Hong
Kong Med J 2020 Dec;26(6):500–9 | Epub 11 Dec 2020
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Safety and efficacy of magnetic seed localisation
of non-palpable breast lesions: pilot study in a
Chinese population
WY Fung, MB, ChB, FRCR1; T Wong, MB, ChB, FHKCR1; CM Chau, MB, BS, FHKCR1; Ellen LM Yu, BSc, MSc2; TS Chan, MB, BS, FHKCR1; Rois LS Chan, MB, BS, FHKCR1; Alfred WT Yung, MB, BS, FHKCR1; Johnny KF Ma, MB, BS, FHKCR1
1 Department of Radiology, Princess Margaret Hospital, Hong Kong
2 Clinical Research Centre, Princess Margaret Hospital, Hong Kong
Corresponding author: Dr WY Fung (fwyyuk@gmail.com)
Abstract
Introduction: A magnetic seed marker system
(Magseed, Endomagnetics, Cambridge, United
Kingdom) is used as a localisation method for non-palpable
breast lesions in the United States, Europe,
and Hong Kong. It overcomes many limitations of
conventional techniques and allows scheduling
flexibility. We sought to evaluate its efficacy and
safety in the Chinese population.
Methods: We retrospectively reviewed all Chinese
women who underwent magnetic seed marker–guided breast lesion excision from June 2019 to
February 2020 at a single institution. Placement
success (final target-to-seed distance <10 mm) was
evaluated by imaging on the day of surgery. Specimen
radiographs and pathology reports were reviewed for
magnetic seed markers and target removal. Margin
clearance and re-excision rates were analysed.
Results: Twenty two magnetic seed markers
were placed in 21 patients under sonographic or
stereotactic guidance to localise 21 target lesions.
One target lesion required two magnetic seed
markers for bracketing. There was no migration
of nine markers placed 6 to 56 days before the day
of surgery. Placement success was achieved in
20 (90.9%) cases. Mean final target-to-seed distance
was 3.1 mm. Two out of 21 (9.5%) lesions required alternative localisation due to marker migration
>=10 mm, while 19 (90.5%) lesions underwent
successful magnetic seed marker-guided excision.
Three of these 19 lesions (15.8%) were excised with
therapeutic intent, one of which (33%) required
re-excision due to a close margin. All 22 magnetic
seed markers were successfully removed. No
complications were reported.
Conclusion: Magnetic seed markers demonstrated
safety and efficacy in Chinese women for breast
lesion localisation and excision.
New knowledge added by this study
- The magnetic marker system is an accurate and safe method to localise and excise non-palpable breast lesions.
- This is the first study reporting high placement success and retrieval rate without any reported complications in a Chinese population.
- The magnetic marker system addresses many limitations associated with conventional localisation methods such as hookwire and radioguided occult lesion localisation. The deployment procedure is approved to be performed up to 30 days before the surgical procedure in Hong Kong, and as long-term implantation in the United States and Europe.
- The lack of any external component overcomes the disadvantages of wire localisation including wire kinking, transection, migration, and breakage.
- Magnetic seed markers are non-radioactive, thus no support from the nuclear medicine unit is necessary and radiation exposure to staff and patients can be minimised.
Introduction
With the increasing use of screening mammography
and advances in neoadjuvant therapy, tumours at
the time of surgery are more often non-palpable.1 2 3 4 5 6 7
Accurate image-guided localisation is the key to
successful excision of these lesions.
Hookwire localisation has been the traditional
standard method of localising non-palpable breast
lesions for decades. It has many inherent limitations
and challenges. Wire placement has to be done
on the day of surgery to minimise the risk of wire
dislodgment, which limits the flexibility of radiology appointments and scheduling of surgery, therefore
potentially resulting in delayed surgery.8 Wire
displacement and wire transection with retained
fragments have also been reported.5 9 10 The track
of the wire limits the surgical approach, causing
additional healthy breast tissue to be dissected along
the course of the wire.5 9 10 These can affect cosmetic
outcome.5 9 10
More recently, radioguided occult lesion
localisation (ROLL) has gained popularity, as it
overcomes many disadvantages of wire localisation
and is reported to be equally effective compared to
hookwire.11 However, it also needs to be performed
on the same day or a day before surgery due to the
half-life of the radiotracer.12 Moreover, radiation
safety precautions and the need of Nuclear Medicine
unit support limit its widespread use.
Recently, non-radioactive non-wire techniques
have started to emerge and address many of these
issues. A magnetic marker system (Magseed,
Endomagnetics, Cambridge, United Kingdom) is one
of these techniques and received clearance for longterm
breast implantation from United States Food
and Drug Administration in February 2018. It was
introduced in Hong Kong in 2019. Our study aimed
to evaluate the efficacy and safety of magnetic seed
marker localisation of non-palpable breast lesions.
To the best of our knowledge, there is no prior publication on magnetic seed marker localisation in
a Chinese population.
Methods
A retrospective review of all Chinese women who
underwent magnetic seed marker localisation for
non-palpable breast lesions from June 2019 to
February 2020 in a single institution was conducted.
Patients were selected by breast surgeons and breast
radiologists in consensus by reviewing images on the
basis of target visibility and target depth. Patients
who had a magnetic seed marker placed but surgery
performed out of the study period were excluded.
Magnetic marker system
The magnetic seed marker (Magseed, Endomagnetics,
Cambridge, United Kingdom) is made of non-radioactive
paramagnetic low-nickel stainless steel.
The seed is 5 mm × 0.9 mm, which is the smallest
non-wire non-radioactive localisation device
available. The magnetic seed marker is preloaded in
a sterile 7- or 12-cm 18-gauge deployment needle.
The magnetic seed marker is intended to
be placed at a depth up to 3 cm from the skin
according to the manufacturer’s instructions13 due
to limitations of signal transmission from a greater
depth. It is localised with a detector probe (Sentimag,
Endomagnetics), which generates an alternating
magnetic field to transiently magnetise the seed.14
A visual numerical value and audio feedback are
produced according to the strength of the magnetic
field, thus signalling the distance of the seed from
the detector probe.14
Localisation procedure
Magnetic seed marker placement was percutaneously
performed under image guidance by one of four
breast radiologists with 3 to 19 years of experience
performing image-guided breast localisation, or
by a breast radiology trainee who was directly
supervised by one of the breast radiologists. During
ultrasound-guided placement, the patient lies supine
and rolled slightly with a wedge put under the
shoulder on the ipsilateral side to spread the breast
evenly. The ipsilateral arm is raised over the patient’s
head to facilitate a larger sterilisation field. During
stereotactically guided placement, the patient lies on
either side or sits up to facilitate breast compression
by the stereotactic table.
Target-to-seed distance was evaluated in
real time for magnetic seed markers placed under
sonographic guidance and was measured on post-procedure
mammograms in mediolateral and
craniocaudal projections for magnetic seed markers
placed under stereotactic guidance. If multiple
magnetic seed markers were placed in one breast,
the minimum distance between the markers was measured. For patients with magnetic seed markers
inserted before the day of surgery, target ultrasound
and/or mammography were performed on the day
of surgery to evaluate for any delayed magnetic
seed marker migration, which was defined by any
difference between the initial target-to-seed distance
after the localisation procedure and the final target-to-seed distance on the day of surgery. If the final
target-to-seed distance was >=10 mm, signifying
significant migration, alternative localisation was
performed on the day of surgery. Lesions with
acceptable marker position underwent marker-guided
excision as planned with the depth of the
marker from the skin evaluated by preoperative
ultrasound, followed by intraoperative guidance with
the use of the probe. The presence of the markers
in the specimens was confirmed with the probe by
surgeons and by specimen radiographs with the
radial margins evaluated.
Outcome analysis
Rates of placement success and retrieval success with
a 95% confidence interval (CI) were calculated using
the Wilson score method.15 Placement success was
defined as a final target-to-seed distance <10 mm
in any plane on images on the day of surgery, with
reference to guidelines from the National Health
Service Breast Screening Programme16 and previous
studies.14 17 For degrees of magnetic seed marker
placement success, the final target-to-seed distances
were further subdivided into ≤1 mm, 2 to 5 mm,
and 5 to 9 mm. Retrieval success was determined by
the presence of the magnetic seed marker(s) in the
specimen radiograph.
Electronic patient records were reviewed for
patients’ demographics, preoperative pathology
(if any), and indications for surgery. Specimen
radiographs and pathology reports were reviewed to
verify excision of target lesions and to evaluate the
resection margins.
The target lesions were divided into two groups
according to the indications for surgery. The surgery
was considered to be of therapeutic intent if the
target lesion had been proven to be malignant from
preoperative pathology. Otherwise, the surgery was
considered to be of diagnostic intent. Among the
surgeries with therapeutic intent, margin clearance,
defined as at least 1-mm disease-free margins, was
assessed. The re-excision rate due to inadequate
margin clearance was analysed. Complications
related to magnetic seed marker deployment and
surgeries were recorded.
Results
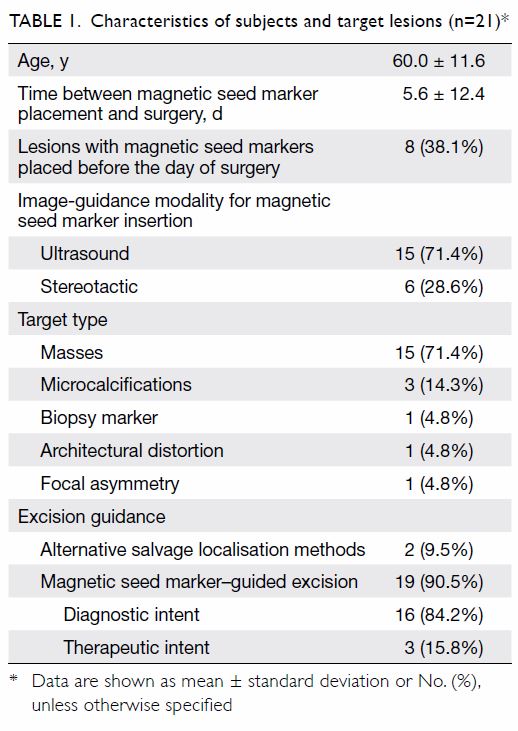
There were 22 Chinese patients with magnetic
seed markers placed during the study period; one
patient was excluded due to deferred surgery out
of the study period (Fig 1a). A total of 21 patients, with mean age 60.0 years (range, 38-73 years)
were included (Table 1). Thirteen patients (61.9%)
each had one magnetic seed marker placed on the
day of surgery, which were performed during the
initial learning period of this new technique. Eight
patients (38.1%) had nine magnetic seed markers
inserted before the day of surgery in out-patient setting, ranging from 6 to 56 days from surgery with
a median of 8 days (interquartile range=6.25-13.75)
[Fig 1b]. Fifteen out of 22 magnetic seed markers
(68.2%) were placed under ultrasound guidance, and
seven magnetic seed markers (31.8%) were placed
under stereotactic guidance. The most common type
of target lesion was a solid mass (15 of 21, 71.4%),
all of which had markers placed under ultrasound
guidance. The other six lesions had magnetic seed
markers placed by stereotactic guidance, including
three groups of microcalcifications, one biopsy
marker, one architectural distortion, and one focal
asymmetry. One group of calcifications required
two magnetic seed markers for bracketing due to its
extensive distribution.
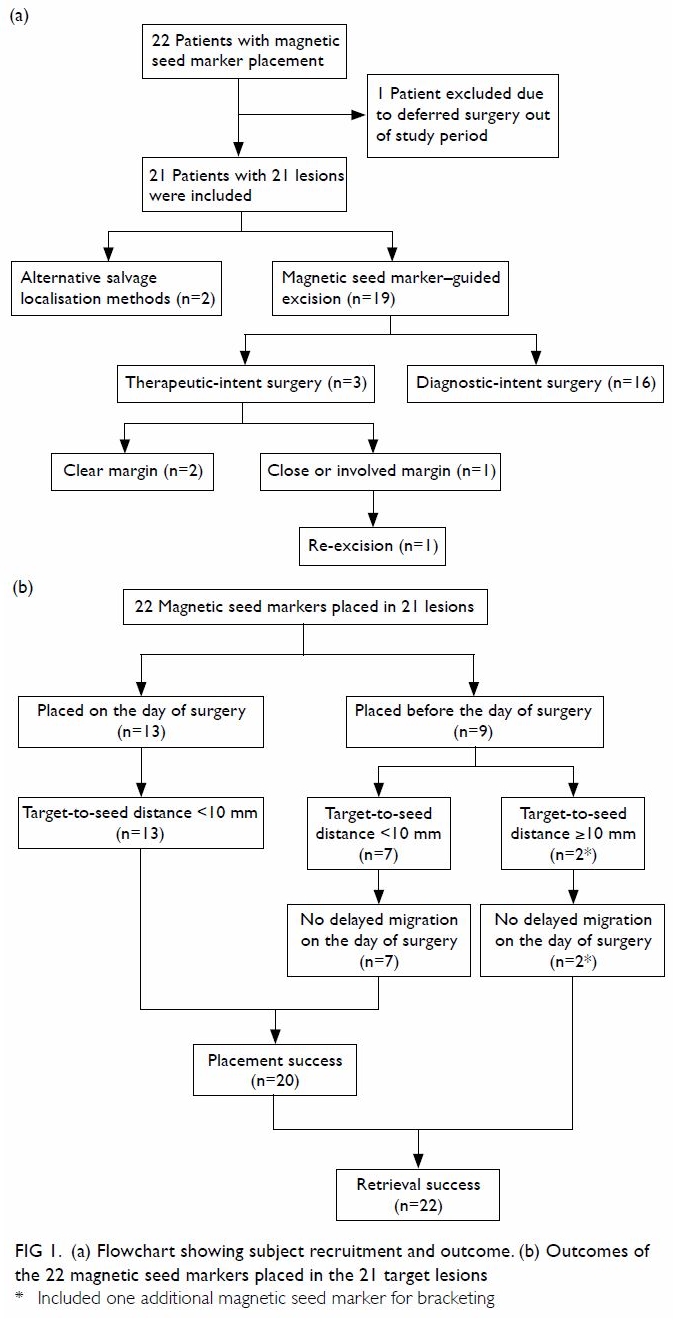
Figure 1. (a) Flowchart showing subject recruitment and outcome. (b) Outcomes of the 22 magnetic seed markers placed in the 21 target lesions
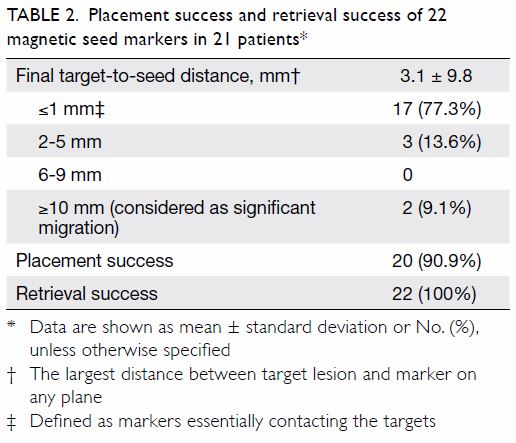
Two magnetic markers (9.1%) migrated >=10 mm
away from their targets. Both had been placed
under stereotactic guidance and migrated along the
direction of breast compression (Fig 2). One of these
magnetic seed markers was aimed for bracketing
initially. No delayed migration was detected in all of
the nine magnetic seed markers placed before the day
of surgery, and there was no further migration of the
two with initial migration. Among the 22 magnetic
seed markers, 17 (77.3%) and three (13.6%) were
≤1 mm and 2 to 5 mm from their target, respectively
(Figs 3 and 4). Therefore, placement success was
achieved in 20 out of 22 magnetic seed markers, with
a success rate of 90.9% (95% CI=72.2%-97.5%). The
mean final target-to-seed distance was 3.1±9.8 mm (Table 2). The final distance between the two
bracketing magnetic seed markers was 29 mm. All 22
magnetic seed markers were able to be localised by
the probe intraoperatively and removed successfully
(100%; 95% CI=85.1%-100%).
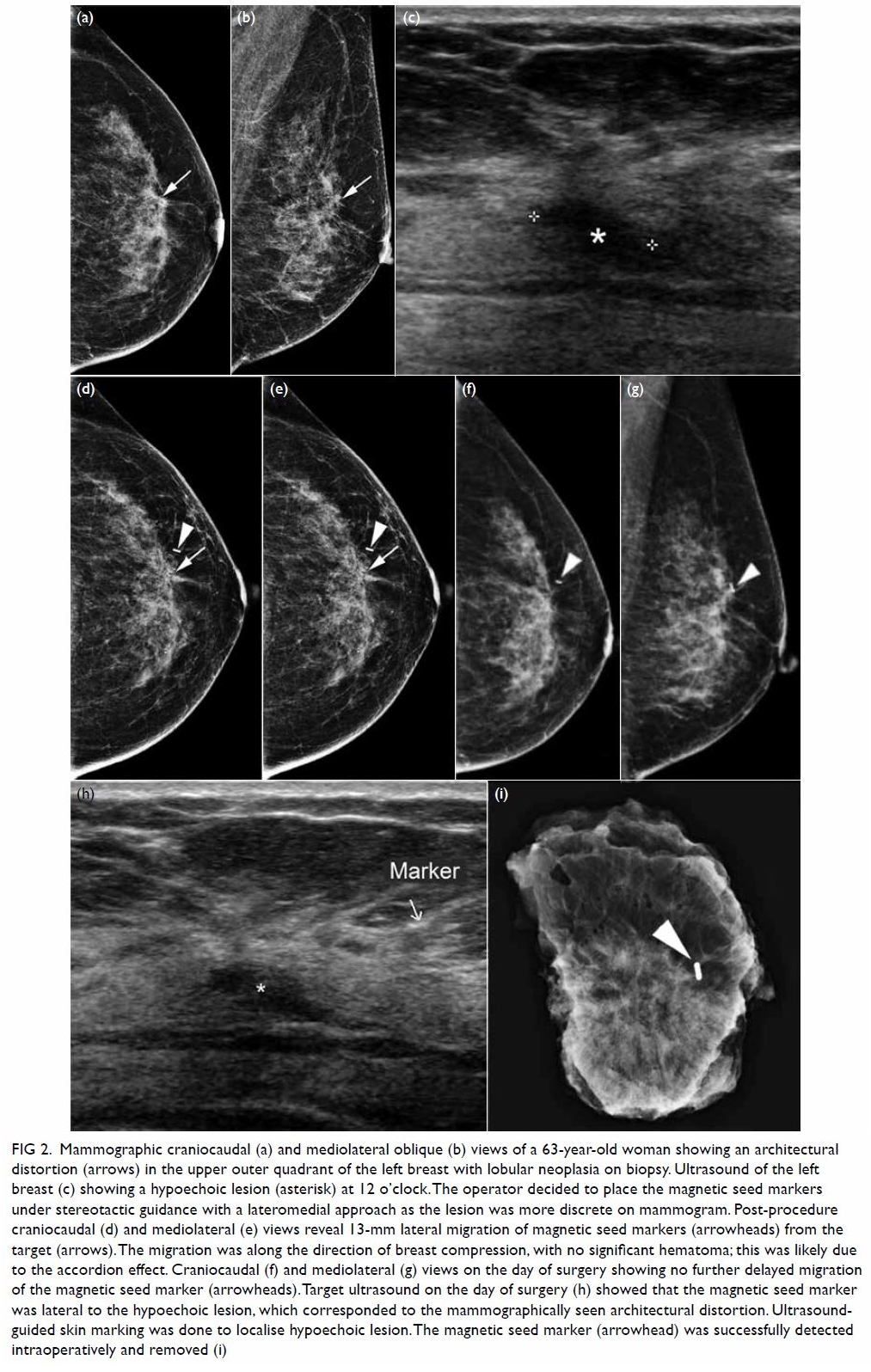
Figure 2. Mammographic craniocaudal (a) and mediolateral oblique (b) views of a 63-year-old woman showing an architectural distortion (arrows) in the upper outer quadrant of the left breast with lobular neoplasia on biopsy. Ultrasound of the left breast (c) showing a hypoechoic lesion (asterisk) at 12 o’clock. The operator decided to place the magnetic seed markers under stereotactic guidance with a lateromedial approach as the lesion was more discrete on mammogram. Post-procedure craniocaudal (d) and mediolateral (e) views reveal 13-mm lateral migration of magnetic seed markers (arrowheads) from the target (arrows). The migration was along the direction of breast compression, with no significant hematoma; this was likely due to the accordion effect. Craniocaudal (f) and mediolateral (g) views on the day of surgery showing no further delayed migration of the magnetic seed marker (arrowheads). Target ultrasound on the day of surgery (h) showed that the magnetic seed marker was lateral to the hypoechoic lesion, which corresponded to the mammographically seen architectural distortion. Ultrasoundguided skin marking was done to localise hypoechoic lesion. The magnetic seed marker (arrowhead) was successfully detected intraoperatively and removed (i)
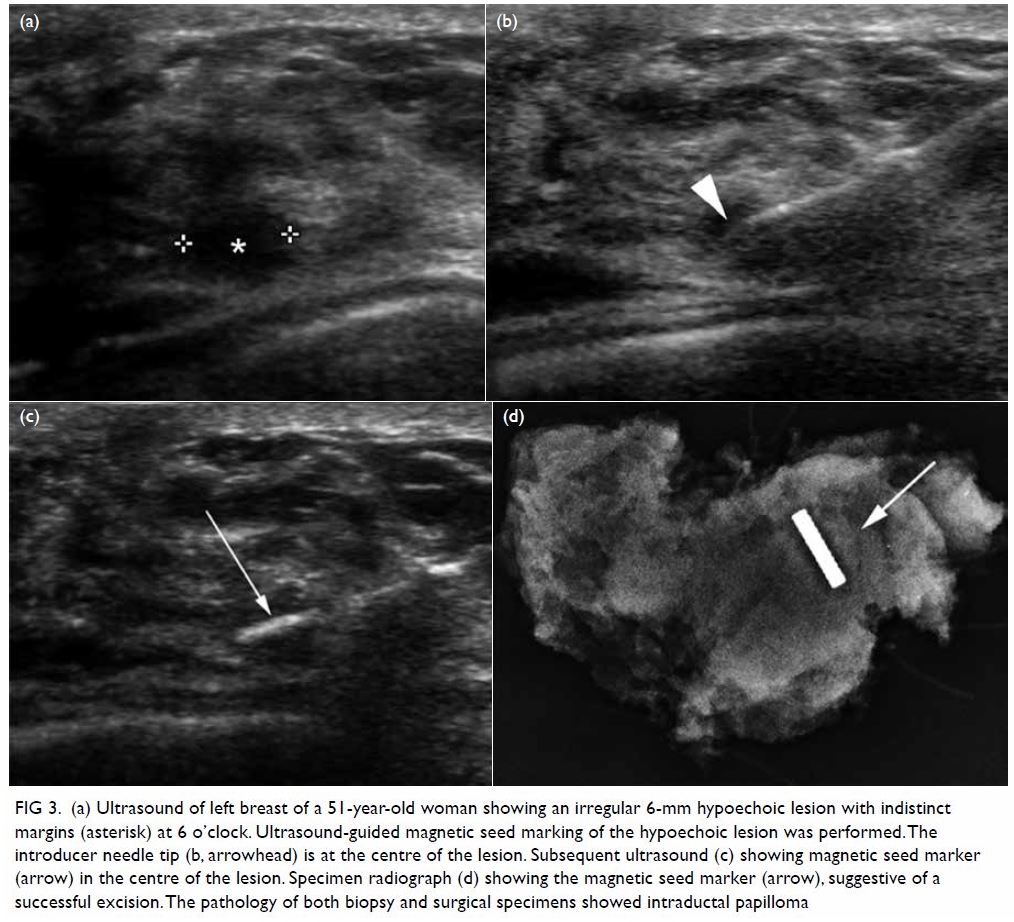
Figure 3. (a) Ultrasound of left breast of a 51-year-old woman showing an irregular 6-mm hypoechoic lesion with indistinct margins (asterisk) at 6 o’clock. Ultrasound-guided magnetic seed marking of the hypoechoic lesion was performed. The introducer needle tip (b, arrowhead) is at the centre of the lesion. Subsequent ultrasound (c) showing magnetic seed marker (arrow) in the centre of the lesion. Specimen radiograph (d) showing the magnetic seed marker (arrow), suggestive of a successful excision. The pathology of both biopsy and surgical specimens showed intraductal papilloma
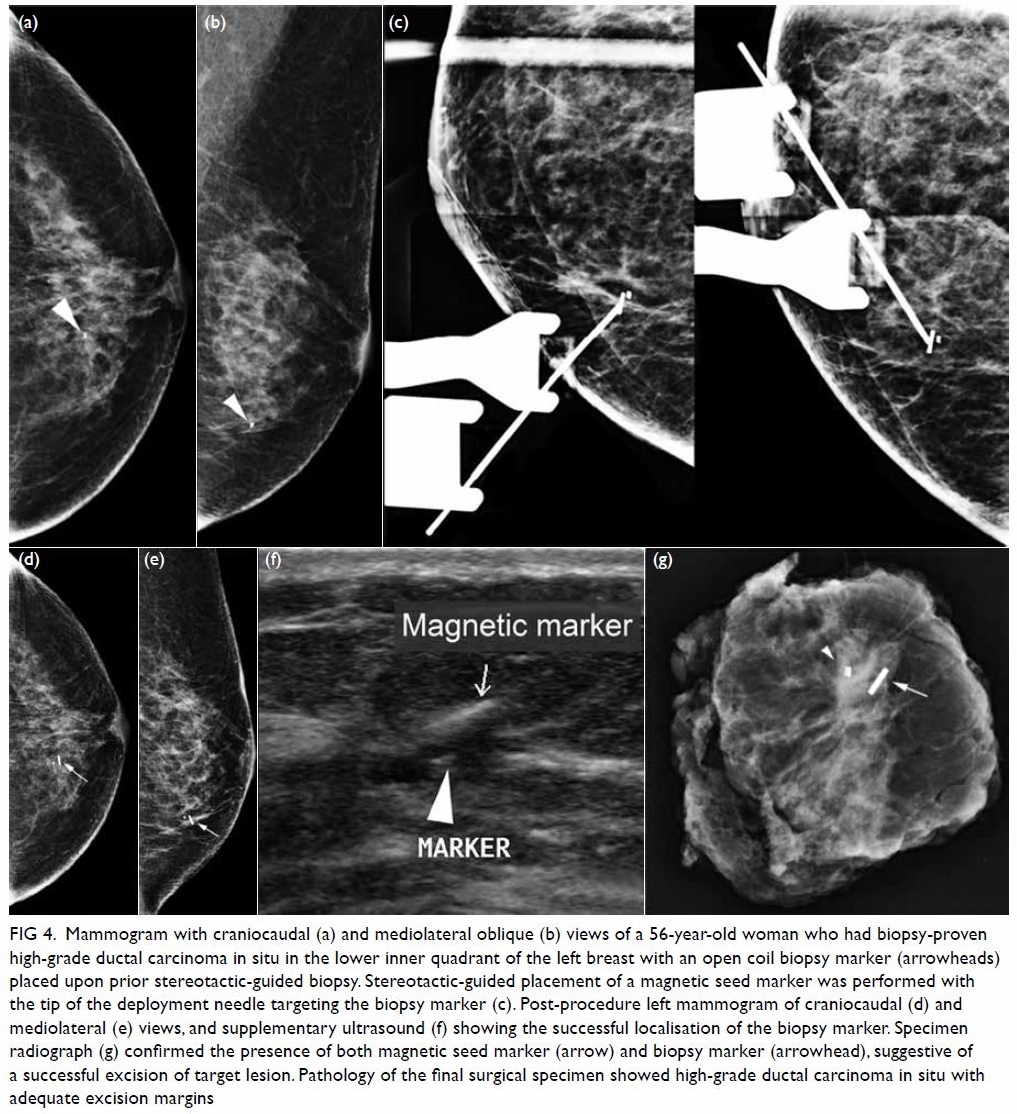
Figure 4. Mammogram with craniocaudal (a) and mediolateral oblique (b) views of a 56-year-old woman who had biopsy-proven high-grade ductal carcinoma in situ in the lower inner quadrant of the left breast with an open coil biopsy marker (arrowheads) placed upon prior stereotactic-guided biopsy. Stereotactic-guided placement of a magnetic seed marker was performed with the tip of the deployment needle targeting the biopsy marker (c). Post-procedure left mammogram of craniocaudal (d) and mediolateral (e) views, and supplementary ultrasound (f) showing the successful localisation of the biopsy marker. Specimen radiograph (g) confirmed the presence of both magnetic seed marker (arrow) and biopsy marker (arrowhead), suggestive of a successful excision of target lesion. Pathology of the final surgical specimen showed high-grade ductal carcinoma in situ with adequate excision margins
Two out of 21 lesions (9.5%) required
alternative localisation performed on the day of
surgery to guide lesion excision due to significant
magnetic seed marker migration of >=10 mm. One
of the lesions was a mammographic architectural
distortion that could be visualised on ultrasound.
The magnetic seed marker had migrated 13 mm
laterally on mammogram. Ultrasound-guided skin
marking was performed on the day of surgery with
the magnetic seed marker detected and removed
together with successful removal of the target lesion
(Fig 2). Another lesion was a wide distribution of
microcalcifications that required two magnetic seed
markers for bracketing under stereotactic guidance.
One of the magnetic seed markers migrated 45 mm
along the direction of breast compression, with no
significant associated haematoma. Salvage hookwire
localisation was performed on the day of surgery. The
target lesion and the non-migrated magnetic seed
marker were first removed by hookwire guidance,
and the migrated magnetic seed marker was then
detected by the probe and removed.
Nineteen lesions (90.5%) had magnetic
seed marker–guided excision as planned, with
sonographic depth of the magnetic seed markers
from skin ranging from 3 to 21 mm with a mean of
10.8±4.8 mm. Among these 19 lesions, 16 (84.2%)
were excised with diagnostic intent and three (15.8%)
were excised with therapeutic intent.
For the 16 lesions excised with diagnostic
intent, preoperative biopsies or fine needle aspiration
had been performed in 14 (87.5%) lesions. Core
needle biopsy of 12 lesions, resulted in two with non-diagnostic
findings, four with benign pathologies
and six with high-risk findings; including four
papillary lesions, one atypical ductal hyperplasia,
and one with scanty atypical ductal cells. Fine needle
aspiration was performed in two lesions, detecting
one fibroadenoma and one papillary lesion. In final
surgical pathology, two of these 16 lesions (12.5%)
had a malignant upgrade from the core biopsy
findings including one low-grade and one high-grade
ductal carcinoma in situ (DCIS).
For the three lesions excised with therapeutic
intent, both preoperative biopsy and final surgical
pathology showed DCIS. The subtype of these lesions
included a high-grade DCIS, a low-grade DCIS, and
an intermediate-grade DCIS with atypical lobular
hyperplasia. One of them had close (0.5 mm) margins
and required re-excision, for a margin clearance rate
of 66.7% and a re-excision rate of 33.3%. There were
no reported complications related to magnetic seed
marker localisation or lesion excision.
Discussion
Successful localisation of breast lesions by magnetic
seed markers was achieved in 19 out of 21 (90.5%)
Chinese patients with a high placement success rate
(90.9%) in our study. The majority of the magnetic
seed markers were accurately placed with a mean
final target-to-seed distance of 3.1 mm. All of the
successfully placed magnetic seed markers were
<5 mm of the target, with 85% of them ≤1 mm. In
all, 100% marker retrieval was achieved without any
reported complications. Such results were similar
to several recent studies which revealed 100%
successful magnetic seed marker retrieval14 17 18 19 20 and
high placement success (96.7%-100%).14 17 18 Our
re-excision rate for therapeutic intent surgery was
found to be 33.3%, which was apparently higher
than that reported in previous studies, ranging from
14.8% to 21.9%.17 18 19 This could be attributable to our
small sample size with only three lesions excised
for therapeutic intent. In fact, a prospective non-randomised
control study by Zacharioudakis et al19 with 100 patients in each arm demonstrated that
the outcome of magnetic seed marker localisation
was comparable to hookwire localisation for breast
conservation surgery in terms of re-excision rate. A
systemic review by Fusco et al21 demonstrated that
the successful localisation and margin clearance
rates were 65% to 100% and 58% to 84%, respectively
for hookwire localisation, and 93% to 100% and 60%
to 100%, respectively for ROLL, while the margin
clearance rates from other previous studies9 10 22
ranged from 57% to 87.4% for hookwire localisation
and 75% to 93.5% for ROLL. All these suggest that
magnetic seed marker is a feasible alternative
localisation method.
Thirteen magnetic seed markers (59.1%)
were placed on the day of surgery during our initial
experience. The purpose was to ensure safety and
to allow radiologists’ and surgeons’ familiarisation
with the new device and workflow. Among all of the
nine magnetic seed markers placed before the day of
surgery (range, 6-56 d), none of them showed delayed migration on the day of surgery. This illustrates
that delayed migration is unlikely to occur and it
may not be necessary for patients to come back to
the Radiology Department on the day of surgery to
confirm magnetic seed marker position prior to the
operation. Similar results were reported by a multi-centre
open-label cohort study on mastectomy
patients, which showed no migration of magnetic
seed markers between placement and surgery,
which were up to 30 days apart.20 This reassures the
feasibility of decoupling of surgery and radiology
appointments, which can potentially reduce
localisation-related delay in surgery. Prolonged
fasting before surgery and the associated increased
risk of vasovagal syncope can therefore be avoided.9 Magnetic seed markers are approved to be placed
up to 30 days prior to surgery in Hong Kong at the
time this article was written. However, successful
retrieval was achieved in one of our patients who
had had her surgery deferred to 56 days after
magnetic seed marker placement due to personal
reasons. This suggests that magnetic seed markers
may be applicable for long-term implantation, which
has already been approved in the United States and
Europe.
Due to limitations of signal transmission,
magnetic seed markers are intended to be placed
at a depth up to 3 cm from skin according to the
manufacturer’s instructions.13 It is challenging to
estimate the true lesion depth as the intraoperative
breast position varies from the position during breast
examinations, particularly when the breast is under
compression during mammographic examinations.
The distance from skin on the image does not
necessarily reflect the shortest distance to the lesion
and can be overestimated. Therefore, for lesions
visible only on mammography, we selected those
near the skin or at middle depth on mammography.
For ultrasound-detected lesions, the sonographic
depth of the lesion from the skin would be measured.
We performed sonographic measurements for
magnetic seed marker depth for all patients as the
sonographic breast position should best resemble
its intraoperative position. In our study, the depth
of magnetic seed marker placement in successfully
localised lesions ranged from 3 to 21 mm with a mean
of 10.8 mm. All magnetic seed markers were able to
be localised by the probe intraoperatively. The depth
limitation of magnetic seed markers is probably not a
major issue in the Chinese population, since Chinese
females tend to have thinner breasts.23 Further study
is warranted to validate this postulation.
Because of potential signal interference, two
magnetic seed markers should not be placed at close
proximity (<2 cm apart) within the breast.14 20 This
can potentially limit its use in bracketing a target or
in localising multiple target lesions in one breast. We
had one case requiring two magnetic seed markers
placed in the same breast for bracketing a group of
microcalcifications. Although one of them showed
significant migration from the initial target, the final
distance between the two magnetic seed markers was
29 mm. Since there could be potential interference
to the probe from hookwires, the target lesion and
the non-migrated magnetic seed marker were first
removed by hookwire guidance, and the migrated
magnetic seed marker was then detected by the probe
and removed. The utility of multiple magnetic seed
markers in one breast should be further evaluated in
future studies with larger sample sizes.
In our study, two magnetic seed markers (9.1%)
were found to have undergone significant migration
of >=10 mm from the target on post-insertion images. Both of them migrated along the direction
of breast compression after the compression was
released, with no significant hematoma detected
radiologically or clinically. We postulate such
migration to be resulting from the accordion effect,
which is a well-known cause for clip migration after
stereotactically guided biopsy. Fatty breasts are
known to be more susceptible to accordion effect–related migration as they are more compressible and
are usually compressed to a greater degree.24 The
migrated biopsy marker can move in the direction of
compression either proximal or distal to the needle
track when the breast expands to its original size and
shape after compression.25 26 27 28 It is best evaluated in
the plane orthogonal to the direction of compression
used.25 Such migration was also recognised in 5.9%
of tomosynthesis-guided magnetic seed marker
localisation procedures by a previous study.17 For
prevention, it is suggested to hold and release the
breast slowly from the compression pad after marker
placement.17 Chinese patients probably have a lower
risk of accordion effect–related migration, as they
tend to have denser breasts.23 However, it could not
be analysed in our study given our small sample size
with only seven magnetic seed markers placed under
stereotactic guidance. Future research with a larger
sample size is needed to evaluate the association
between breast density and seed migration.
There are several other drawbacks of magnetic
seed marker localisation. Cost is a major concern
as it is more expensive compared with hookwire or
ROLL. Extra costs are needed for the initial purchase
of the probes and instruments,17 as specialised non-ferromagnetic
surgical instruments must be used
to avoid magnetic interaction between magnetic
seed marker and sensor. However, minimising
localisation-related delay in surgery may reduce the
operational cost and improve workflow efficiency.
A full cost analysis is necessary in the future. In
addition, magnetic seed markers could not be placed
under magnetic resonance imaging (MRI) guidance
as the deployment needle is made of stainless steel.
Magnetic seed marker insertion is contra-indicated
for patients who have pacemakers or implanted
cardiac devices due to interference of the devices
with the probe.29 Magnetic seed markers are not
officially indicated for use in nickel allergy patients.
Bone wax, which is used as a terminal plug in the
deployment needle, contains beeswax, and may
cause allergic or foreign body reaction.13 Magnetic
seed marker deployment is also not advised in a
patient who may undergo future breast MRI prior to
surgery due to its void artefact of 4 to 6 cm distance,5 9
which influences the MRI diagnostic accuracy.5
There are several limitations to this study. It is a
single-institution retrospective study without direct
comparison to our hookwire localisation or ROLL
cases. Patients were selected for magnetic seed marker localisation in a multidisciplinary meeting
involving breast radiologists and breast surgeons and
this might introduce selection bias. We did not have
any patients with a preoperative diagnosis of invasive
carcinoma in our study, as sentinel node and occult
lesion localisation with a radioisotope still remains
the preferred localisation method for invasive
carcinoma requiring sentinel lymph node biopsy
in our centre. This can be performed in one single
procedure instead of two, thus minimising patients’
discomfort and potential complications from the
procedure. However, magnetic seed markers have
been reported to be a safe and feasible method for
image-guided excision of invasive carcinoma.14 17 18
As discussed before, our small sample size limited
our analyses of migration and margin clearance
rates, and the evaluation of the feasibility of using
multiple seeds in one breast for bracketing a lesion
or for localising multiple lesions. A prospective
randomised trial with larger sample size will
be necessary to fully compare wire localisation
and ROLL to magnetic seed marker localisation.
Patient satisfaction, the reproducibility operator
dependence of magnetic seed marker deployment
and intraoperative localisation, specimen weight,
and cosmetic outcome can also be investigated in
future studies.
Conclusion
The magnetic seed marker system demonstrated
safety and efficacy in Chinese women to localise and
excise non-palpable breast lesions and appears to
overcome many of the limitations of conventional
localisation techniques. It can be an alternative
to hookwires or ROLL in selected patients. Future
research is needed to validate the results.
Author contributions
Concept or design: WY Fung, T Wong, CM Chau, ELM Yu.
Acquisition of data: WY Fung.
Analysis or interpretation of data: WY Fung, T Wong, CM Chau, ELM Yu, JKF Ma.
Drafting of the manuscript: WY Fung, T Wong, CM Chau, ELM Yu.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: WY Fung.
Analysis or interpretation of data: WY Fung, T Wong, CM Chau, ELM Yu, JKF Ma.
Drafting of the manuscript: WY Fung, T Wong, CM Chau, ELM Yu.
Critical revision of the manuscript for important intellectual content: All authors.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
We would like to express our gratitude to our breast team
(Department of Surgery, Princess Margaret Hospital) for
support of our research project.
Funding/support
This research received no specific grant from any funding
agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This study was approved by Kowloon West Cluster Research
Ethics Committee (Ref 146-11). The need for patient consent
was waived by the Research Ethics Committee.
References
1. Lui CY, Lam HS, Chan LK, et al. Opportunistic breast
cancer screening in Hong Kong; a revisit of the Kwong
Wah Hospital experience. Hong Kong Med J 2007;13:106-
13.
2. Lau SS, Cheung PS, Wong TT, Ma MK, Kwan WH.
Comparison of clinical and pathological characteristics
between screen-detected and self-detected breast cancers:
a Hong Kong study. Hong Kong Med J 2016;22:202-9. Crossref
3. Welch HG, Prorok PC, O’Malley AJ, Kramer BS. Breast-cancer
tumor size, overdiagnosis, and mammography
screening effectiveness. N Engl J Med 2016;375:1438-47. Crossref
4. Ramos M, Díez JC, Ramos T, Ruano R, Sancho M,
González-Orús JM. Intraoperative ultrasound in
conservative surgery for non-palpable breast cancer after
neoadjuvant chemotherapy. Int J Surg 2014;12:572-7. Crossref
5. Hayes MK. Update on preoperative breast localization.
Radiol Clin North Am 2017;55:591-603. Crossref
6. Chu TY, Lui CY, Hung WK, Kei SK, Choi CL, Lam HS.
Localisation of occult breast lesion: a comparative analysis
of hookwire and radioguided procedures. Hong Kong Med
J 2010;16:367-72.
7. Dauphine C, Reicher JJ, Reicher MA, Gondusky C,
Khalkhali I, Kim M. A prospective clinical study to evaluate
the safety and performance of wireless localization
of nonpalpable breast lesions using radiofrequency
identification technology. AJR Am J Roentgenol
2015;204:W720-3. Crossref
8. Sharek D, Zuley ML, Zhang JY, Soran A, Ahrendt GM,
Ganott MA. Radioactive seed localization versus wire
localization for lumpectomies: a comparison of outcomes.
AJR Am J Roentgenol 2015;204:872-7. Crossref
9. Kapoor MM, Patel MM, Scoggins ME. The wire and
beyond: recent advances in breast imaging preoperative
needle localization. Radiographics 2019;39:1886-906. Crossref
10. Cheang E, Ha R, Thornton CM, Mango VL. Innovations in image-guided preoperative breast lesion localization. Br J
Radiol 2018;91:20170740. Crossref
11. Ocal K, Dag A, Turkmenoglu O, Gunay EC, Yucel E,
Duce MN. Radioguided occult lesion localization
versus wire-guided localization for non-palpable breast
lesions: randomized controlled trial. Clinics (Sao Paulo)
2011;66:1003-7. Crossref
12. Manca G, Mazzarri S, Rubello D, et al. Radioguided occult
lesion localization: technical procedures and clinical
applications. Clin Nucl Med 2017;42:e498-e503. Crossref
13. Endomag Ltd. Magseed® magnetic marker system:
Instructions for use. 2017. Available from: https://www.
endomag.com/magseed/overview/. Accessed 30 Mar 2020.
14. Price ER, Khoury AL, Esserman LJ, Joe BN, Alvarado MD.
Initial clinical experience with an inducible magnetic seed
system for preoperative breast lesion localization. AJR Am
J Roentgenol 2018;210:913-7. Crossref
15. Wilson EB. Probable inference, the law of succession, and
statistical inference. J Am Stat Assoc 1927;22:209-12. Crossref
16. Sibbering M, Watkins R, Winstanley J, Patnick J, editors.
Quality Assurance Guideline for Surgeons in Breast Cancer
Screening (NHSBSP Publication No. 20). 4th ed. Sheffield: NHS Cancer Screening Programmes; 2009.
17. Lamb LR, Bahl M, Specht MC, D’Alessandro HA,
Lehman CD. Evaluation of a nonradioactive magnetic
marker wireless localization program. AJR Am J Roentgenol
2018;211:940-5. Crossref
18. Thekkinkattil D, Kaushik M, Hoosein MM, et al. A
prospective, single-arm, multicentre clinical evaluation
of a new localisation technique using non-radioactive
Magseeds for surgery of clinically occult breast lesions.
Clin Radiol 2019;74:974.e7-11. Crossref
19. Zacharioudakis K, Down S, Bholah Z, et al. Is the future
magnetic? Magseed localisation for non palpable breast
cancer. A multi-centre non randomised control study. Eur J
Surg Oncol 2019;45:2016-21. Crossref
20. Harvey JR, Lim Y, Murphy J, et al. Safety and feasibility of
breast lesion localization using magnetic seeds (Magseed):
a multi-centre, open-label cohort study. Breast Cancer Res
Treat 2018;169:531-6. Crossref
21. Fusco R, Petrillo A, Catalano O, et al. Procedures for
location of non-palpable breast lesions: a systematic review
for the radiologist. Breast Cancer 2014;21:522-31. Crossref
22. Nadeem R, Chagla LS, Harris O, et al. Occult breast lesions: a comparison between radioguided occult lesion
localisation (ROLL) vs. wire-guided lumpectomy (WGL).
Breast 2005;14:283-9. Crossref
23. Maskarinec G, Meng L, Ursin G. Ethnic differences in mammographic densities. Int J Epidemiol 2001;30:959-65. Crossref
24. Rosen LE, Vo TT. Metallic clip deployment during
stereotactic breast biopsy: Retrospective analysis.
Radiology 2001;218:510-6. Crossref
25. Burbank F, Forcier N. Tissue marking clip for stereotactic
breast biopsy: initial placement accuracy, long-term
stability, and usefulness as a guide for wire localization.
Radiology 1997;205:407-15. Crossref
26. Liberman L, Dershaw DD, Morris EA, Abramson AF,
Thornton CM, Rosen PP. Clip placement after stereotactic
vacuum-assisted breast biopsy. Radiology 1997;205:417-22. Crossref
27. Esserman LE, Cura MA, DaCosta D. Recognizing pitfalls
in early and late migration of clip markers after imaging-guided
directional vacuum-assisted biopsy. Radiographics
2004;24:147-56. Crossref
28. Endomag Ltd. Sentimag®: instructions for use. 2018.
Available from: https://www.endomag.com/sentimag/.
Accessed 30 Mar 2020.