© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Ureterosciatic hernia with pyonephrosis and
obstructive uropathy: a case report
Clara YC Chan, MB, BS; Terence CT Lai, MB, BS, FCSHK; Chloe HT Yu, MB, BS; Clarence LH Leung, MB, ChB, FCSHK;
Wayne KW Chan, MB, BS, FCSHK; IC Law, MB, BS, FCSHK
Department of Surgery, Kwong Wah Hospital, Hong Kong
Corresponding author: Dr Terence CT Lai (cttlai@yahoo.com.hk)
Introduction
Ureterosciatic hernia is an extremely rare cause of
ureteral obstruction. We report a patient with left
pyonephrosis and obstructive uropathy caused by a
ureterosciatic hernia.
Case report
A 97-year-old woman with a history of ischaemic
stroke, hypertension, hyperlipidaemia, and chronic
obstructive pulmonary disease attended the
Accident and Emergency department of Kwong
Wah Hospital in January 2020 with a 1-day history
of decreased general health and vomiting. She had
no urinary or bowel symptoms. Her vital signs were
stable on admission and physical examination of
her cardiorespiratory and abdominal systems was
unremarkable.
Blood tests on admission revealed acute kidney
injury with serum creatinine level of 387 μmol/L
(baseline 73 μmol/L), leucocytosis (23.8 × 109/L),
and elevated C-reactive protein level of 287 mg/L.
Kidney, ureter, and bladder plain radiograph
revealed the absence of urinary stone. Amoxicillin
with clavulanic acid were administered
intravenously. The following day the patient
developed fever up to 40.1°C with abdominal pain.
Urgent contrast computed tomography scan of the
abdomen and pelvis showed moderate-to-severe left
hydronephrosis (Fig 1) with hydroureter up to 1.4 cm
down to the distal ureter at the level of the left greater
sciatic foramen, where the ureter herniated out
of the pelvis with an abrupt calibre change (Fig 2).
There was reduced enhancement of the left kidney
with no contrast excretion evident on the delayed
phase. Retrograde ureteral stenting was performed
and 30 mL pus was drained from the left kidney.
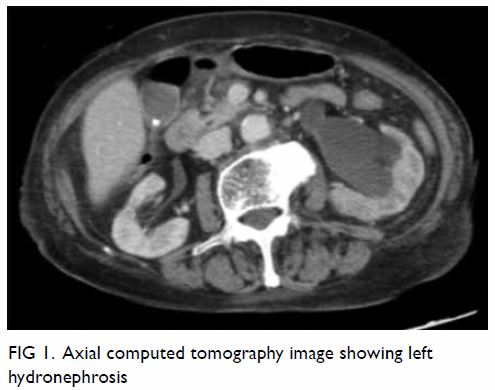
Figure 2. Coronal and axial computed tomography images showing left ureter with herniation into the left sciatic foramen (arrows)
Blood and urine cultures grew Escherichia
coli. The patient recovered gradually with a 2-week
course of antibiotics. The double-J stent was
removed at the end of March (2 months after stent
insertion). However, she developed another episode
of urosepsis shortly afterwards and a double-J stent
was re-inserted. She remained well with regular
revision of double-J stent.
Discussion
Ureterosciatic hernia is a rare disease with no more
than 40 cases published worldwide to date.1 It occurs when the peritoneal sac and its contents (eg, ovary,
small intestine, colon, greater omentum) protrude
through the greater or lesser sciatic foramen.2
When the ureter becomes involved in the herniated
contents, it is called ureterosciatic hernia. The
sacrospinous ligament divides the sciatic notch into
the greater and lesser sciatic foramina. The piriformis
muscle subdivides the greater sciatic foramen into the
suprapiriformis and infrapiriformis compartments.
Ureterosciatic herniation commonly occurs through
the suprapiriformis compartment of the greater
sciatic foramen.2 Herniation of the ureter into the
greater sciatic foramen often results from piriformis
muscle weakening due to increased pressure in the
intra-abdominal area due to pregnancy, constipation,
surgery, trauma, neuromuscular diseases, or hip
disease.3 It commonly develops in elderly women
due to their wider pelvic bones but congenital cases
have also been reported. The left ureter is affected
more often than the right.4
The clinical presentation of ureterosciatic
hernia varies and can range from asymptomatic
to life-threatening urinary sepsis or obstructive
uropathy. Patients may complain of flank or abdominal pain, nausea, and vomiting. A palpable mass over the affected area may be present.2
Since the signs and symptoms of ureterosciatic
hernias are rather non-specific, the diagnosis is
commonly made by radiographic studies including
intravenous urogram, retrograde pyelography, and
computed tomography. Obstruction of the ureter
with U-shaped tortuosity into the sciatic foramina,
also referred to as a “curlicue ureter” sign, is
suggestive of ureterosciatic hernia.5
Treatment options include observation (mostly
for asymptomatic patients), ureteral stenting, and
surgical correction. Open, laparoscopic and robotic
approaches have been described for reduction of the
ureter and hernia repair.1 As our patient was aged 97 years with multiple co-morbidities, surgery was
not considered.
Conclusion
Although seldom seen, ureterosciatic hernias
are occasionally encountered. Diagnosis can be a
challenge given its non-specific symptomatology
and rarity.
Author contributions
Concept or design: All authors.
Acquisition of data: CYC Chan.
Analysis or interpretation of data: CYC Chan.
Drafting of the manuscript: CYC Chan and TCT Lai.
Critical revision of the manuscript for important intellectual content: CYC Chan.
Acquisition of data: CYC Chan.
Analysis or interpretation of data: CYC Chan.
Drafting of the manuscript: CYC Chan and TCT Lai.
Critical revision of the manuscript for important intellectual content: CYC Chan.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This case report received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patient was treated in accordance with the Declaration of Helsinki. The procedure was done under 2MO consent as
the patient’s condition was unstable at the time. Risks of and
indications for the procedure were discussed with the patient’s
daughter who showed understanding and agreed to proceed.
The patient provided consent for publication.
1. Kamisawa K, Ohigashi T, Omura M, Takamatsu K,
Matsui Z. Ureterosciatic hernia treated with laparoscopic
intraperitonization of the ureter. J Endourol Case Rep
2020;6:150-2. Crossref
2. Gandhi J, Lee MY, Joshi G, Smith NL, Khan SA.
Ureterosciatic hernia: an up-to-date overview of evaluation
and management. Translational Research in Anatomy
2018;11:5-9. Crossref
3. Gee J, Munson JL, Smith JJ 3rd. Laparoscopic repair of ureterosciatic hernia. Urology 1999;54:730-3. Crossref
4. Loffroy R, Bry J, Guiu B, et al. Ureterosciatic hernia: a
rare cause of ureteral obstruction visualized by multislice
helical computed tomography. Urology 2007;69:385.e1-3. Crossref
5. Pollack HM, Popky GL, Blumberg ML. Hernias of the ureter—an anatomic-roentgenographic study. Radiology
1975;117:275-81. Crossref

