Hong Kong Med J 2021 Apr;27(2):154–6 | Epub 9 Apr 2021
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
COMMENTARY
Optimising vitamin D levels in patients with COVID-19
Jasndeep Kaler, BA1; Azhar Hussain, BA, MBA1,2; Dua Azim, MB, BS3; Syed Ali, BS4; Sundus Nasim, MB, BS3
1 Xavier University School of Medicine, Oranjestad, Aruba
2 Doctoral Candidate of HealthCare Administration, Franklin University, Ohio, United States
3 Dow Medical College, Dow University of Health Sciences, Karachi, Pakistan
4 Stony Brook University, New York, United States
Corresponding author: Mr Azhar Hussain (azharhu786@gmail.com)
As the spread of severe acute respiratory syndrome
coronavirus 2 (SARS-CoV-2) continues, the focus
on establishing a comprehensive treatment strategy
is greater than ever. Coronavirus disease 2019
(COVID-19) places an immense burden on public
health and limited hospital capacity; thus, it comes
as no surprise that an effective therapeutic option
has become a dire necessity. Although many drugs
are currently undergoing clinical trials to test
their efficacy and safety for treating patients with
COVID-19, no specific medicine has been confirmed
as truly beneficial to date.
The pathogenesis of SARS-CoV-2 is considered
a two-phase viral response: the first immune
defence-mediated protective phase and the second
inflammation-driven destructive phase. Clinicians
need immune boosters to manage phase one of
COVID-19, and immune suppressors to manage
phase two.
Recently, tocilizumab, an immunosuppressive
drug, has gained considerable attention as a
potential treatment option for patients with
COVID-19. Tocilizumab, a synthetic monoclonal
antibody, competitively inhibits the binding of
interleukin (IL)-6 to its receptor, making it incapable
of inducing immune damage, and relieving the
inflammatory reactions.1 Therefore, tocilizumab
provides hope for treating critically ill patients with
COVID-19; however, it can be used to manage only
phase two, the inflammatory phase of COVID-19.
Moreover, tocilizumab is expensive and requires
intravenous administration, and it is associated with
complications including gastrointestinal perforation
and elevated pancreatic biomarkers.1 Thus, there
is a growing need for a cheaper and more readily
available alternative treatment that can be used in
both phases of COVID-19.
Several studies have demonstrated a potential
link between vitamin D and various respiratory
illnesses.2 The role of vitamin D against viral infections
is twofold. First, vitamin D induces the production
of antiviral peptides such as cathelicidin in the
respiratory epithelium, which strengthens mucosal defenses.3 Second, vitamin D reduces cytokine
production by enhancing the innate immune system
and suppressing the overactivation of the adaptive
immune system secondary to viral load.4 Recent
evidence also suggests an association of increased
levels of IL-6 with vitamin D deficiency in HIV
infection.5 Vitamin D may mitigate the production of
pro-inflammatory and anti-inflammatory cytokines,
such as tumour necrosis factor α and IL-6, generated
by the innate immune system in response to
SARS-CoV-2 infection.
There is little evidence on the role of vitamin D
deficiency in COVID-19 severity and mortality. The
SARS-CoV-2 outbreak emerged during winter in the
Northern Hemisphere; influenza virus also happens
to peak in winter.6 Because supplementation with
vitamin D lowers the risk of influenza A,7 insufficient
levels of vitamin D due to reduced sunlight exposure
in Northern regions may have contributed to the
increased incidence of COVID-19.
Another indirect connection between poorer
outcomes of COVID-19 and low vitamin D levels
arises from the observation that some ethnicities are
differentially affected by ongoing pandemic. Darker
skin tone raises the risk of vitamin D deficiency, and
estimates from the Office for National Statistics,
United Kingdom, indicate a fourfold risk of
COVID-19-related deaths in dark-skinned
individuals from England and Wales relative to
lighter-skinned individuals.8
We extracted data on the number of
COVID-19 cases and deaths up to 6 August 2020
from the worldwide COVID-19 pandemic database9
and data on about the prevalence of vitamin D
deficiency from previous studies (Table).10 11 12 13 14 We
found that people residing in regions that are
severely affected by COVID-19 also often had
vitamin D deficiency, further reinforcing the
potential correlation of vitamin D with seriousness
of the disease.
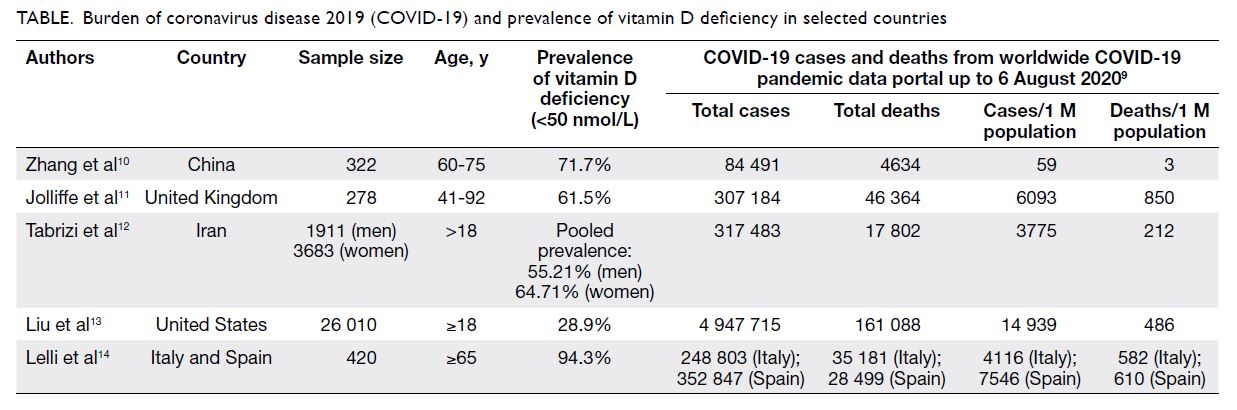
Table. Burden of coronavirus disease 2019 (COVID-19) and prevalence of vitamin D deficiency in selected countries
Although low vitamin D levels are implicated
in severity and mortality of COVID-19, there is
no evidence to date supporting supplementation with vitamin D as a therapy with dose-response
curve. However, several randomised open-label
and blinded clinical trials are currently in progress
of investigating vitamin D as a treatment option for
COVID-19, rather than a preventive measure.15 16 17
Considering the expensiveness, limited
availability, and adverse effects of tocilizumab, we
believe that vitamin D is safe and offers a viable
therapeutic option. The twofold mechanism of
vitamin D in countering SARS-CoV-2 infection
reinforces our confidence in its preventive and
therapeutic adequacy. Further research is required
to elucidate the exact mechanism of vitamin D in
SARS-CoV-2 pathogenesis. We recommend that
patients with COVID-19 have blood vitamin D
levels tested on hospitalisation; these data would
be invaluable in investigating any links between
COVID-19 mortality and vitamin D. In the
meantime, we recommend following the vitamin D
supplementation guidelines set out by public health
authorities.
Author contributions
J Kaler and A Hussain contributed to the study concept and
critically revised the manuscript for important intellectual
content. All authors contributed to acquisition and analysis
of the data and drafted the manuscript. All authors had full
access to the data, contributed to the study, approved the final
version for publication, and take responsibility for its accuracy
and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This commentary received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
1. Nasim S, Hashmi SH, Azim D, Kumar S, Nasim J. Tocilizumab for COVID-19: a real ‘miracle drug’? Infect
Dis (Lond) 2020;52:681-2. Crossref
2. Berry DJ, Hesketh K, Power C, Hyppönen E. Vitamin D
status has a linear association with seasonal infections and
lung function in British adults. Br J Nutr 2011;106:1433-40. Crossref
3. Gombart AF, Borregaard N, Koeffler HP. Human
cathelicidin antimicrobial peptide (CAMP) gene is a
direct target of the vitamin D receptor and is strongly up-regulated
in myeloid cells by 1,25-dihydroxyvitamin D3.
FASEB J 2005;19:1067-77. Crossref
4. Greiller C, Martineau A. Modulation of the immune response to respiratory viruses by vitamin D. Nutrients
2015;7:4240-70. Crossref
5. Manion M, Hullsiek KH, Wilson EM, et al. Vitamin D
deficiency is associated with IL-6 levels and monocyte
activation in HIV-infected persons. PLoS One
2017;12:e0175517. Crossref
6. Hope-Simpson RE. The role of season in the epidemiology of influenza. J Hyg (Lond) 1981;86:35-47. Crossref
7. Urashima M, Segawa T, Okazaki M, Kurihara M, Wada Y,
Ida H. Randomized trial of vitamin D supplementation to
prevent seasonal influenza A in schoolchildren. Am J Clin
Nutr 2010;91:1255-60. Crossref
8. Office for National Statistics, UK Government. Coronavirus
(COVID-19) related deaths by ethnic group, England and
Wales: 2 March 2020 to 10 April 2020. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/coronavirusrelateddeathsbyethnicgroupenglandandwales/2march2020to10april2020. Accessed 5 Jul 2020.
9. Worldometer. COVID-19 coronavirus pandemic. Available from: https://www.worldometers.info/coronavirus/.Accessed 6 Aug 2020.
10. Zhang W, Zheng X, Wang Y, Xiao H. Vitamin D deficiency as a potential marker of benign prostatic hyperplasia.
Urology 2016;97:212-8. Crossref
11. Jolliffe DA, James WY, Hooper RL, et al. Prevalence,
determinants and clinical correlates of vitamin D deficiency
in patients with Chronic Obstructive Pulmonary Disease
in London, UK. J Steroid Biochem Mol Biol 2018;175:138-45.Crossref
12. Tabrizi R, Moosazadeh M, Akbari M, et al. High prevalence
of vitamin D deficiency among Iranian population: a
systematic review and meta-analysis. Iran J Med Sci 2018;43:125-39.
13. Liu X, Baylin A, Levy PD. Vitamin D deficiency and
insufficiency among US adults: Prevalence, predictors and
clinical implications. Br J Nutr 2018;119:928-36. Crossref
14. Lelli D, Pérez Bazan LM, Calle Egusquiza A, et al. 25(OH)
vitamin D and functional outcomes in older adults admitted
to rehabilitation units: the safari study. Osteoporos Int
2019;30:887-95. Crossref
15. ClinicalTrials.gov, US National Library of Medicine.
Improving vitamin D status in the management of
COVID-19. Available from: https://clinicaltrials.gov/ct2/show/NCT04385940. Accessed 6 Aug 2020.
16. ClinicalTrials.gov, US National Library of Medicine.
Prevention and treatment with calcifediol of COVID-19
coronavirus-induced acute respiratory syndrome (SARS).
Available from: https://clinicaltrials.gov/ct2/show/NCT04366908. Accessed 6 Aug 2020.
17. ClinicalTrials.gov, US National Library of
Medicine. Preventive and therapeutic effects of oral
25-hydroxyvitamin D3 on coronavirus (COVID-19) in
adults. Available from: https://clinicaltrials.gov/ct2/show/NCT04386850. Accessed 6 Aug 2020.

