Hong Kong Med J 2022 Feb;28(1):76–8 | Epub 14 Feb 2022
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Paediatric multisystem inflammatory syndrome
temporally associated with SARS-CoV-2: a case report
Gilbert T Chua, MB, BS, FHKAM (Paediatrics)1 †; Joshua SC Wong, MB, BS, FHKAM (Paediatrics)2 † Jaime Chung, MB, BS2; Ivan Lam, FHKCP, FHKAM (Paediatrics)2; Joyce Kwong, FHKAM (Pathology)3; Kate Leung, FRCPA, FHKAM (Pathology)3; CY Law, PhD, FHKAM (Pathology)4; CW Lam, PhD, FRCP5; Janette Kwok, PhD, FRCPA6; Patrick WK Chu, MPhil6; Elaine YL Au, FRCPA, FHKCPath7; Crystal K Lam, MB, BS7; Daniel Mak, MRCPCH, FHKAM (Paediatrics)2; NC Fong, FRCPCH2; Daniel Leung, PhD (Candidate)1; Wilfred HS Wong, PhD1; Marco HK Ho, MDM, FRCP1; Sabrina SL Tsao, MB, BS, FACC1; Christina S Wong, MRCP, FHKAM (Medicine)8; Jason C Yam, MB, BS, FCOphthHK,9; Winnie WY Tso, FHKAM (Paediatrics)1; Kelvin KW To, MD, FRCPath10; Paul KH Tam, FRCS, FRCPCH11,12Godfrey CF Chan, MD, FRCPCH1; WH Leung, MB, BS, PhD1; KY Yuen, MD, FRCPath10; Vas Novelli, FRCP, FRCPCH13,14; Nigel Klein, PhD13,14; Michael Levin, PhD, FRCPCH15; Elizabeth Whitaker, MRCPCH, PhD16; YL Lau, MD (Hon), FRCPCH1; Patrick Ip, MPH, FHKAM (Paediatrics)1; Mike YW Kwan, MRCPCH, MSc (Applied Epidemiology CUHK)2
1 Department of Paediatrics and Adolescent Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong
2 Department of Paediatrics and Adolescent Medicine, Princess Margaret Hospital, Hong Kong
3 Haematology Laboratory, Department of Pathology, Princess Margaret Hospital, Hong Kong
4 Division of Chemical Pathology, Department of Pathology, Queen Mary Hospital, Hong Kong
5 Department of Pathology, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong
6 Division of Transplantation and Immunogenetics, Department of Pathology, Queen Mary Hospital, Hong Kong
7 Division of Clinical Immunology, Department of Pathology, Queen Mary Hospital, Hong Kong
8 Division of Dermatology, Department of Medicine, Queen Mary Hospital, Hong Kong
9 Department of Ophthalmology and Visual Sciences, Chinese University of Hong Kong, Hong Kong
10 Department of Microbiology, Carol Yu Centre for Infection, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong
11 Division of Paediatric Surgery, Department of Surgery, The University of Hong Kong, Hong Kong
12 Dr Li Dak-Sum Research Centre, The University of Hong Kong–Karolinska Institutet Collaboration in Regenerative Medicine, The University of Hong Kong, Hong Kong
13 Department of Paediatric Infectious Diseases, Great Ormond Street Hospital for Children, London, United Kingdom
14 Institute of Child Health, University College London, London, United Kingdom
15 Section of Paediatrics, Imperial College London, London, United Kingdom
16 Paediatric Infectious Diseases Department, Imperial College Healthcare NHS Trust, London, United Kingdom
† Co-first authors
Corresponding author: Dr Mike YW Kwan (kwanyw1@ha.org.hk)
Case report
A 10-year-old ethnic-Russian boy was confirmed to
have severe acute respiratory syndrome coronavirus
2 (SARS-CoV-2) during the second wave of the
coronavirus disease 2019 (COVID-19) outbreak
in Hong Kong.1 He had a past medical history of
coarctation of the aorta with corrective surgery
performed at age 2 months. He returned from Russia
on 6 June 2020 and his first deep throat saliva specimen
saved on arrival at Hong Kong International Airport
tested negative for SARS-CoV-2. Four days later, he
developed fever, malaise, and headache. On 13 June
2021, he was admitted to our Paediatric Infectious
Disease Unit and a new deep throat saliva specimen
was positive for SARS-CoV-2. He did not require
oxygen during his hospital stay. He was discharged
from the hospital after being tested positive for
SARS-CoV-2 anti-nucleoprotein immunoglobulin G
antibodies 17 days after admission. This complied with the discharge criteria set by the Department
of Health, the Government of Hong Kong Special
Administrative Region.1
On 16 July, 16 days after being discharged, he
returned to our Paediatric Infectious Disease Unit
with a 2-day history of high fever and right cervical
tender lymphadenopathy. Repeat nasal pharyngeal
swab for SARS-CoV-2 polymerase chain reaction
was negative. He was presumed to have bacterial
lymphadenitis and was prescribed intravenous
antibiotics but symptoms progressed. Ultrasound
of the neck showed evidence of lymphadenitis
but no signs of abscess formation. His fever and
lymphadenitis persisted for 5 days and he also
developed bilateral non-purulent conjunctivitis
with peri-limbic sparing, erythematous and cracked
lips, strawberry tongue and blanchable erythema
over the trunk (Fig). Serial blood tests showed mild
thrombocytopenia (trough 110 × 109/L), and raised erythrocyte sedimentation rate (peak 60 mm/Hr),
C-reactive protein (peak 102 mg/L; range, <5.0),
lactate dehydrogenase (270 U/L; range, <270),
ferritin (1568 pmol/L; range, 31-279), highly sensitive
troponin I (peak 643 ng/L; range, <21), N-terminal
prohormone of brain natriuretic peptide (peak
3213 ng/L; range, <112), and interleukin-6 (IL-6)
(peak 480.9 pg/mL; range, <4). Electrocardiogram
and echocardiogram were unremarkable. His clinical
presentation was compatible with Kawasaki-like
disease. Since he had been infected with COVID-19
approximately 4 weeks previously, he was suspected to
have PIMS-TS (paediatric multisystem inflammatory
syndrome temporally associated with SARS-CoV-2).2
Other differential diagnoses were excluded but
included streptococcal and staphylococcal infection,
Epstein–Barr virus infection and infection-related
myocarditis. Owing to the rarity of PIMS-TS in
East Asia, the clinical team discussed the case with
experts from the United Kingdom who concurred
with the diagnosis. He was treated with two doses of
intravenous immunoglobulin (IVIG) at 2 g/kg/dose
as his fever resurged 1 day after the first dose. Fever
and other symptoms subsequently subsided after the
second dose of IVIG, and serial echocardiograms
did not reveal any coronary lesions. Whole exome
sequencing performed to look for the possibility of
an underlying monogenic immune dysregulation syndrome because of the rarity of this condition was unremarkable.
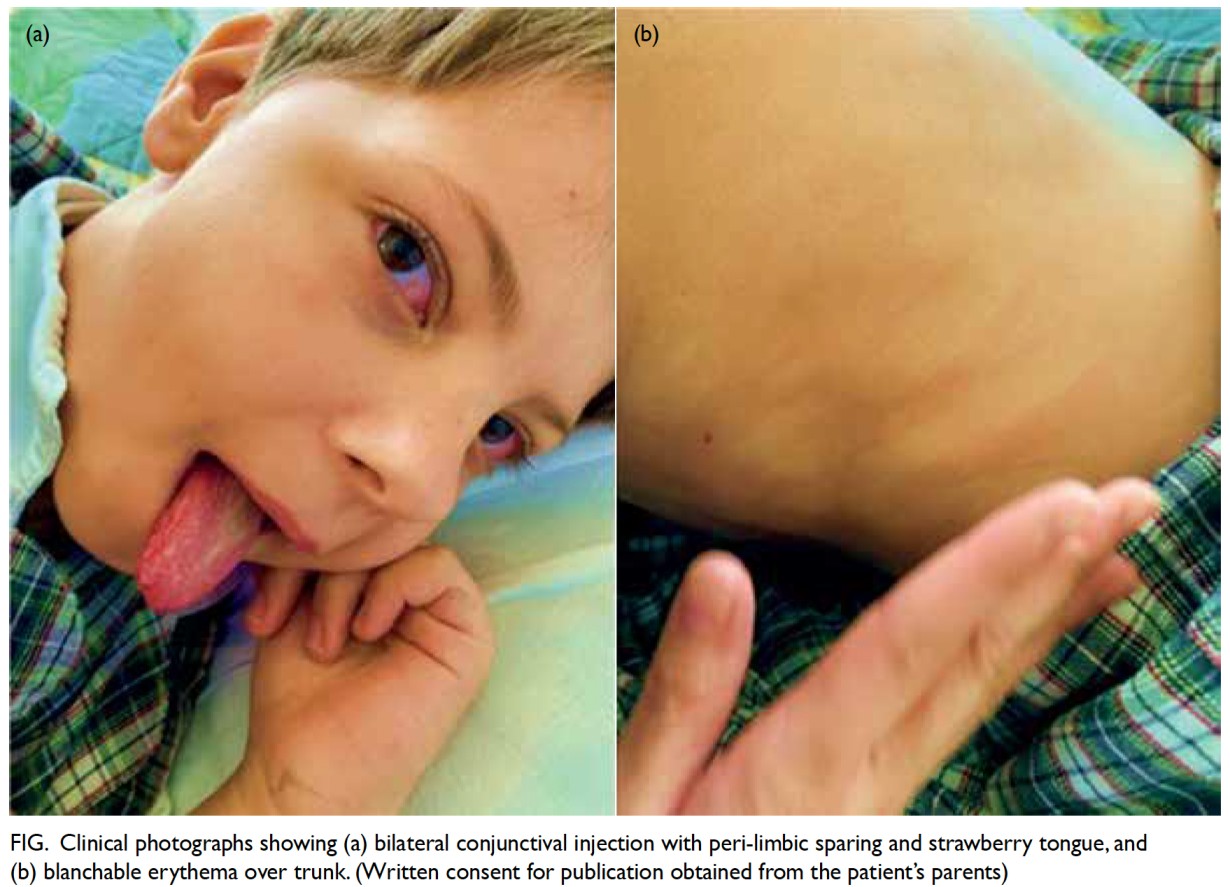
Figure. Clinical photographs showing (a) bilateral conjunctival injection with peri-limbic sparing and strawberry tongue, and (b) blanchable erythema over trunk. (Written consent for publication obtained from the patient’s parents)
Discussion
Paediatric multisystem inflammatory syndrome
temporally associated with SARS-CoV-2 is one of the
most severe complications of COVID-19 infection
in children. It was initially described in several case
series in Europe and North America among children
who presented with Kawasaki-like illness and
were confirmed or known to have been in contact
with another SARS-CoV-2–infected individual.2 3
Kawasaki disease (KD) is most prevalent among
East Asians but rare in other parts of the world.3
On the contrary, paediatric cross-sectional clinical
studies from East Asia have reported that PIMS-TS
is rare among East Asians.1 We present the first, and
so far, the only case of PIMS-TS in China. The case
was an ethnic Russian boy who showed features of
KD approximately 4 weeks after confirmation of
SARS-CoV-2 infection. There is no consensus on the
treatment regimen at present. In our patient, IVIG
alone, instead of steroid or immunomodulators, was
effective in treating the condition.
The pathophysiology of PIMS-TS remains
uncertain. Studies have shown significant clinical
and laboratory differences between PIMS-TS and KD, despite some similarities in clinical
presentation. Patients with PIMS-TS are generally
older than those with KD (median age, 8.3-9 years vs
2.7 years).2 3 They also have a higher white blood cell
and neutrophil count and C-reactive protein, and
a greater degree of lymphopenia and anaemia and
tendency to develop thrombocytopenia in contrast
to thrombocytosis in KD. In addition, fibrinogen
and troponin levels are more elevated in PIMS-TS.2
These factors are associated with an increased risk
of intensive care admission among children with
PIMS-TS.2 These findings imply that PIMS-TS is
a different entity to KD, with a greater degree of
inflammation and myocardial injury. Studies have
shown that certain cytokines, such as IL-6, appear
to be particularly elevated in patients with PIMS-TS
and may be involved in myocardial depression.2
Studies have also suggested that life-threatening
COVID-19 pneumonia may be associated with
monogenic inborn errors of immunity related
to type 1 interferonopathies or type 1 interferon
neutralising antibodies.4 Certain human leukocyte
antigens, which are prevalent in East Asians but
not Caucasians, have been associated with KD.4
However, no genes have been identified to cause
PIMS-TS. Future studies will continue to explore the
genetic factors related to PIMS-TS and the possible
associated leukocyte antigen that explains the ethnic
differences in PIMS-TS prevalence.
The treatment for PIMS-TS is similar to that for
KD. A recent observational study demonstrated that
patients who received IVIG and methylprednisolone
together were less likely to require second-line
biological agents, and were at lower risk of secondary
acute left ventricular dysfunction and need for
haemodynamic support with a shorter length of stay
in the intensive care unit.5 Interleukin-1 and IL-6
receptor monoclonal antibodies have been used as
second-line biological agents and have been shown
to achieve remission when first-line therapies fail.2 5
Short-term outcomes of PIMS-TS are generally good.
Immediate cardiac complications include coronary
abnormalities, transient valvular regurgitation and
myocardial dysfunction.2 The majority of patients
recover without sequelae, but mortality has been
reported.2 Data on the long-term outcomes of
PIMS-TS are lacking.
The PIMS-TS remains a rare disease among
East Asian patients.1 Nevertheless, frontline
paediatricians in East Asia should remain vigilant
when looking after ethnic non-East Asian children
with COVID-19 infection in case they develop
PIMS-TS after their initial recovery. Paediatricians
should advise parents about the symptoms and signs of PIMS-TS so that timely medical consultation can be sought.
Author contributions
Concept or design: GT Chua, JSC Wong, P Ip, MYW Kwan.
Acquisition of data: J Chung, I Lam, J Kwong, K Leung, CY Law, CW Lam, J Kwok, PWK Chu, EYL Au, CK Lam, MYW Kwan.
Analysis or interpretation of data: D Mak, NC Fong, D Leung, WHS Wong, MHK Ho, SSL Tsao, CS Wong, JC Yam, WWY Tso, KKW To, PKH Tam, GCF Chan, WH Leung, KY Yuen, V Novelli, N Klein, M Levin, E Whitaker, YL Lau.
Drafting of the manuscript: GT Chua, JSC Wong, I Lam, J Chung.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: J Chung, I Lam, J Kwong, K Leung, CY Law, CW Lam, J Kwok, PWK Chu, EYL Au, CK Lam, MYW Kwan.
Analysis or interpretation of data: D Mak, NC Fong, D Leung, WHS Wong, MHK Ho, SSL Tsao, CS Wong, JC Yam, WWY Tso, KKW To, PKH Tam, GCF Chan, WH Leung, KY Yuen, V Novelli, N Klein, M Levin, E Whitaker, YL Lau.
Drafting of the manuscript: GT Chua, JSC Wong, I Lam, J Chung.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This work was supported by the Collaborative Research Fund
(CRF) 2020/21 and One-off CRF Coronavirus and Novel
Infectious Diseases Research Exercises (Ref: C7149-20G).
The funding source was not involved in the study design,
collection, analysis or interpretation of data; in the writing of
the manuscript; or in the decision to submit the manuscript
for publication.
Ethics approval
The patient was treated in accordance with the Declaration of Helsinki, and the parents of the patient provided informed
consent for the treatment and procedures.
References
1. Chua GT, Wong JS, Lam I, et al. Clinical characteristics and
transmission of COVID-19 in children and youths during
3 waves of outbreaks in Hong Kong. JAMA Netw Open
2021;4:e218824. Crossref
2. Whittaker E, Bamford A, Kenny J, et al. Clinical
characteristics of 58 children with a pediatric
inflammatory multisystem syndrome temporally associated
with SARS-CoV-2. JAMA 2020;324:259-69. Crossref
3. To KK, Chua GT, Kwok KL, et al. False-positive SARS-CoV-2
serology in 3 children with Kawasaki disease. Diagn
Microbiol Infect Dis 2020;98:115141. Crossref
4. Sancho-Shimizu V, Brodin P, Cobat A, et al. SARS-CoV-2-r
elated MIS-C: A key to the viral and genetic causes of
Kawasaki disease? J Exp Med 2021;218:e20210446.
5. Ouldali N, Toubiana J, Antona D, et al. Association of
intravenous immunoglobulins plus methylprednisolone vs
immunoglobulins alone with course of fever in multisystem
inflammatory syndrome in children. JAMA 2021;325:855-64.Crossref

