Hong Kong Med J 2021 Dec;27(6):405–12 | Epub 17 Dec 2021
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE CME
Effectiveness of a childbirth massage programme for labour pain relief in nulliparous pregnant women at term: a randomised controlled trial
CY Lai, MSc (Endocrinology, Diabetes and Metabolism), MSc Nursing (Midwifery)1; Margaret KW Wong, MSc (Women’s Health Studies)2; WH Tong, MSc (Public Health)2; SY Chu, MN (Clinical Leadership); BSc (Health Science)3; KY Lau, MSc (Women’s Health Studies)2; Agnes ML Tam, MSc (Women’s Health Studies)2; LL Hui, PhD (Community Medicine)4; Terence TH Lao, MD, FRCOG1; TY Leung, MB, ChB, MD1
1 Department of Obstetrics and Gynaecology, The Chinese University of Hong Kong, Hong Kong
2 Department of Obstetrics and Gynaecology, Prince of Wales Hospital, Hong Kong
3 Department of Obstetrics and Gynaecology, Kwong Wah Hospital, Hong Kong
4 Department of Paediatrics, The Chinese University of Hong Kong, Hong Kong
Corresponding author: Ms CY Lai (cylai@cuhk.edu.hk)
Abstract
Introduction: The effect of massage for pain relief
during labour has been controversial. This study
investigated the efficacy of a programme combining
intrapartum massage, controlled breathing, and
visualisation for non-pharmacological pain relief
during labour.
Methods: This randomised controlled trial was
conducted in two public hospitals in Hong Kong.
Participants were healthy low-risk nulliparous
Chinese women ≥18 years old whose partners were
available to learn massage technique. Recruitment
was performed at 32 to 36 weeks of gestation;
women were randomised to attend a 2-hour
childbirth massage class at 36 weeks of gestation or
to receive usual care. The primary outcome variable
was the intrapartum use of epidural analgesia or
intramuscular pethidine injection.
Results: In total, 233 and 246 women were
randomised to the massage and control groups,
respectively. The use of epidural analgesia or
pethidine did not differ between the massage and
control groups (12.0% vs 15.9%; P=0.226). Linear-by-linear analysis demonstrated a trend whereby
fewer women used strong pharmacological pain
relief in the massage group, and a greater proportion
of women had analgesic-free labour (29.2% vs 21.5%;
P=0.041). Cervical dilatation at the time of pethidine/epidural analgesia request was significantly greater in the massage group (3.8 ± 1.7 cm vs 2.3 ± 1.0 cm;
P<0.001).
Conclusion: The use of a massage programme appeared to modulate pain perception in labouring
women, such that fewer women requested epidural
analgesia and a shift was observed towards the use
of weaker pain relief modalities; in particular, more
women in the massage group were analgesic-free
during labour.
New knowledge added by this study
- In this randomised controlled trial of healthy low-risk nulliparous Chinese women, fewer women used strong pharmacological pain relief in the childbirth massage group, and a greater proportion of women had analgesicfree labour, compared with the control group.
- Cervical dilatation at the time of pethidine/epidural analgesia request was significantly greater in the childbirth massage group than in the control group.
- A structured childbirth massage programme delivered by qualified midwife trainers can provide couples with both theoretical knowledge and practical skills, which help to modulate pain perception among labouring women.
- With appropriate training, massage can be an efficacious option for labour pain relief with no associated adverse effects on delivery.
Introduction
Labour is regarded as a time of suffering in a
woman’s life, during which she may experience intensive pain that lasts for many hours. Ineffective
labour pain management could create a negative
life experience for a woman, which may negatively impact postpartum sexual and marital satisfaction.1 2
Labour pain involves both physical and psychological
elements such as uterine contractions, tension, fear,
anxiety, and the sensations of powerlessness and a
loss of control.3 Current remedies for labour pain
include pharmacological and non-pharmacological
interventions. The most common pharmacological
interventions include nitrous oxide inhalation,
the injection of narcotic analgesics (eg, pethidine),
and epidural analgesia. However, these methods
are associated with adverse effects such as nausea
and vomiting, longer first and second stages of
labour, hypotension, motor blockade, fever, and
urinary retention; they can also lead to neonatal
respiratory depression and newborn sleepiness
that affects breastfeeding.4 5 6 7 8 9 Hence, women prefer
safer and simpler non-pharmacological pain relief
methods.10 11
A notable non-pharmacological remedy is
massage, which may provide pain relief to the site
of application, along with overall psychological
relaxation.12 The pressure applied during massage
is presumed to block the transmission of pain
impulses to the brain, while stimulating local
release of endorphins.13 Randomised controlled
trials concerning intrapartum massage have been
conducted in various countries over the past two
decades.12 14 15 16 17 18 19 20 21 22 23 However, there have been conflicting
findings concerning beneficial effects (ie, reductions
in pain score or the use of pharmacological
analgesia)12 14 15 16 17 21 because of small sample sizes which ranged from 28 women12 to 176 women.21
Furthermore, the duration of intrapartum massage
was either unspecified15 21 or lasted for only 30 to
40 minutes.12 14 18 19 22 23 In addition, intrapartum
massage was performed by various types of people:
student midwives,22 therapists17 19 or partners who
had received training by therapists immediately
before labour.12 14 These factors probably influenced
the effectiveness, consistency, and duration of the
application of massage. A recent Cochrane review
concluded that the current quality of evidence
regarding intrapartum massage is low to very
low.24 Therefore, this randomised controlled study
investigated the efficacy of a comprehensive massage
programme, combined with controlled breathing
and visualisation—all initiated during the antenatal
period—as a non-pharmacological pain relief
method during labour, with the goal of reducing
pethidine or epidural analgesia use.
Methods
Design and recruitment
This randomised controlled study was conducted
in two public hospitals in Hong Kong, where
the midwives were responsible for intrapartum
management and natural vaginal delivery of low-risk
pregnancies. The respective annual childbirth rates
were approximately 5000 and 7000; the caesarean
section rates were 21% and 23%.25 Recruitment
commenced in September 2016 and completed in
December 2017. The recruitment of women was
conducted at 32 to 36 weeks of gestation during
their routine antenatal visit by a team of research
midwives. The inclusion criteria were low-risk
nulliparous Chinese women aged ≥18 years,
who could communicate in Cantonese, and who
carried a singleton pregnancy without known
contraindications for vaginal delivery. Exclusion
criteria were the use of massage among women in
the control group, the absence of a partner to learn
the massage technique, planned delivery in hospitals
other than the study sites, and planned caesarean
delivery. There was no exclusion of recruited
women who attempted vaginal delivery or induction
of labour but eventually required intrapartum
caesarean delivery.
Randomisation was conducted via two-by-two
blocking with a block size of 4; a computer-generated
number indicating either the study or
control group was sealed in an opaque envelope.
After a woman had provided written informed
consent to participate, the midwife revealed the
group allocation by opening the envelope. Because
there were multiple midwifery staff responsible for
participant recruitment at different occasions, none
of the staff were aware of the allocation of previous
participants; hence, they were unable to guess the
group allocation.
Intervention
Couples (ie, participating women and their partners)
randomised to the massage group were invited to
attend a 2-hour childbirth massage programme
class at 36 weeks of gestation. This programme
was based on the United Kingdom’s Royal College
of Midwives accredited course ‘Towards Natural
Childbirth and Beyond’.26 It included a 30-minute
theoretical explanation of the evidence
underpinning the childbirth massage programme,
followed by a 90-minute practicum. During the
90-minute practicum, the couples received training
by accredited midwifery trainers with respect to
the massage technique, controlled breathing, and
visualisation, in accordance with the methods used
in previous studies.16 20 The massage areas included
the lower back and four limbs. Couples were taught
how to synchronise the massage strokes with slow
rhythmic breathing. Visualisation (ie, a mind
mapping component) was also taught.26 In this
process, the woman was asked to imagine something
comfortable, which could bring her to a relaxed
state. Subsequently, the couples were encouraged to
practise the massage technique regularly at home in
the evening, in a dimly lit and quiet environment,
with the aim of encouraging relaxation and
improving the quality and duration of sleep.27 The
control group received standard antenatal education
without instruction concerning massage, controlled
breathing, or visualisation techniques.
When a woman in the massage group was
admitted to the study hospital at onset of labour
or for planned labour induction, her partner was
first asked to demonstrate massage technique to the
research team midwives to ensure that the partner
could perform the procedure properly. If labour was
not yet established, each woman was encouraged
to relax through self-massage on her abdomen and
legs. When labour commenced, the partner stayed
to provide arm and shoulder massage for relaxation
or lateral sacral massage for pain relief, according
to the woman’s preference. There was no time limit
for massage as long as the couple was happy and felt
comfortable to continue the procedure throughout
the labour. The partner could take a break in times
of fatigue, or when the woman fell asleep. The
partners of women in the control group were also
encouraged to accompany the women during labour
and delivery. Women in both groups otherwise
received the same intrapartum care. They received
explanations concerning the effectiveness of various
analgesic methods according to the ranking of
reported efficacy4 7: epidural was ranked highest,
followed by pethidine, then nitrous oxide and other
non-pharmacological analgesia methods (including
transcutaneous nerve stimulation, birthing ball, and
warm pads). Women could choose various methods
or a combination of methods according to their pain tolerance and acceptance, using a step-up approach
or direct implementation of the most effective
methods. The degree of labour pain was assessed
using the visual analogue scale for pain (ranging
from 0 [no pain] to 10 [most painful]) at different
stages of labour: latent phase (cervical dilatation of
1-3 cm), active phase (cervical dilatation of 4-7 cm),
late active phase (cervical dilatation of 8-9 cm), and
second stage (cervical dilatation of 10 cm); it was also
assessed when the women first requested pethidine
or epidural analgesia.
Outcome measures
The primary outcome of this study was the use of
the two most effective pharmacological methods (as
described above): intramuscular pethidine injection
or epidural analgesia. Women were also categorised
according to the type of analgesia that they
eventually received: none of the analgesic methods;
non-pharmacological methods only; nitrous oxide ±
non-pharmacological methods; pethidine ± other
pain relief except epidural; or epidural ± above
methods. The proportions of women that received
each type of analgesia were also compared as one of
the secondary outcomes. Other secondary outcomes
included intrapartum caesarean rate, duration of
labour, the pain score at the point when the women
first requested pethidine or epidural analgesia, the
interval between the onset of labour to the time of
making such a request, and the cervical dilatation at
which such a request was made.
Sample size calculation
A previous study reported a reduction of 60% in the
epidural rate with the use of intrapartum massage
when compared with the control group.2 Therefore,
our study sample size was calculated based on the
assumption that the requirement for pethidine
injection or epidural analgesia could be reduced by
60% (ie, from the current 15% according to Hospital
Authority data to 6%) in the study group. Using an
80% power (beta) threshold and a two-tailed alpha
value of 5%, we calculated that 181 participants were
required in each arm. The method of calculation
was obtained from the website of Department of
Obstetrics and Gynaecology, the Chinese University
of Hong Kong (http://www.obg.cuhk.edu.hk/ResearchSupport/StatTools/index.php). Because we
anticipated that 40% of the recruited participants
would be excluded (eg, because of a shift to a private
hospital for delivery, change to elective caesarean
section, or withdrawal from the study), we planned
to recruit 300 participants for each arm.
Statistical analysis
The Chi squared test and t test were used to assess
differences in baseline characteristics, obstetric outcomes, neonatal outcomes, and the proportions
of women using specific pharmacological pain relief
methods between the massage and control groups.
Linear-by-linear association was used to assess trends
regarding the use of different types of analgesia. The
t test was used to compare between-group differences
in the stage of labour, cervical dilatation, and pain
score among participants who used pethidine/epidural, as well as the mean pain scores in different
phases of labour among participants who did not
use any pain relief modalities. A P value of <0.05 was
considered statistically significant. All analyses used
a per-protocol approach. Intention-to-treat analysis
(including all participants recruited at baseline)
could not be conducted because information
collected during labour (eg, the use of pain relief
modalities) was not available for participants who
delivered in other hospitals, required caesarean
section before pain labour commenced, or withdrew
from the study. Statistical analyses were performed
using SPSS software (Windows version 22.0; IBM
Corp, Armonk [NY], United States).
Results
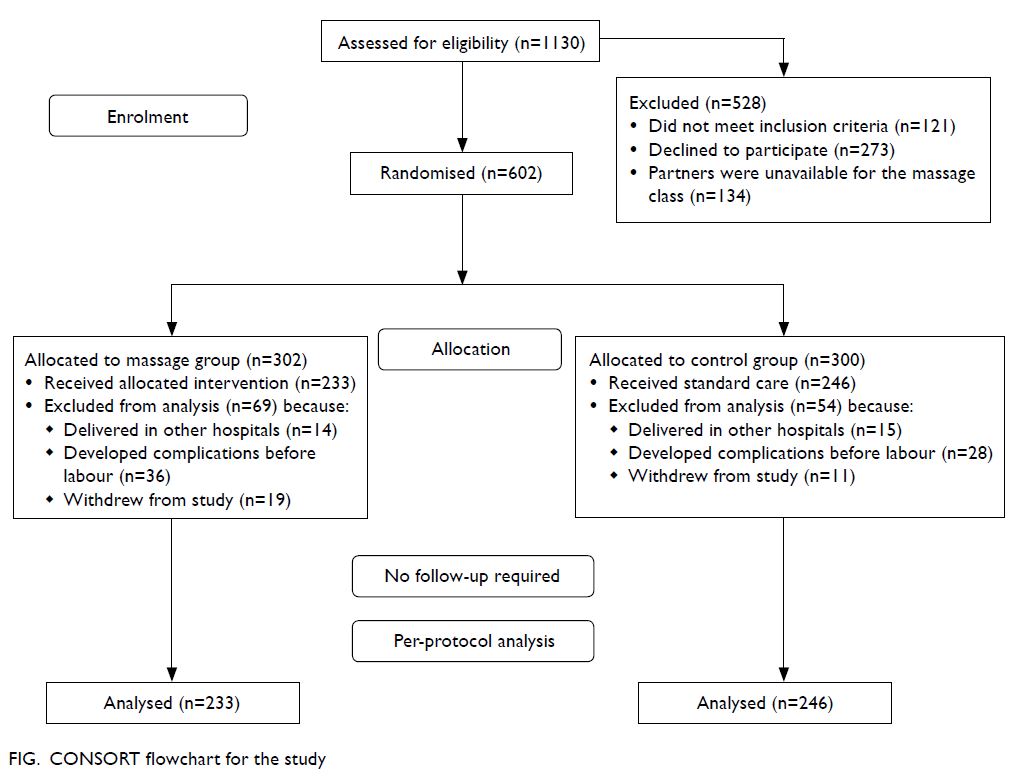
Of the 1130 women eligible for this study, 528 were
excluded for reasons shown in the Figure; thus, 602 women were randomised to the massage group
(n=302) and control group (n=300). Furthermore,
69 (22.8%) and 54 (18.0%) women were subsequently
excluded from the massage and control groups,
respectively, for reasons such as delivery in private
hospitals, planned caesarean section, development
of complications before labour, or withdrawal from
the study. Finally, 479 pregnant women (233 in the
massage group and 246 in the control group) were
included in the per-protocol analysis.
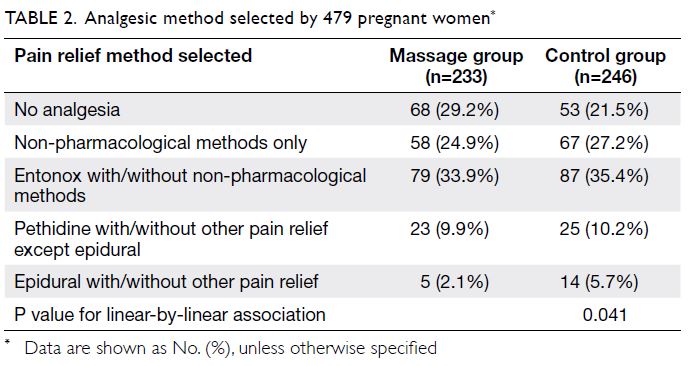
There were no significant differences between
groups in terms of maternal age, height, or
demographic characteristics nor in the proportions
of women who underwent induction of labour,
augmentation of labour, or delivered by caesarean
section (Table 1). The mean duration of labour did
not differ between the massage and control groups.
No significant differences were found in gestational
age at delivery, birthweight, or the proportion of
babies with Apgar score ≥8 at 5 minutes (Table 1).
All women in the massage group practised massage
during labour (n=233). The duration of massage
ranged from 35 minutes to 195 minutes (median,
100 minutes).
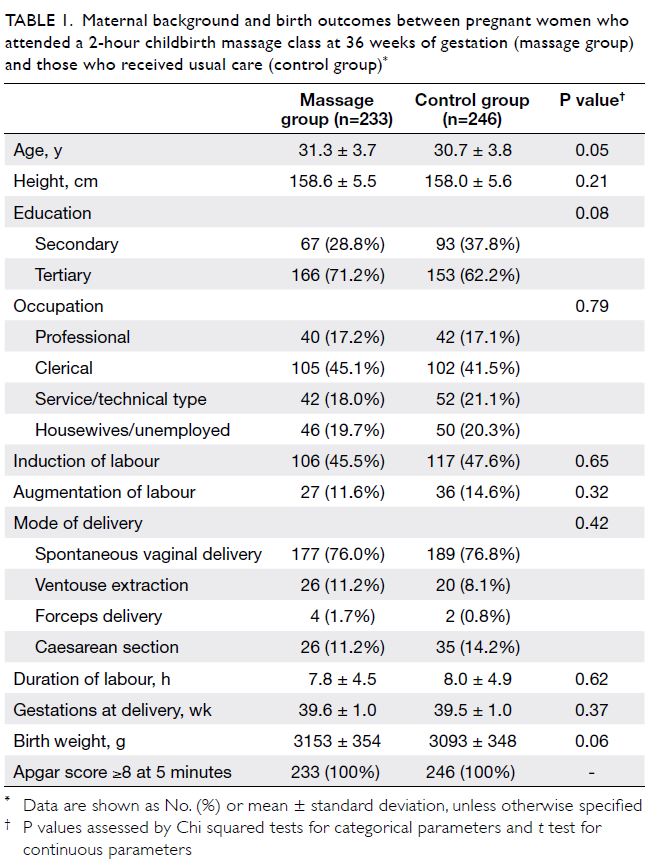
Table 1. Maternal background and birth outcomes between pregnant women who attended a 2-hour childbirth massage class at 36 weeks of gestation (massage group) and those who received usual care (control group)
The proportion of women who used pethidine
or epidural did not significantly differ between
the massage and control groups (12.0% vs 15.9%; P=0.226). However, linear-by-linear association
analysis showed a significant shift in the massage
group, from using stronger analgesics (eg, epidural
analgesia: 2.1% in the massage group vs 5.7% in the
control group) to weaker analgesics. Thus, more
women in the massage group required none of the
analgesics, compared with women in the control
group (29.2% vs 21.5%; P=0.041) [Table 2].
Among women who needed pethidine or
epidural for pain control, there was no difference
between the two groups in terms of the pain score
at the point when they requested these pain relief
modalities, or the interval between the onset of labour
to the time of requesting these modalities (Table 3).
However, the cervical dilatation at which pethidine
or epidural was first requested was significantly
greater in the massage group (3.8 ± 1.7 cm)
than in the control group (2.3 ± 1.0 cm; P<0.001)
[Table 3].
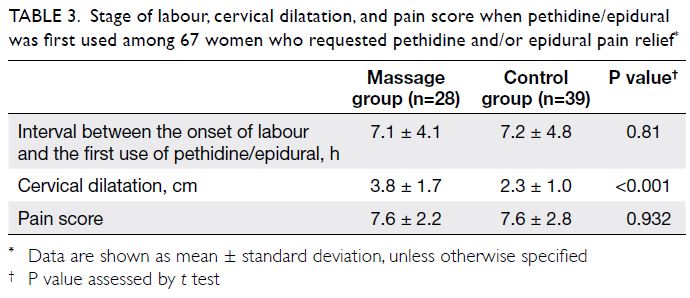
Table 3. Stage of labour, cervical dilatation, and pain score when pethidine/epidural was first used among 67 women who requested pethidine and/or epidural pain relief
Among women who needed none of the pain
relief modalities, the pain scores progressively
increased with cervical dilatation, although there
were no differences between the two groups
(Table 4).
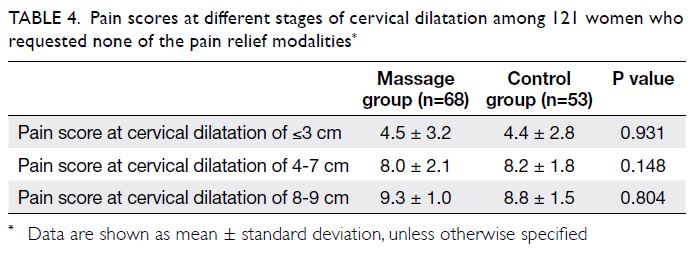
Table 4. Pain scores at different stages of cervical dilatation among 121 women who requested none of the pain relief modalities
Discussion
Although our study did not show a statistically
significant reduction in the number of women who
used either pethidine or epidural analgesia with the
practice of massage (12.0% vs 15.9%), linear-by-linear
analysis revealed that there was a statistically
significant overall shift in the pattern of analgesics
use in the massage group: a smaller proportion of
women requested epidural analgesia (2.1% vs 5.7%)
and a larger proportion of women requested none of
the pain relief methods (29.2% vs 21.5%). Our results
suggest that the pain perceptions of labouring
women were improved by the training and practice
of massage, controlled breathing, and visualisation.
Thus, some women who initially requested the
stronger methods (eg, epidural analgesia) might
have achieved satisfactory pain control with weaker
analgesic methods (eg, pethidine or nitrous oxide).
Similarly, women who initially requested pethidine
or nitrous oxide might have shifted to non-pharmacological
methods only; this led to a greater
proportion of women in the massage group who
requested no analgesia.
Interpretation
Although pain scores are commonly used to compare
analgesic effectiveness, such comparisons are often
difficult on the basis of a single pain score during
labour. This is because the labour process is generally
long and its characteristics are variable; labouring
women might use more than one method of pain
relief at different stages of labour. Nonetheless, if the pain is intolerable, labouring women require
a stronger analgesic method.28 Hence, we used a
pattern of analgesic utility (rather than a single
pain score) as an indicator for the effectiveness
of the massage programme; our linear-by-linear
association findings indicated that the massage
programme may reduce pain perception among labouring women. Furthermore, the mean cervical
dilatation at the time of pethidine or epidural
analgesia request was higher in the massage group
than in the control group (3.8 ± 1.7 cm vs 2.3 ± 1.0 cm).
Notably, among women who requested pethidine
or epidural analgesia, the pain score at the point of
first pethidine or epidural analgesia request was very
similar between the massage and control groups
(7.6 ± 2.2 vs 7.6 ± 2.8). Although the midwives were
not blinded to the allocation in this study, women in
both groups received the same intrapartum care and
could choose pain relief methods according to their
pain tolerance and acceptance. These results further
support the notion that the practice of massage
might have modulated the pain perception among
labouring women, such that they only requested
stronger pharmacological pain relief during later
phases of labour; additional studies are required to
confirm the underlying biological mechanism.
Janssen et al17 also reported a delay in epidural
insertion by 1 cm of cervical dilatation (5.9 cm in the
massage group vs 4.9 cm in the control group) in their
randomised controlled trial. However, they failed to
show a significant reduction in the rate of epidural
analgesia use (81.1% in the massage group vs 65.0%
in the control group). Importantly, their participants
only learned and practised massage at the time of
labour, while our participants began learning the
massage programme during the antenatal period.
In another randomised controlled trial,
Levett et al21 showed that the incidence of epidural
analgesia was significantly reduced (from 68.2% to 23.9%) in a cohort of 176 Australian patients.
However, their control group had a baseline epidural
analgesia rate of 68.2%, which was much higher than
the rate in our control group (ie, 5.7%, which is similar
to the 6.6% reported previously in Hong Kong29)
Possible reasons for the large difference in epidural
rates between Australia and Hong Kong include
variations in midwifery practices, pain tolerance
among labouring women, and limited resources in
Hong Kong public hospitals. Other obstetric practice
differences include an overall (massage and control
groups combined) higher normal vaginal delivery
rate in our cohort than in the cohort reported by
Levett et al21 (76.4% vs 57.9%); our overall cohort
also exhibited a lower instrumental delivery rate
(10.9% vs 17.0%) and a lower caesarean section rate
(12.7% vs 25.1%). Regardless of our low baseline
epidural rate, we found a 60% reduction in epidural
use in the massage group (2.1%), compared with
the control group (5.7%). Finally, Levett et al21 only
reported the incidence of simultaneous use of
pethidine and nitrous oxide, whereas we stratified
analgesic methods according to the strength of
pain relief; this allowed us to detect an overall shift
towards weaker analgesics among women in the
massage group.
Importantly, neither study (this study or the
study by Levett et al21) demonstrated any reduction
in the overall duration of labour in nulliparous
women, although the cohort reported by Levett et al21
exhibited a marked reduction in the rate of epidural
use. In contrast, Bolbol-Haghighi et al22 showed that
massage practice was associated with significantly
shorter durations in both the first stage (9.0 hours
vs 11.5 hours) and the second stage of labour
(49 minutes vs 64 minutes) among a cohort of Iranian
women. However, their study included multiparous
women with an overall vaginal delivery rate over
95%; they did not describe the availability of epidural
analgesia for their participants. In summary, it
remains unclear whether the practice of massage
has consistent effects on labour progression; the
underlying mechanisms of such effects are unknown.
Strengths and limitations
This study had several strengths. First, it involved
a large number of nulliparous labouring women.
To our knowledge, this is the largest number of
such women among similar published studies; it
allowed us to identify any changes in the utilisation
of different levels of analgesic methods, without
any confounding effects related to multiparity.20 22
Second, this study involved a team of accredited
and dedicated midwife trainers, which enabled us
to ensure that a consistent high-quality massage
technique was applied to women in the study. Third,
training at 36 weeks of gestation allowed each
couple (ie, a participating woman and her partner) to have sufficient time to practise massage at home
and refine their technique before the woman began
labour. Fourth, on admission prior to delivery,
an accredited midwife trainer was available to
verify each couple’s massage technique and ensure
quality. Finally, there was no limit to the duration
of intrapartum massage; women could receive their
preferred amount of massage to achieve optimal
results.
There were some notable limitations in this
study. First, because of the pain relief methods
used, we were unable to incorporate blinding in
the trial design. However, the midwives providing
intrapartum care were not involved in data
collection. Second, approximately one-fifth of the
participants in each group had changes to their
childbirth plan, including shift to a private hospital
or to planned caesarean delivery; thus, they were
excluded from the final analysis. Third, we could
only assess the intrapartum massage provided by the
participating women’s partners; we could not assess
the breathing and visualisation practice at home,
which are also essential components of the overall
massage programme. Finally, because continuous
foetal heart monitoring was the standard method of
intrapartum foetal surveillance in Hong Kong during
the study period, women were unable to move freely
during labour; this restriction might have limited
the ability to perform certain massage techniques.
Nevertheless, the shifts towards less epidural
analgesia use and higher rates of analgesic-free
labour, in the absence of adverse labour outcomes,
support the efficacy of our massage programme.
Conclusion
This study demonstrated an overall shift towards
using weaker pain relief modalities among women
participating in an intrapartum massage programme.
The findings imply that massage, in combination
with controlled breathing and visualisation, may
modulate pain perception among labouring women,
leading to higher rates of analgesic-free labour.
Author contributions
Concept or design: CY Lai.
Acquisition of data: MKW Wong, WH Tong, SY Chu, KY Lau, AML Tam.
Analysis or interpretation of data: CY Lai, LL Hui.
Drafting of the manuscript: CY Lai, TTH Lao, TY Leung.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: MKW Wong, WH Tong, SY Chu, KY Lau, AML Tam.
Analysis or interpretation of data: CY Lai, LL Hui.
Drafting of the manuscript: CY Lai, TTH Lao, TY Leung.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
The authors thank Ms Linda Kimber, Midwife/Director, and
Ms Mary McNabb, Scientific Advisor and Academic Midwife,
both of Childbirth Essentials, Banbury, United Kingdom, for
training the midwives involved in the present study and for
advising the authors on the study design.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The study was approved by The Joint Chinese University of
Hong Kong–New Territories East Cluster Clinical Research
Ethics Committee (CREC Ref: 2016.332). The study has been registered
at the Centre for Clinical Research and Biostatistics, The
Chinese University of Hong Kong, (Unique Trial Number:
CUHK_CCRB00525; https://www2.ccrb.cuhk.edu.hk/registry/public/393). All participants were informed about the nature
of the study and provided written consent to participate
before randomisation into study groups.
References
1. Kabeyama K, Miyoshi M. Longitudinal study of the intensity of memorized labour pain. Int J Nurs Pract
2001;7:46-53. Crossref
2. Rijnders M, Baston H, Schönbeck Y, et al. Perinatal factors
related to negative or positive recall of birth experience
in women 3 years postpartum in the Netherlands. Birth
2008;35:107-16. Crossref
3. Rachmawati IN. Maternal reflection on labour pain management and influencing factors. Br J Midwifery
2012;20:263-70. Crossref
4. Yerby M. Managing pain in labour. Part 3: pharmacological
methods of pain relief. Mod Midwife 1996;6:22-5.
5. Cawthra AM. The use of pethidine in labour. Midwives Chron 1986;99:178-81.
6. Rajan L. The impact of obstetric procedure and analgesia/anaesthesia during labour and delivery on breastfeeding.
Midwifery 1994;10:87-103. Crossref
7. Jones L, Othman M, Dowswell T, et al. Pain management for women in labour: an overview of systematic reviews.
Cochrane Database Syst Rev 2012;(3):CD009234. Crossref
8. Anim-Somuah M, Smyth RM, Cyna AM, Cuthbert A.
Epidural versus non-epidural or no analgesia for pain
management in labour. Cochrane Database Syst Rev 2018;(5):CD000331. Crossref
9. Klomp T, van Poppel M, Jones L, Lazet J, Di Nisio M, Lagro-Janssen AL. Inhaled analgesia for pain management
in labour. Cochrane Database Syst Rev 2012;(9):CD009351. Crossref
10. Thomson G, Feeley C, Moran VH, Downe S, Oladapo OT.
2019 Women’s experiences of pharmacological and non-pharmacological
pain relief methods for labour and
childbirth: a qualitative systematic review. Reprod Health
2019;16:71. Crossref
11. Chaillet N, Belaid L, Crochetière C, et al. Nonpharmacologic
approaches for pain management during labor compared
with usual care: a meta-analysis. Birth 2014;41:122-37. Crossref
12. Field T, Hemandez-Reif M, Taylor S, Quintino O, Burman I. Labor pain is reduced by massage therapy. J Psychosom
Obstet Gynecol 1997;18:286-91. Crossref
13. McCaffery M, Beebe A. Pain: clinical manual for nursing practice. J Pain Symptom Manage 1990;5:338-9. Crossref
14. Chang MY, Wang SY, Chen CH. Effects of massage on pain
and anxiety during labour: a randomized controlled trial in
Taiwan. J Adv Nurs 2002;38:68-73. Crossref
15. Karami NK, Safarzadeh A, Fathizadeh N. Effect of massage
therapy on severity of pain and outcome of labour in
primipara. Iran J Nurs Midwifery Res 2007;12:6-9.
16. Kimber L, McNabb M, Mc Court C, Haines A,
Brocklehurst P. Massage or music for pain relief in labour:
a pilot randomised placebo controlled trial. Eur J Pain
2008;12:961-9. Crossref
17. Janssen P, Shroff F, Jaspar P. Massage therapy and labor
outcomes: a randomized controlled trial. Int J Ther
Massage Bodywork 2012;5:15-20. Crossref
18. Mortazavi SH, Khaki S, Moradi R, Heidari K, Vasegh
Rahimparvar SF. Effects of massage therapy and presence
of attendant on pain, anxiety and satisfaction during
labour. Arch Gynecol Obstet 2012;286:19-23. Crossref
19. Silva Gallo RB, Santana LS, Jorge Ferreira CH, et al. Massage
reduced severity of pain during labour: a randomised trial.
J Physiother 2013;59:109-16. Crossref
20. Mc Nabb MT, Kimber L, Haines A, McCourt C. Does
regular massage from late pregnancy to birth decrease
maternal pain perception during labour and birth? A
feasibility study to investigate a programme of massage,
controlled breathing and visualization, from 36 weeks
of pregnancy until birth. Complement Ther Clin Pract
2006;12:222-31. Crossref
21. Levett KM, Smith CA, Bensoussan A, Dahlen HG. Complementary therapies for labour and birth study:
a randomised controlled trial of antenatal integrative medicine for pain management in labour. BMJ Open
2016;6:e010691. Crossref
22. Bolbol-Haghighi N, Masoumi SZ, Kazemi F. Effect of massage therapy on duration of labour: a randomized
controlled trial. J Clin Diagn Res 2016;10:12-5. Crossref
23. Taghinejad H, Delphisheh A, Suhrabi Z. Comparison between massage and music therapies to relieve the severity
of labour pain. Womens Health (Lond) 2010;6:377-81. Crossref
24. Smith CA, Levett KM, Collins CT, Dahlen HG, Ee CC,
Suganuma M. Massage, reflexology and other manual
methods for pain management in labour. Cochrane
Database Syst Rev 2018;(3):CD009290. Crossref
25. Hui AS, Lao TT, Leung TY, Schaaf JM, Sahota DS. Trends
in preterm birth in singleton deliveries in a Hong Kong
population. Int J Gynaecol Obstet 2014;127:248-53. Crossref
26. The Royal College of Midwives. Childbirth essentials
towards natural childbirth and beyond. Available from:
https://www.rcm.org.uk/promoting/learning-careers/
accredited-learning/childbirth-essentials-towards-natural-childbirth-and-beyond/. Accessed 19 Feb 2020.
27. Fuchs AR, Behrens O, Liu HC. Correlation of nocturnal
increase in plasma oxytocin with a decrease in plasma
estradiol/progesterone ratio in late pregnancy. Am J Obstet
Gynecol 1992;167:1559-63. Crossref
28. Tsui MH, Ngan Kee WD, Ng FF, Lau TK. A double blinded
randomised placebo-controlled study of intramuscular
pethidine for pain relief in the first stage of labour. BJOG
2004;111:648-55. Crossref
29. Hong Kong College of Obstetricians and Gynaecologists.
Report of the territory-wide audit in obstetrics &
gynaecology. 2014. Available from: https://www.hkcog.org.hk/hkcog/pages_4_307.html. Accessed 19 Feb 2020.