Hong Kong Med J 2021 Oct;27(5):373.e1–2
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Gastric emphysema
G Liang, MMed; LC Zeng, MMed; MG Xie, BMed; MX Zhang, MMed (TCM); ZH Hou, MMed (TCM)
Department of Radiology, Hospital of Chengdu University of Traditional Chinese Medicine, Chengdu, Sichuan, China
Corresponding author: Prof MG Xie (xmg6806@163.com)
Case
A 47-year-old woman was admitted to the intensive
care unit following craniectomy for intracranial
haematoma. She reported tenderness in the epigastric
region with no evidence of peritonitis. Enhanced
computed tomography (CT) of the abdomen revealed
a distended stomach and diffuse circumferential air
in the stomach wall, with prominent enhancement of
the stomach wall mucosa. Pneumoperitoneum was detected on identification of extraluminal stomach
air along the greater curvature (Fig 1). Laboratory
results showed no abnormality. The patient had
no obvious predisposing factors or infection and
inflammatory markers in blood cultures were
normal. Based on the clinical presentation and
relevant laboratory examinations, assessment
of predisposing factors and CT findings, gastric
emphysema (GE) was diagnosed and the patient
was managed conservatively. She underwent gastric
decompression with nasogastric tube placement
and fluid resuscitation, and was prescribed a proton
pump inhibitor and broad-spectrum antibiotics.
Non-enhanced CT scan 11 days later revealed
complete resolution of gas within the submucosal
layer (Fig 2).
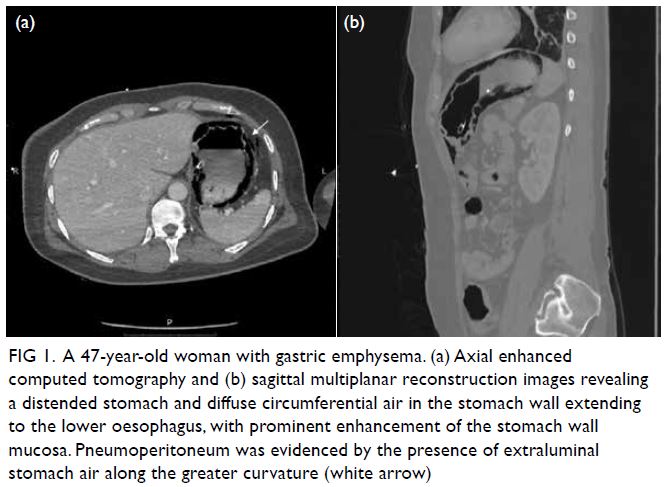
Figure 1. A 47-year-old woman with gastric emphysema. (a) Axial enhanced computed tomography and (b) sagittal multiplanar reconstruction images revealing a distended stomach and diffuse circumferential air in the stomach wall extending to the lower oesophagus, with prominent enhancement of the stomach wall mucosa. Pneumoperitoneum was evidenced by the presence of extraluminal stomach air along the greater curvature (white arrow)
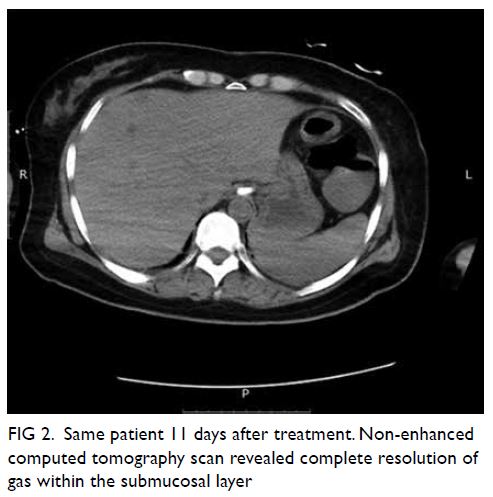
Figure 2. Same patient 11 days after treatment. Non-enhanced computed tomography scan revealed complete resolution of gas within the submucosal layer
Discussion
Gastric pneumatosis is a rare finding identified by
accumulation of gas within the stomach wall. Both
GE and emphysematous gastritis (EG) are important
differential diagnoses of intramural gastric air. They
differ in their aetiology, clinical course, radiographic
findings, management, and prognosis. However, it is
important to differentiate the much more benign GE
from the highly lethal EG.
Gastric emphysema is caused by a disruption
in gastric mucosal integrity without underlying
infection. Most patients with GE have no or mild
symptoms, and the prognosis is excellent.1 Gastric
emphysema is a relatively benign condition and
usually self-limiting. The causes of the mucosal
defect in GE include increased intragastric
pressure, instrumentation such as gastroscopy,
severe vomiting, and dissection of air from the
mediastinum and ischaemia. The management of
GE is usually non-surgical and includes bowel rest
with nasogastric tube placement, fluid resuscitation
and nutritional support.1 We think our case of GE
was related to stress-related mucosal erosions of
the stomach mucosa, and possibly increased gastric
distension.
In contrast, EG, resulting from gas-forming
organisms and associated with systematic toxicity,
is a devastating infectious process with a mortality
rate of 60%.2 3 Patients with EG usually display severe
clinical signs including severe abdominal pain,
severe abdominal tenderness, haematemesis, and
occult gastric bleeding. The patient may need to be
transferred to the intensive care unit and treated
with broad-spectrum antibiotics if there is evidence of bacterial infection. Patients should undergo
oesophagogastroduodenoscopy and enhancement CT
as early as possible when EG is suspected. Surgical
intervention is more commonly indicated for EG and
is directed at removal of the septic organ, whereas
the primary indication for surgical intervention in
GE is uncertainty of diagnosis.3 4
In summary, despite similar radiographic
findings, GE is typically secondary to mechanical
injury of the stomach mucosa, whereas EG is an acute
infection of the stomach wall. The differentiation of
these two entities depends on the patient’s clinical
presentation, assessment of predisposing factors,
and CT findings.
Author contributions
Concept or design: All authors.
Acquisition of data: G Liang, LC Zeng.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: G Liang.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: G Liang, LC Zeng.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: G Liang.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
We would like to thank two anonymous reviewers and the
journal editor, who have provided excellent comments and
significantly contributed to the improvement of the article.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This study was approved by the Hospital of Chengdu University of Traditional Chinese Medicine Research Ethics
Committee. Informed consent was obtained from the patient.
References
1. Matsushima K, Won EJ, Tangel MR, Enomoto LM,
Avaella DM, Soybel DI. Emphysematous gastritis and
gastric emphysema: similar radiographic findings, distinct
clinical entities. World J Surg 2015;39:1008-17. Crossref
2. Misro A, Sheth H. Diagnostic dilemma of gastric
intramural air. Ann R Coll Surg Engl 2014;96:e11-3. Crossref
3. Guillén-Morales C, Jiménez-Miramón FJ, Carrascosa-Mirón T, Jover-Navalón JM. Emphysematous gastritis
associated with portal venous gas: medical management
to an infrequent acute abdominal pain. Rev Esp Enferm
Dig 2015;107:455-6. Crossref
4. Inayat F, Zafar F, Zaman MA, Hussain Q. Gastric emphysema secondary to severe vomiting: a comparative
review of 14 cases. BMJ Case Rep 2018;2018:
bcr2018226594. Crossref

