Hong Kong Med J 2021 Feb;27(1):61–3 | Epub 2 Feb 2021
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
COMMENTARY
Successfully conducting an objective structured
clinical examination with real patients during the
COVID-19 pandemic
CH Lee#, MB, BS; Pauline Y Ng#, MB, BS; Shirley YY Pang#, MD; David CL Lam, MD; CS Lau, MD
Department of Medicine, The University of Hong Kong, Hong Kong
# These authors contributed equally to this commentary.
Corresponding author: Prof CS Lau (cslau@hku.hk)
Introduction
For decades, the objective structured clinical
examination (OSCE) has been regarded as a valid
and reliable method of assessing clinical competency
in medical education. The choice of patient
representation in an OSCE depends on context
and availability.1 The coronavirus disease 2019
(COVID-19) pandemic presents an unprecedented
challenge to both medical education and examinations
worldwide, especially high-stakes qualification
examinations such as the final-year medical student
OSCE. Whereas some medical schools elected to
cancel all clinical examinations and grant provisional
registration to graduates, others have resorted to
the use of manikins, video recordings, or simulated
patients for assessment of clinical skills.2 Hong Kong
was one of the earliest regions in the world to be
affected by COVID-19.3 Owing to uncertainty about
the scale of the local outbreak, the Department of
Medicine at The University of Hong Kong decided to
uphold the format of its final-year OSCE by involving
assessment of real patients in all clinical stations. We
hereby report the organisation details of our OSCE
conducted during the COVID-19 pandemic, with a
focus on adaptations that were necessary to address
concerns about infection control, whilst maintaining
the overall validity of the examination.
Objective structured clinical
examination design and structure
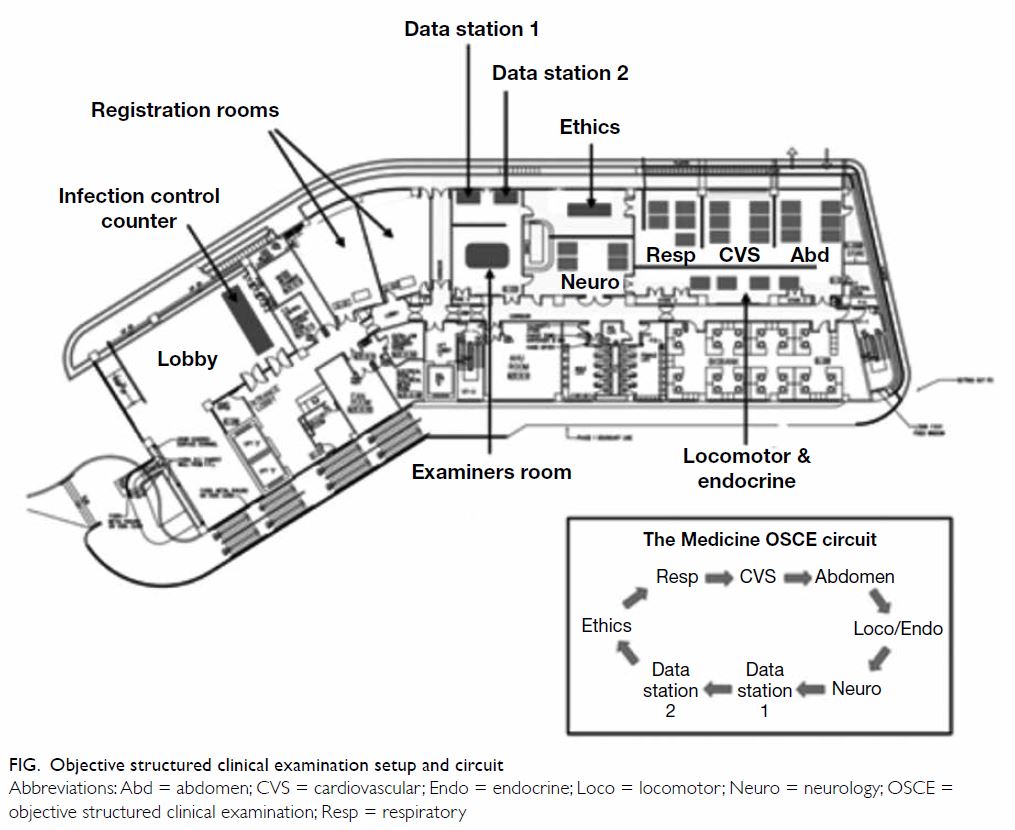
Our OSCE for the graduating class of 2020 was
conducted from 4 to 8 May 2020. A total of 204
candidates, divided into 26 cohorts, were examined.
As in previous years, each candidate was examined
in a circuit of eight stations within 80 minutes,
consisting of five clinical stations with real patients,
two data interpretation stations, and one on ethics
and communication with a trained actor. Candidates
were examined at each clinical station by a pair of
physician examiners, who separately graded their
performance based on a standardised marking
scheme, with emphasis on the approach to patients,
core examination skills, and ability to detect and
interpret physical signs.
In the past, our medical OSCE had always
been conducted in the ward areas of Queen Mary
Hospital, Hong Kong. However, following our first
confirmed COVID-19 patient on 22 January 2020
and activation of the Emergency Response Level
in public hospitals 3 days later mandating that
all teaching activities conducted within hospital
compounds be suspended,4 our OSCE had to be
relocated to a non-clinical area on campus. Seminar
rooms had to be temporarily converted to patient
cubicles using portable ward screens, and a total of
five seminar rooms were employed to construct the
OSCE circuit (Fig).
Altogether, 52 volunteer patients from the
community were recruited, with an average of
24 patients participating on each day of the
examination due to multiple attendances. Since
most clinical staff were deployed to combat
COVID-19, a crew of 70 research assistants,
laboratory technicians, post-doctoral fellows
and administrative staff, who mostly had no
prior experience with the OSCE, was enlisted as
administrators and helpers.
Infection control measures
Our OSCE was also conducted when the Prohibition
on Group Gathering Regulation, which limited
group gatherings of more than four people in
public places, was in force. Our Faculty successfully
acquired exemption from this Regulation for our
OSCE. Since close physical contact was inevitable
during clinical examination and in order to safeguard
all participants, several faculty-wide stringent
precautionary infection control measures were
implemented.
Firstly, all participants, including candidates,
examiners, patients and helpers, submitted a deep
throat saliva specimen for severe acute respiratory
syndrome coronavirus 2 reverse-transcription
polymerase chain reaction test at least 2 days prior to
their OSCE participation. Secondly, all participants
were required to submit a health declaration form
1 day prior to each day of examination. Those who
declared any suggestive symptom in the past 7 days,5 history of travel or contact with confirmed or
suspected COVID-19 patients in the past 14 days,
were flagged for further considerations before being
allowed to participate in the examination on the
following day. Thirdly, participants who persistently
had a body temperature of ≥37.5°C measured on
arrival at the examination venue were subjected to
clinical assessment by the on-duty infection control
supervisor to determine if they would be permitted
to participate. Protocols were in place for clinical
assessment of candidates for these purposes.
At all times during the OSCE, participants
were required to wear surgical masks, and examiners
and candidates had been instructed not to unmask
a patient at any time. Demonstration of cough
manoeuvre was also not mandatory. To minimise
close contact, fundoscopic examination was
replaced by interpretation of retinal photos in the
data stations. Participants were required to perform
strict hand hygiene using alcohol-based hand rub
and disinfect their clinical instruments before and
after examining each patient. Social distancing
was observed in all waiting areas, with a spacing of 2-metre radius between seats. All bedsheets,
pillows, and pyjamas of patients were changed daily,
and the examination hall was disinfected twice daily.
Lunch and drinks were all individually packaged
and consumed within each individual’s assigned
station.
At the conclusion of our OSCE, only one
candidate did not attend the examination because
of persistent fatigue and will be allowed to sit in the
Supplementary Examination. No candidates were
denied entry on the day of examination. A total
of 53 clinical teachers assessed the candidates at
the clinical examination stations. All volunteering
patients had negative COVID-19 tests and there
were at least three patients in each clinical station
daily. No major equipment failure occurred during
OSCE, except for a slight delay in the electronic
scoring system on the first day of the examination,
which were immediately resolved by our on-site
computer technicians. The candidates’ pass and fail
rates were similar to previous OSCEs. Importantly,
no participants have contracted COVID-19 through
participation in the examination.
Difficulties and limitations
The implementation of the above measures was not
without difficulties, and there remain limitations
worth highlighting. Although an out-of-hospital
venue was reassuring to patients who wished to avoid
hospital attendance during the pandemic, this limited
the diversity of patients, especially in terms of their
disease severity, represented in our OSCE. Some
patients who had participated in OSCEs in past years
declined to help this time for fear of contracting the
virus despite the out-of-hospital venue. Nonetheless,
since the selection of patients was based on a list
of core and optional medical competencies that
students are expected to acquire during various
clerkship teachings in our Department, the overall
disease spectrum represented was still comparable
with OSCEs in previous years.
Moreover, with compulsory quarantine
imposed on all inbound travellers entering Hong
Kong, special arrangements had to be made with
our external examiner, who was based in the United
Kingdom. A list of the patients recruited for OSCE
was sent to the external examiner to evaluate diversity
and appropriateness of cases, and the distinction
viva was conducted over video-teleconferencing
with his presence.
The COVID-19 pandemic has affected all
strata of the healthcare system, and medical schools
are no exception. Organising an in-person real-patient
OSCE was an immense, but not impossible
challenge. We demonstrated that strict infection
control measures and detailed planning, albeit with a
high administrative cost, could provide reassurance
to all OSCE participants, facilitate the smooth
running of the examination, and uphold the standard
we expect from our medical graduates. Lastly,
we should emphasise that good patient rapport
fostered by physicians during routine clinical care is
unarguably a major key to the successful conduction
of our OSCE where our patients have demonstrated
tremendous support and trust in the measures
we have taken. While it remains uncertain when
this pandemic would come to an end, or if social
distancing practices have to be kept indefinitely, our successful experience may provide some guidance
and encouragement to those who are pressing on to
deliver safe and valid qualifying examinations during
one of the most difficult times in this century.
Author contributions
Concept or design: CH Lee, CS Lau, PY Ng, SYY Pang.
Drafting of the manuscript: CH Lee, PY Ng, SYY Pang.
Critical revision of the manuscript for important intellectual content: DCL Lam, CS Lau.
Drafting of the manuscript: CH Lee, PY Ng, SYY Pang.
Critical revision of the manuscript for important intellectual content: DCL Lam, CS Lau.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
CS Lau is Immediate Past President of the Hong Kong
Academy of Medicine. Other co-authors report no conflicts
of interest.
Acknowledgement
We thank the Li Ka Shing Faculty of Medicine for its enduring
support. We are grateful for the efforts and contributions
from all participants, especially our patients, who have made
this objective structured clinical examination possible and
successful.
References
1. Collins JP, Harden RM. AMEE Medical Education Guide
No. 13: real patients, simulated patients and simulators in
clinical examinations. Med Teach 1998;20:508-21. Crossref
2. Boursicot K, Kemp S, Ong TH, et al. Conducting a high-stakes OSCE in a COVID-19 environment. MedEdPublish
2020;9:54.Crossref
3. Centre for Health Protection, Department of Health, Hong Kong SAR Government. Latest situation of cases
of COVID-19. Available from: https://www.chp.gov.hk/files/pdf/local_situation_covid19_en.pdf. Accessed 18 May
2020.
4. Hospital Authority, Hong Kong SAR Government. Hospital
Authority activates Emergency Response Level. Available
from: https://www.ha.org.hk/haho/ho/pad/200125Eng6.pdf. Accessed 25 Jan 2020.
5. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China.
Lancet 2020;395:497-506. Crossref