241599979.
Accessed 21 Mar 2022.
6. Hospital Authority, Hong Kong SAR Government. Strategic
service framework for elderly patients. 26 April 2012.
Available from: https://www.ha.org.hk/ho/corpcomm/Strategic%20Service%20Framework/Elderly%20Patients.pdf. Accessed 21 Mar 2022.
7. Kong TK. Hospital service for the elderly in Hong Kong—present and future. J Hong Kong Geriatr Soc 1990;1:16-20.
8. Haylen BT, Maher CF, Barber MD, et al. An International
Urogynecological Association (IUGA)/International
Continence Society (ICS) joint report on the terminology
for female pelvic organ prolapse (POP). Int Urogynecol J
2016;27:165-94. Crossref
9. Toozs-Hobson P, Freeman R, Barber M, et al. An
International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the
terminology for reporting outcomes of surgical procedures
for pelvic organ prolapse. Int Urogynecol J 2012;23:527-35. Crossref
10. Chan SS, Cheung RY, Yiu AK, et al. Chinese validation
of pelvic floor distress inventory and pelvic floor impact
questionnaire. Int Urogynecol J 2011;22:1305-12. Crossref
11. Chan SS, Cheung RY, Yiu KW, Lee LL, Pang AW,
Chung TK. Symptoms, quality of life, and factors affecting
women’s treatment decisions regarding pelvic organ
prolapse. Int Urogynecol J 2012;23:1027-33. Crossref
12. Friedman WH, Gallup DG, Burke JJ 2nd, Meister EA,
Hoskins WJ. Outcomes of octogenarians and
nonagenarians in elective major gynecologic surgery. Am
J Obstet Gynecol 2006;195:547-52. Crossref
13. Stepp KJ, Barber MD, Yoo EH, Whiteside JL, Paraiso MF,
Walters MD. Incidence of perioperative complications of
urogynecologic surgery in elderly women. Am J Obstet
Gynecol 2005;192:1630-6. Crossref
14. Mairesse S, Chazard E, Giraudet G, Cosson M, Bartolo S.
Complications and reoperation after pelvic organ prolapse,
impact of hysterectomy, surgical approach and surgeon
experience. Int Urogynecol J 2020;31:1755-61. Crossref
15. Elkattah R, Brooks A, Huffaker RK. Gynecologic
malignancies post-lefort colpocleisis. Case Rep Obstet
Gynecol 2014;2014:846745. Crossref
16. Frick AC, Walters MD, Larkin KS, Barber MD. Risk of
unanticipated abnormal gynecologic pathology at the time
of hysterectomy for uterovaginal prolapse. Am J Obstet
Gynecol 2010;202:507.e1-4. Crossref
17. FitzGerald MP, Richter HE, Siddique S, Thompson P,
Zyczynski H, Ann Weber for the Pelvic Floor Disorders
Network. Colpocleisis: a review. Int Urogynecol J Pelvic
Floor Dysfunct 2006;17:261-71. Crossref
18. Bochenska K, Leader-Cramer A, Mueller M, Davé B,
Alverdy A, Kenton K. Perioperative complications following colpocleisis with and without concomitant
vaginal hysterectomy. Int Urogynecol J 2017;28:1671-5.Crossref
19. Hong Kong Cancer Registry, Hospital Authority, Hong
Kong SAR Government. Cancer in 2018. Available from:
https://www3.ha.org.hk/cancereg/pdf/factsheet/2018/corpus_2018.pdf. Accessed 29 Dec 2020.
20. Wan OY, Cheung RY, Chan SS, Chung TK. Risk of
malignancy in women who underwent hysterectomy for
uterine prolapse. Aust N Z J Obstet Gynaecol 2013;53:190-6. Crossref
21. Wan OY, Chan SS, Cheung RY, Chung TK. Mesh-related
complications from reconstructive surgery for pelvic organ
prolapse in Chinese patients in Hong Kong. Hong Kong
Med J 2018;24:369-77. Crossref
22. Friedman T, Eslick GD, Dietz HP. Risk factors for prolapse
recurrence: systematic review and meta-analysis. Int
Urogynecol J 2018;29:13-21. Crossref