Hong
Kong Med J 2020 Dec;26(6):492–9 | Epub 16 Dec 2020
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Cross-border reproductive care use by women
with infertility in Hong Kong: cross-sectional
survey
Dorothy YT Ng, MB, BS, FHKAM (Obstetrics and Gynaecology)1,2; Ellen MW Lui, MB, BS, FHKAM (Obstetrics and Gynaecology)1; SF Lai, MB, BS, FHKAM (Obstetrics and Gynaecology)3; Tracy SM Law, MB, BS, FHKAM (Obstetrics and Gynaecology)4; Grace CY Wong, MB, BS, FHKAM (Obstetrics and Gynaecology)5; Ernest HY Ng, MD, FHKAM (Obstetrics and Gynaecology)5
1 Department of Obstetrics and Gynaecology, The University of Hong Kong, Hong Kong
2 Department of Obstetrics and Gynaecology, Pamela Youde Nethersole Eastern Hospital, Hong Kong
3 Department of Obstetrics and Gynaecology, Kwong Wah Hospital, Hong Kong
4 Department of Obstetrics and Gynaecology, Prince of Wales Hospital, Hong Kong
5 The Family Planning Association of Hong Kong, Hong Kong
Corresponding author: Dr Dorothy YT Ng (dor723@gmail.com)
Abstract
Objectives: Cross-border reproductive care (CBRC)
is an increasingly common global phenomenon, but
there is a lack of information regarding its frequency
among residents of Hong Kong. This study aimed to
evaluate the use of CBRC and the factors affecting its
use among residents of Hong Kong.
Methods: This cross-sectional questionnaire study
collected data from 1204 women with infertility who
attended Hong Kong Hospital Authority and Family
Planning Association infertility clinics.
Results: In total, 178 women (14.8% of all
respondents) had used CBRC. Among respondents
who had not used CBRC, 36.3% planned to use or
would consider it. The main factors influencing
the likelihood of using CBRC among women with
infertility in Hong Kong use were long waiting times
in the public sector and high cost in the private
sector. Taiwan was the most preferred destination
for CBRC (69.6% of respondents). Most information
concerning CBRC was accessed via the internet.
More than two thirds of respondents believed that
the government in Hong Kong should formulate
some regulations or guidance regarding CBRC.
Conclusion: Nearly one in six women with infertility in Hong Kong had used CBRC. Among women who had not used CBRC, more than one third planned
to use or would consider it. The main factors
influencing the likelihood of CBRC use were long
waiting times in the public sector and high cost in
the private sector. These results will help clinicians
to more effectively counsel patients considering
CBRC and facilitate infertility services planning by
authorities in Hong Kong.
New knowledge added by this study
- Nearly one in six women with infertility in Hong Kong has used cross-border reproductive care (CBRC). Among women who have not used CBRC, more than one third plan to use CBRC or would consider using CBRC.
- The main factors influencing the likelihood of using CBRC instead of local reproductive care included long waiting times in the public sector and high cost in the private sector.
- More than two thirds of respondents believe that the authorities in Hong Kong should formulate some regulations or guidance regarding CBRC.
- Clinicians should remind patients about the implications of the number of embryos transferred during CBRC and the potential risk of multiple pregnancy.
- The safety of women in Hong Kong who travel abroad for fertility treatment is jeopardised by the current lack of uniform clinical and safety regulations in other parts of the world.
- To ensure fair access to infertility care in Hong Kong, local health authorities should implement more effective measures to manage long waiting lists in the public sector.
Introduction
Cross-border reproductive care (CBRC) is an
increasingly popular global trend in reproductive
medicine, whereby patients travel out of their
home country to receive fertility treatment.1 2
This phenomenon has also been referred to as
“reproductive tourism”, “reproductive travel”, “health
travel”, and “reproductive exile”.3 4 Among these
terms, CBRC has a relatively neutral meaning and
is used in the present study to avoid stigmatisation. Thus far, CBRC has been described in Europe, North
America, Middle East, Australia, and Japan.1 2 3 4 5 6 7 8 9 10 11
A survey in Europe in 2010 showed that there
were 24 000 to 30 000 cycles of CBRC annually,
which involved 11 000 to 14 000 patients.12 13 Because
525 640 total treatment cycles were performed
during the same period, approximately 5% of the
fertility care was estimated to involve CBRC. In
the US, nearly 4% of all fertility treatment provided
was delivered to non-US residents; this comprised
approximately 6000 cycles.13 14 The reasons for
CBRC use in Europe12 included avoidance of legal
restrictions at home (eg, fertility treatment for single
and lesbian women in France and pre-implantation
genetic testing in Germany), avoidance of lengthy
waiting lists at home (eg, for egg donation in
the United Kingdom), lower treatment cost, and
treatment within a more favourable framework (eg,
gamete donation with donor anonymity).
The aim of the present study was to evaluate
the use of CBRC and its influencing factors in Hong
Kong.
Methods
Participants
Women with infertility who attended infertility
clinics in the Hospital Authority (ie, Queen Mary
Hospital, Pamela Youde Nethersole Eastern Hospital,
Kwong Wah Hospital, and Prince of Wales Hospital)
and the Family Planning Association (FPA) from
1 February 2017 to 31 March 2019 were recruited to participate in the study. Women who could not
read English or Chinese were excluded from the
study. All participants provided written informed
consent to participate. The study was approved by
the Institutional Review Boards of all participating
centres, including the Hong Kong East Cluster Ethics
Committee (HKECREC-2018-014); The University
of Hong Kong Hong Kong West Cluster Clinical
Research Ethics Committee (UW 18-266); Kowloon
Central/Kowloon East Cluster Clinical Research
Ethics Committee (KC/KE-18-0073/ER-4); North
Territories East Cluster Clinical Research Ethics
Committee (NTEC-2018-0384); and the Ethics
Panel and the Health Services Subcommittee of the
FPAHK (OA1-2).
Questionnaire development and distribution
A search of the literature was conducted using
PubMed using the terms “cross border reproductive
care”, “reproductive travel”, “infertility”, and
“Hong Kong”. It revealed no existing validated
questionnaires concerning CBRC use in Hong Kong.
Most questions in our questionnaire were adapted
from another questionnaire focused on CBRC.5 The
questionnaire content focused on three main areas:
(1) demographic information, (2) reproductive
history and attitudes concerning fertility, and (3)
factors affecting the use of CBRC. The questionnaire
was evaluated and revised by specialists in Obstetrics
and Gynaecology and subspecialists in Reproductive
Medicine, all of whom worked in the Hospital
Authority. It was then piloted by administration to
five patients in the clinic with the aim of ensuring
that patients could understand the questionnaire.
Women with infertility who attended infertility
clinics in the Hospital Authority or FPA were invited
to participate in the study. The questionnaire was
distributed by clinic nurses to clinic attendees.
Participation was voluntary and patients were
invited to complete the questionnaire without
assistance while awaiting medical consultation. The
questionnaire required approximately 20 minutes to
complete. Completed questionnaires were returned
to the clinic nurse at the end of the consultation.
Statistical analysis
Calculations were performed using SPSS Statistics
for Windows, version 25.0 (IBM Corp, Armonk [NY],
US). Associations between attitudes towards CBRC
and background variables (total monthly household
income, education level, years of attempting
conception, and age) were explored using the Chi
squared test. P values <0.05 were considered to
indicate statistical significance. Logistic regression
was used to investigate whether respondent age,
education level, years of attempting conception, and
total monthly household income were associated
with CBRC use.
Results
Respondent characteristics
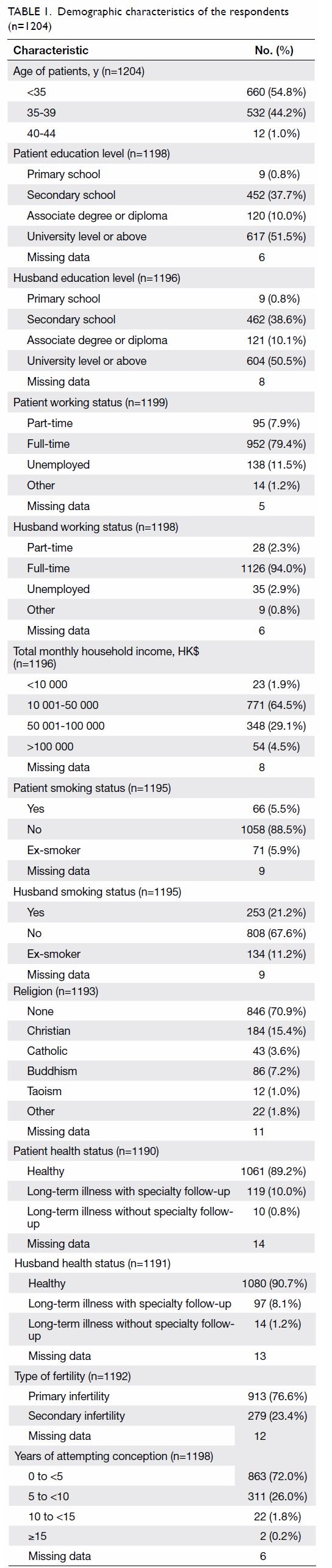
In total, 1204 questionnaires were returned (Table 1):
175 (14.5%) from Pamela Youde Nethersole Eastern
Hospital, 510 (42.4%) from Queen Mary Hospital,
293 (24.3%) from Kwong Wah Hospital, 146 (12.1%)
from Prince of Wales Hospital, and 80 (6.6%) from
the FPA. The mean age (±standard deviation) of
the respondents was 34.7±6.8 years. Among the
1204 respondents, 913 women (76.6%) had primary
infertility and 279 women (23.4%) had secondary
infertility. Thirty one women had an existing child.
All respondents indicated that they were married;
the shortest duration was 0.2 years. This finding was
presumably influenced by the marriage requirement
for intrauterine insemination (IUI) and in vitro
fertilisation (IVF) in Hong Kong. Concerning the
duration of attempted conception, 863 women
(72.0%) had been actively trying for fewer than
5 years, 311 women (26.0%) had been actively trying
for 5 years to fewer than 10 years, 22 women (1.8%)
had been actively trying for 10 years to fewer than
15 years, and two women (0.2%) had been actively
trying for 15 years or more.
There were missing data in our study involving
non-responses to some questionnaire components.
The missing data exhibited a random pattern and
did not cluster around a particular question. Because
the number of missing values was small (<5%), these
values were omitted from further analyses.
Reproductive history and attitudes
concerning fertility
Overall, 1051 respondents (87.3%) reported
unremarkable medical histories. The cause of
infertility was unexplained in 516 respondents
(43.0%, 516/1200), related to the male partner in
216 respondents (18.0%, 216/1200), caused by a
tubal factor in 181 respondents (15.1%, 181/1200),
and caused by anovulation in 103 respondents (8.6%,
103/1200). The remaining respondents noted that
infertility was attributed to endometriosis, other
factors, or unknown (ie, no previous consultation).
Notably, 578 respondents (48.0%, 578/1204) or
their partners were unwilling to accept adoption.
When asked to rank the importance of having a
child, 382 respondents (31.7%, 382/1204) reported
a score of 10/10 (very important). Furthermore,
300 respondents (24.9%, 300/1204) reported that
having a child was very important to their marital
relationship (score of 10/10). Finally, 351 respondents
(29.2%, 351/1204) felt that having a child was very
important to their family members (score of 10/10).
Use of cross-border reproductive care and
factors affecting its use
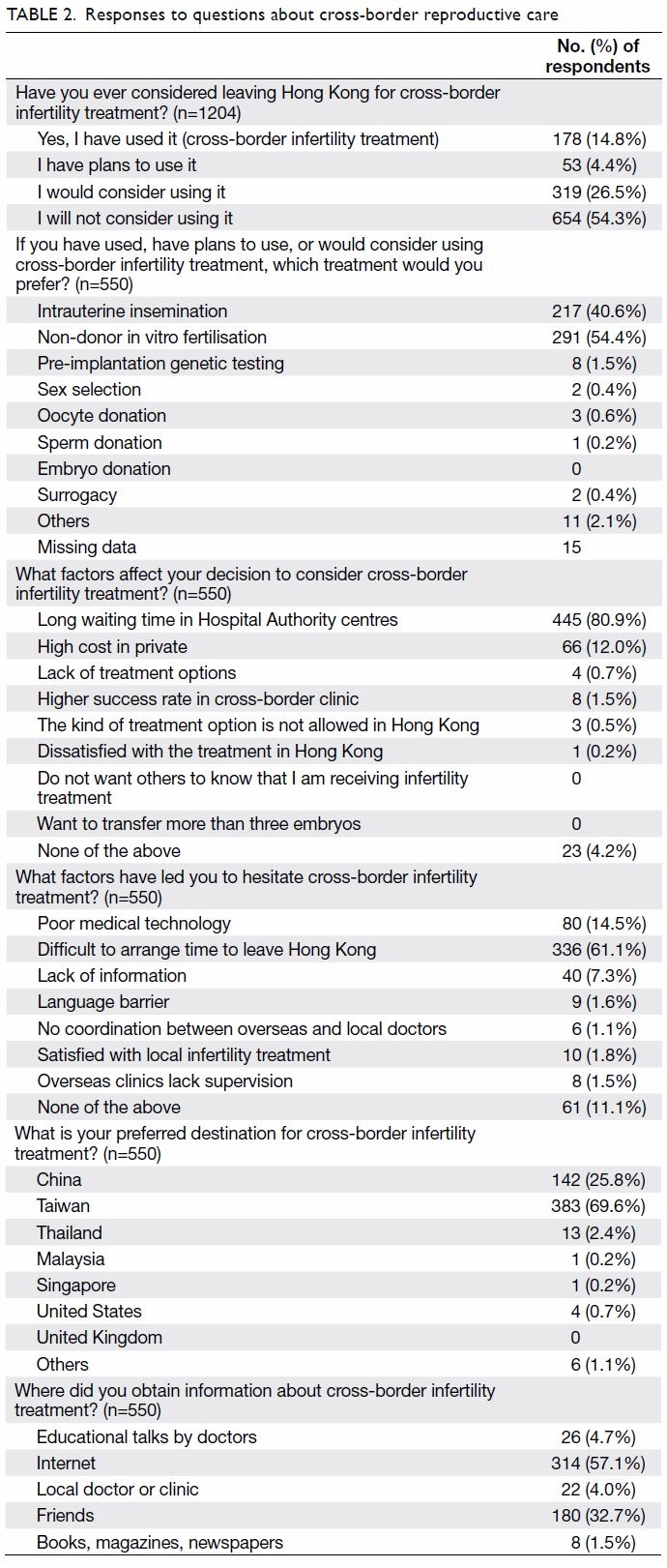
In total, 178 women (14.8% of total respondents) had used CBRC (Table 2). Among respondents who had
not used CBRC, 36.3% (372/1026) were planning
or would consider it. The 550 respondents who had
previously used CBRC, were planning for CBRC, or
would consider CBRC were then asked to choose
one reproductive technology that they preferred for
use in CBRC; 54.4% selected non-donor IVF as their
treatment of choice. In all, 40.6% of these respondents
showed interest in IUI; only 0.6% showed interest
in oocyte donation, 0.2% showed interest in sperm
donation, and 0.4% showed interest in surrogacy for
CBRC.
The two main factors positively influencing
its use (ie, motivational factors) were long waiting
times in the public sector and high treatment costs
in the private sector, reported by 80.9% (445/550)
and 12.0% (66/550), respectively, of the respondents
who had used or would consider CBRC. Only 0.5%
(3/550) of the respondents reported law evasion as a
positive influence for the use of CBRC.
Most respondents indicated that Taiwan was
their preferred destination (69.6%; 383/550); China
was the second-most preferred destination (25.8%;
142/550).
Most respondents who had used or would
consider CBRC (61.1%; 336/550) felt that it was
difficult to allocate time for CBRC. In total, 14.5%
of these respondents (80/550) had a suspicion of
substandard medical technology in the destination
countries. Some respondents were worried about
a language barrier and the lack of communication
between local doctors and doctors in the destination
countries.
Source of information
Respondents accessed information concerning
CBRC through multiple channels (Table 2). Among
the respondents who had used or would consider
CBRC, more than half (57.1%; 314/550) accessed
information from the internet; 32.7% (180/550)
obtained relevant information from their friends.
Notably, only 4.0% of these respondents (22/550)
obtained information concerning CBRC from
professional sources (eg, local fertility clinics).
Fertility treatment during cross-border
reproductive care
Among respondents who had used or would
consider CBRC (n=550), 340 (61.8%) indicated that
they had received local counselling from their home
country to assist in CBRC treatment. Among the
178 respondents who had previously used CBRC, 67
(37.6%) had some involvement from local doctors in
their home country during CBRC treatment.
Among respondents who had engaged in CBRC
and reached the point of embryo transfer (n=59),
40 (67.8%) had undergone transfer of two embryos.
Surprisingly, 10 women (16.9%) had undergone transfer of three embryos and three women (5.1%)
had undergone transfer of four embryos.
Among the 178 respondents who had used
CBRC, three (1.7%) had ovarian hyperstimulation
syndrome and three (1.7%) had other types of
complications. Overall, 70.2% of the respondents
believed that the authorities in Hong Kong should
formulate some regulations or guidance regarding
CBRC.
Respondent characteristics influencing use of
cross-border reproductive care
Associations between attitudes towards CBRC and
background variables were also explored using
the Chi squared test. Respondents who had a total
monthly household income above >HK$100 000
were more likely to consider CBRC than those who had total monthly household income of ≤HK$100 000
(P<0.001). Respondents who had a university degree
or above were also more likely to consider CBRC
than those who had education below university level
(P<0.001). Respondents who had been attempting
conception for ≥5 years had a similar likelihood
of CBRC use, compared with those who had been
attempting conception for <5 years. Respondents
aged ≥35 years had a similar likelihood of CBRC use,
compared with those aged <35 years.
Logistic regression analysis of factors
potentially associated with CBRC use revealed
no relationships with respondent age, education,
years of attempting conception, or total monthly
household income.
Discussion
To the best of our knowledge, this is the first study
concerning the use of CBRC and factors affecting
its use in Hong Kong. Nearly one in six women
with infertility had used CBRC and approximately
one-third of the respondents planned to use or
would consider it. The main factors influencing the
likelihood of CBRC use, instead of local reproductive
care, included long waiting times in the public sector
and high cost in the private sector. Over half of the
respondents accessed information from the internet.
More than two thirds of respondents believed that
the authorities in Hong Kong should formulate some
regulations or guidance regarding CBRC.
Comparison with other regions
It is difficult to compare the use of CBRC in Hong
Kong with that in Europe (5%) and the US (4%); the
methodologies have differed among studies and the
extent of CBRC use in Hong Kong was not fully
established in the present study. Where women in
Europe frequently engage in CBRC for purposes of
law evasion, women in Hong Kong appear to engage
in CBRC primarily because of the long waiting lists
for public fertility treatment. In a survey of European
women, law evasion was a concern for 55% of
women using CBRC (9% of patients in the UK, 65%
in France, 71% in Italy, and 80% in Germany).12
Specific assisted reproduction treatment, such as
surrogacy or oocyte donation, is prohibited in some
countries (eg, Italy, Germany, and Japan), but legal
in other countries (eg, Belgium, India, and the US).
We found that only 0.5% of women in Hong Kong
travelled for purposes of law evasion. This may be
partly explained by the legal availability of gamete
donation and surrogacy in Hong Kong (although
no treatment centres in Hong Kong an appropriate
licence to offer surrogacy). Because of differences in
cultural backgrounds, compared with prior studies,
women in Hong Kong may be less interested in
gamete donation (eg, in relation to their traditional
Chinese beliefs).
Fertility treatment options
Surprisingly, many respondents in our study
engaged in IUI during CBRC. Among respondents
in this subgroup, the two main motivational factors
were identical: long waiting times in the public
sector and high treatment costs in the private sector.
The waiting time for IUI in public hospitals within
the Hospital Authority may be longer than many
patients prefer; this includes the waiting time for
the initial consultation, required examinations,
and subsequent waiting list for IUI treatment. The
treatment cost of IUI is much lower than that of IVF
in the private sector, but may be prohibitive for many
patients from lower and middle social classes. We
also acknowledge possible misconceptions among
our respondents, who may presume that IUI is
always the first-line approach or must be performed
prior to IVF.
Among women who had previously engaged
in non-donor IVF during CBRC, 33.1% were
aged <35 years. Among all the respondents who
engaged in CBRC, 30% of the respondents were
aged <35 years and had unexplained infertility.
Given the large percentage of young women with
unexplained infertility who actually engaged in
IVF during CBRC, it is unclear whether there is
an overtreatment problem or inappropriate use
of IVF treatment during CBRC. However, the
treatment of unexplained infertility is empirical.
A recent Cochrane systemic review revealed
insufficient evidence for differences in live birth
between expectant management and the other four
interventions (ovarian stimulation, IUI, stimulated
IUI, and IVF).15 For most couples, the American
Society of Reproductive Medicine recommends that
the preferred initial therapy is three or four cycles
of ovarian stimulation with oral medications and
IUI, followed by IVF for those unsuccessful with
stimulated IUI treatments.16 In contrast, the 2013
guidelines of the National Institute for Health and
Care Excellence recommend IVF treatment for
women with unexplained infertility who have not
conceived after 2 years of regular unprotected sexual
intercourse. Therefore, stimulated IUI and IVF are
both appropriate treatment options for unexplained
infertility as the first-line therapy after adequate
counselling.17
Pre-implantation genetic testing is increasingly
used to detect genetic abnormalities in embryos,
thus allowing replacement with normal embryos.
Pre-implantation genetic testing is useful when
prospective parents either have or are carriers of a
genetic disease that is potentially transmissible to
their offspring. A small proportion of the patients
in our study (1.5%) had engaged or were interested
in CBRC for pre-implantation genetic testing. In
Hong Kong, pre-implantation genetic testing is
permitted for medical indications and is available in Queen Mary Hospital, Prince of Wales Hospital, and
some private assisted reproduction centres. Because
it is legal and available in Hong Kong, few of our
respondents reported a desire to engage in CBRC for
pre-implantation genetic testing. A small percentage
of patients (0.4%) reported a desire to engage in
CBRC for sex selection. Notably, sex selection of
embryos for non-medical reasons is prohibited in
Hong Kong and many Western countries; however,
it is allowed in the US.
Destinations and sources of information
Our results found that the most popular CBRC
destination for Hong Kong couples with infertility
was Taiwan. This may be due to the presence of
Taiwanese agencies established in Hong Kong who
provide local couples with the option of going to
Taiwan to undergo CBRC. It may also be associated
with the close proximity, relatively lower costs, and
potential family ties involving Taiwan.
Importantly, we found that the internet was
the major source of information for women in
Hong Kong seeking CBRC. Women who intended
to go abroad sought information concerning CBRC
primarily via the internet, rather than from their
local doctors or fertility clinics. This phenomenon is
consistent with the findings in another study, which
reported that the internet was the main source
of information for Swedish, German, and British
women seeking CBRC.12
Multiple births
For respondents who had engaged in CBRC and
reached the point of embryo transfer, the majority
had undergone transfer of two embryos. An alarming
result of our study was that one of the patients
had undergone transfer of four embryos. High-order
multiple pregnancies can potentially cause
significant morbidity and mortality for the mother
and the baby. To reduce the likelihood of multiple
births, some countries/places (eg, the United
Kingdom and Hong Kong) have placed restrictions
on the number of embryos transferred during each
cycle. A previous survey found that 14 countries had
an upper limit of three embryos, 12 had a limit of four,
and six had a limit of five.18 This indicates that CBRC
may pose an increasing challenge for obstetricians
and paediatricians due to the increasing likelihood
of higher multiple pregnancies from CBRC, which
indirectly leads to a burden on the local healthcare
system. Clinicians should remind patients about the
implications of the number of embryos transferred
during CBRC and the potential risk of multiple
pregnancy.
Benefits and challenges involving cross-border
reproductive care
Potential advantages to CBRC include that it provides an equal opportunity for treatment, thus improving
patient autonomy; however, that autonomy may
come at a cost or involve law invasion. Cross-border
reproductive care also illustrates the principle of
freedom of patient movement, as set out in a 2008
Directive of the European Commission.19
The largest potential problem related to CBRC
involves patient health and safety. In the context of
assisted reproduction treatment, this could include
multiple pregnancies, ovarian hyperstimulation
syndrome, and infectious disease transmission.
The lack of uniform clinical and safety regulations
worldwide is further complicated by the lack of
policies to govern CBRC. This could mean that
patients are disadvantaged, such that they cannot
receive information or services that are of a minimum
quality standard. The lack of knowledge provided
to patients could inhibit their ability to discover
potential services. It is often difficult for a patient
to assess the standard of quality of a fertility clinic
in another country, in terms of infection screening
measures, embryology laboratory quality, and risk
management measures (eg, gamete and embryo
handling). Therefore, patients assume greater risk
when they engage in CBRC, compared with fertility
treatment in their home country, because of the
difference in accessible information. The safety of
women in Hong Kong who travel abroad for fertility
treatment is jeopardised by the current lack of
uniform clinical and safety regulations in other parts
of the world.
Strategies to reduce risks associated with
cross-border reproductive care
Strategies to minimise the negative impact of CBRC
should focus on each of the relevant stakeholders:
patients, clinicians, and local regulatory bodies. First,
patients who are interested in CBRC should obtain
more information prior to engaging in CBRC. They
should be aware of the potential complications and
the success rate in the destination country centre,
then make informed choices for themselves when
embarking on fertility treatment in another country.
Second, clinicians must educate their patients
about the potential risks of CBRC. Clinicians who
are collaborating with doctors in other countries
to facilitate in CBRC should formulate a clear plan
concerning the role of patient management, ensuring
that patients’ best interests are respected. Clinicians
should also resume care of a patient who has
returned after receiving CBRC treatment, especially
if that patient has encountered complications from
fertility treatment during CBRC. Third, in Europe,
the European Society of Human Reproduction and
Embryology has published a good practice guide
for CBRC for centres and practitioners.2 Such
guidelines can help regulators and policy makers
create a framework to enable centres to abide by these rules. The Hong Kong SAR Government can
also formulate guidance for clinicians and publish
advice for patients who are considering CBRC,
particularly highlighting the potential problems of
CBRC. Over two thirds of respondents in the present
study believed that authorities in Hong Kong should
formulate some regulations or guidance regarding
CBRC.
Limitations and implications
This study had a number of limitations. First, it
included patients with infertility who were not
pregnant at the time of consultation. Patients who
had a successful pregnancy following CBRC would
not attend infertility clinics; hence, they would not
be included in our sample. This could have led to
an underestimation of the use of CBRC. Second,
this study only involved heterosexual couples who
were legally married, which was a prerequisite for
receiving assisted reproduction in Hong Kong. The
study did not include single women, single men,
or same-sex couples in Hong Kong who probably
engaged in CBRC for gamete donation or surrogacy.
Third, the infertility centres in this study cannot be
considered representative of all infertility centres in
Hong Kong. A relatively small number of patients
were recruited. A territory-wide study should be
performed to further evaluate the state of CBRC in
Hong Kong.
Notably, the European Society of Human
Reproduction and Embryology recognises that ideal
reproductive care involves fair access to good quality
treatment in a patient’s home country.2 To ensure fair
access to infertility care in Hong Kong, the waiting
lists in the public sector should be shortened. Based
on the results of this questionnaire study, the current
CBRC trend in Hong Kong will presumably continue
until the local health authorities implement more
effective measures to manage the long waiting lists
in the public sector. Patient education on this topic
should also be improved.
Conclusion
Nearly one in six women with infertility in Hong
Kong had used CBRC. Among women who had not
used CBRC, more than one third had planned to use
or would consider it. The main factors influencing
the likelihood of using CBRC instead of local
reproductive care included long waiting times in
the public sector and high cost in the private sector.
These results will help clinicians to more effectively
counsel patients considering CBRC and facilitate
infertility services planning by authorities in Hong
Kong.
Author contributions
Concept or design: DYT Ng, EHY Ng.
Acquisition of data: All authors.
Analysis or interpretation of data: DYT Ng, EHY Ng.
Drafting of the manuscript: DYT Ng, EHY Ng.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: DYT Ng, EHY Ng.
Drafting of the manuscript: DYT Ng, EHY Ng.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the
study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
We would like to express our gratitude to Ms Merie Yuen,
project nurse of University of Hong Kong for data collection
and entry.
Funding/support
This research received no specific grant from any funding
agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The study was approved by the Institutional Review Boards
of all participating centres, including the Hong Kong East
Cluster Ethics Committee (HKECREC-2018-014); The
University of Hong Kong Hong Kong West Cluster Clinical
Research Ethics Committee (UW 18-266); Kowloon Central/Kowloon East Cluster Clinical Research Ethics Committee
(KC/KE-18-0073/ER-4); North Territories East Cluster
Clinical Research Ethics Committee (NTEC-2018-0384); and
the Ethics Panel and the Health Services Subcommittee of the
FPAHK (OA1-2).
All participants provided written informed consent to
participate in the questionnaire study.
References
1. Inhorn MC, Patrizio P. The global landscape of cross-border reproductive care: twenty key findings for the new
millennium. Curr Opin Obstet Gynecol 2012;24:158-63. Crossref
2. Shenfield F, Pennings G, de Mouzon J, Ferraretti AP,
Goossens V, ESHRE Task Force ‘Cross Border Reproductive
Care’ (CBRC). ESHRE’s good practice guide for cross-border
reproductive care for centers and practitioners.
Hum Reprod 2011;26:1625-7. Crossref
3. Inhorn MC, Patrizio P. Rethinking reproductive ‘‘tourism’’
as reproductive ‘‘exile’’. Fertil Steril 2009;92:904-6. Crossref
4. Mattorras R. Reproductive exile versus reproductive
tourism. Hum Reprod 2005;20:3571. Crossref
5. Culley L, Hudson N, Rapport F, Blyth E, Norton W,
Pacey AA. Crossing borders for fertility treatment:
motivations, destinations and outcomes of UK fertility
travellers. Hum Reprod 2011;26:2373-81. Crossref
6. Gomez VR, de La Rochebrochard E. Cross-border
reproductive care among French patients: experiences in
Greece, Spain and Belgium. Hum Reprod 2013;28:3103-10. Crossref
7. Gürtin ZB. Banning reproductive travel: Turkey’s ART
legislation and third party assisted reproduction. Reprod
Biomed Online 2011;23:555-64. Crossref
8. Bergmann S. Reproductive agency and projects: Germans
searching for egg donation in Spain and the Czech
Republic. Reprod Biomed Online 2011;23:600-8. Crossref
9. Hughes EG, Dejean D. Cross-border fertility services
in North America: a survey of Canadian and American
providers. Fertil Steril 2010;94:e16-9. Crossref
10. Inhorn MC, Shrivastav P, Patrizio P. Assisted reproductive
technologies and fertility ‘‘tourism”: examples from global
Dubai and the Ivy League. Med Anthropol 2012;31:249-65. Crossref
11. Yuri H, Yosuke S, Yasuhiro K, Yoshiaki H, Hiroyuki N.
Attitudes towards cross-border reproductive care among
infertile Japanese patients. Environ Health Prev Med
2013;18:477-84. Crossref
12. Shenfield F, de Mouson J, Pennings G, et al. Cross border
reproductive care in six European countries. Hum Reprod
2010;25:1361-8. Crossref
13. Hudson N, Culley L, Blyth E, Norton W, Rapport F,
Pacey A. Cross-border reproductive care: a review of the
literature. Reprod Biomed Online 2011;22:673-85. Crossref
14. National Center for Chronic Disease Prevention and
Health Promotion, Division of Reproductive Health, US
Government. 2013 Assisted reproductive technology:
national summary report 5 (2015). Available from: http://www.cdc.gov/art/pdf/2013-report/art_2013_national_summary_report.pdf. Accessed 4 Dec 2019.
15. Wang R, Danhof NA, Tjon-Kon-Fat RI, et al. Interventions
for unexplained infertility: a systematic review and
network meta-analysis. Cochrane Database Syst Rev
2019;(9):CD012692. Crossref
16. Practice Committee of the American Society for
Reproductive Medicine. Evidence-based treatments for
couples with unexplained infertility: a guideline. Fertil
Steril 2020;113:305-22. Crossref
17. National Collaborating Centre for Women’s and Children’s
Health (UK). Fertility: Assessment and Treatment for
People with Fertility Problems. London: Royal College of
Obstetricians and Gynaecologists; 2013.
18. International Federation of Fertility Societies. Global
Reproductive Health: IFFS Surveillance 2016. September
2016. Available from: https://journals.lww.com/grh/Fulltext/2016/09000/IFFS_Surveillance_2016.1.aspx. Accessed 4 Dec 2019.
19. Commission of the European Communities. Proposal
for a Directive of the European Parliament and of the
Council on the application of patients’ rights in cross-border
healthcare. 2008. Available from: http://ec.europa.eu/health/ph_overview/co_operation/healthcare/docs/COM_en.pdf. Accessed 4 Dec 2019.