Hong Kong Med J 2022 Feb;28(1):54–63 | Epub 12 Nov 2020
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE (HEALTHCARE IN MAINLAND CHINA)
Epidemiological and clinical characteristics
of patients with COVID-19 from a designated hospital in Hangzhou City: a retrospective observational study
J Gao, MD1; S Zhang, MD2, K Zhou, MD2; X Zhao, MD2; J Liu, 3; Z Pu4
1 Critical Care Department, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, Hangzhou, China
2 Critical Care Department, XiXi Hospital of Hangzhou, Hangzhou, China
3 Department of General Internal Medicine, XiXi Hospital of Hangzhou, Hangzhou, China
4 Research Center of Analysis and Measurement, Zhejiang University of Technology, Hangzhou, China
Corresponding author: Dr S Zhang (zrjzk@zju.edu.cn)
Abstract
Introduction: The outbreak of coronavirus disease
2019 (COVID-19) has exerted a heavy burden on
public health worldwide. We aimed to investigate
the epidemiological and clinical characteristics of
patients with COVID-19 in a designated hospital in
Hangzhou, China.
Methods: This was a retrospective study that
included laboratory-confirmed cases of COVID-19
in XiXi Hospital of Hangzhou from 15 January 2020
to 30 March 2020. We reviewed and analysed the
epidemiological, demographic, clinical, radiological,
and laboratory features involving these cases. Age-tratification
analysis was also implemented.
Results: We analysed 96 confirmed cases. The
patients had a mean age of 43 years, with six patients
younger than 18 years and 14 patients older
than 60 years. No significant gender difference
was discovered. Co-morbidities were commonly
observed in patients aged over 40 years. Twenty eight
of the patients had travelled from Wuhan City, and
51 patients were infected through close contact. Familial clusters accounted for 48 of the cases. The
mean incubation time was 7 days, and the symptoms
were mainly fever, cough, fatigue, and sore throat.
Lymphocytopenia was observed predominantly
in patients aged over 60 years. Fifty five patients
presented with bilateral pulmonary lesions. The radiological changes were typically distributed in the
subpleural area, and pleural effusion rarely occurred.
All patients were discharged successfully.
Conclusion: During the early stage of the COVID-19
outbreak, half of the patients from a designated
hospital in Hangzhou City were discovered as familial clusters. Therefore, strict prevention and
control measures during self-isolation should be
implemented. Patients aged over 60 years who
had underlying co-morbidities were prone to
lymphocytopenia and severe infection.
New knowledge added by this study
- Half of the patients with coronavirus disease 2019 (COVID-19) from a designated hospital in Hangzhou City (outside of Hubei Province) during the early stage of COVID-19 outbreak were discovered as familial clusters.
- The patients with COVID-19 who were aged >60 years and had underlying co-morbidities were prone to lymphocytopenia and severe infection.
- All patients with COVID-19 in our centre successfully recovered and were eventually discharged.
- Strict prevention and control measures should be implemented to prevent intrafamilial dissemination of severe acute respiratory syndrome coronavirus 2 during self-isolation and home quarantine, a meaningful insight for policy makers.
- Patients aged >60 years with COVID-19 should be cared for and treated more carefully.
- In general, patients with COVID-19 can recover well when diagnosed and treated early and properly, if overcrowding of medical resources is avoided.
Introduction
The rapid spread of coronavirus disease 2019
(COVID-19) has become a focus of public health
concern since November 2019. According to the World Health Organization report with data updated on 6 November 2020, the COVID-19 pandemic has
caused over 48.5 million confirmed cases and over
1.23 million deaths worldwide.1 The 2019 novel coronavirus has been designated as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)
by the Coronavirus Study Group of the International
Committee on Taxonomy of Viruses. The Law on
Prevention and Control of Infectious Diseases, China
categorises COVID-19 as a Category B infectious
disease, but it is supervised as Category A in China.
During the early stage of the COVID-19
outbreak, especially before the lockdowns of Wuhan
City and then Hubei Province, some people who
had been infected by the virus travelled back to
Hangzhou from Wuhan. Then the disease was
disseminated by person-to-person transmission
within the Hangzhou community. A familial cluster
of the disease occurred during the self-isolation and
home quarantine period because of intrafamilial
transmission. The XiXi Hospital of Hangzhou was
immediately designated by the government as the
only municipal hospital for diagnosis and therapy
of patients with COVID-19 in Hangzhou City. We
reviewed and analysed the hospital’s medical records
to determine the epidemiological and clinical
characteristics of these cases.
Methods
Participants and setting
This retrospective observational study was
performed on the records of patients who were
treated from 15 January 2020 to 30 March 2020 at
the XiXi Hospital of Hangzhou. The study adhered to
the ethical principles of medical research involving human subjects of the World Medical Association
Declaration of Helsinki and was approved by the
Ethics Committee of the XiXi Hospital of Hangzhou.
Informed consent was waived because of the
retrospective nature of this study.
Instruments and testing
The following instruments and materials were used
in the study: a blood gas analyser (Radiometer
ABL90, Denmark), an automatic haematology
analyser (SYSMEX XE-5000, Japan), an automatic
coagulation analyser (SYSMEX CS5100, Japan), an
automatic biochemistry analyser (Beckman Coulter
AU5831, US), and a vacuum blood collection
tube (BD Vacutainer containing lithium heparin
anticoagulant, US). Body surface temperature was
detected by a non-contact infrared thermometer
(JXB-178, Berrcom, Guangzhou). A fever was defined
as a body temperature >37.0°C. Chest computed
tomography (CT) scans (GE Revolution EVO, US)
were conducted on every patient. Standard nucleic
acid detection for SARS-CoV-2 was conducted at
the Hangzhou Municipal Center for Disease Control
and Prevention by the way of qualitative polymerase
chain reaction (PCR). The diagnostic criteria were
based on the recommendation of the National
Institute for Viral Disease Control and Prevention,
China (http://ivdc.chinacdc.cn/kyjz/202001/
t20200121_211337.html).
Data collection
Epidemiological and demographic information
about patients with COVID-19 was collected and
reviewed, including age, gender, height, weight,
co-morbidities like hypertension and type 2 diabetes
mellitus, history of smoking, drinking and surgery,
and recent travel and residence history. The clinical
features and symptoms were recorded and reviewed
during hospital visits. The results of the first
laboratory tests performed on hospital admission
were analysed. During hospitalisation, clinical and
laboratory characteristics including SARS-CoV-2
nucleic acid test results were evaluated. Radiological
manifestations on chest CT scan were examined.
The outcomes of treatment were checked, and the
patients received follow-up.
Two attending doctors were responsible for
the diagnosis and treatment of all patients with
COVID-19 according to the clinical diagnosis
guideline and treatment protocol for COVID-19
released by the National Health Commission &
National Administration of Traditional Chinese
Medicine, China and the Zhongnan Hospital of
Wuhan University Novel Coronavirus Management
and Research Team.2 3 The radiological diagnosis
of chest CT scans was decided by two attending
radiologists and another two attending clinical
doctors independently.
Severity classification
The laboratory-confirmed cases were classified
according to severity as mild (ie, mild symptoms
without pneumonia), moderate (ie, respiratory
symptoms and fever with pneumonia), severe (ie,
respiratory distress, respiratory frequency ≥30/min,
blood oxygen saturation ≤93%, ratio of partial
pressure of arterial oxygen to fraction of inspired
oxygen <300 mm Hg, and/or lung infiltration >50%
within 24-48 hours), and critical (ie, respiratory
failure, shock, and/or multiple organ dysfunction or
failure).
Discharge criteria
The discharge criteria were normalisation of
body temperature for more than 3 days, obvious
improvement of respiratory symptoms, pulmonary
imaging showing distinct inflammation absorption,
and two consecutive negative nucleic acid tests
on respiratory tract samples such as sputum or
nasopharyngeal swab (with a sampling interval of at
least 24 hours). Patients with COVID-19 who met
the above criteria could be discharged.
Statistical analysis
We used SPSS (Windows version 19.0; IBM Corp, Armonk [NY], US) for all statistical analyses. One-way
analysis of variance was performed to compare
continuous, normally distributed numeric variables,
which were presented as means and 95% confidence
intervals. The Mann-Whitney U non-parametric
test was used to compare continuous numeric
variables with skewed distributions, which were
shown as medians and 95% confidence intervals. The
Pearson χ2 test was employed to compare categorical
variables, which were presented as frequencies and
proportions (percentages). A stratified analysis
by age was also conducted. Comparative analysis
between early and late discharge was implemented
to explore potentially associated factors. A P value
of <0.05 was considered to be statistically significant.
Results
Epidemiological, demographic, and general
clinical characteristics
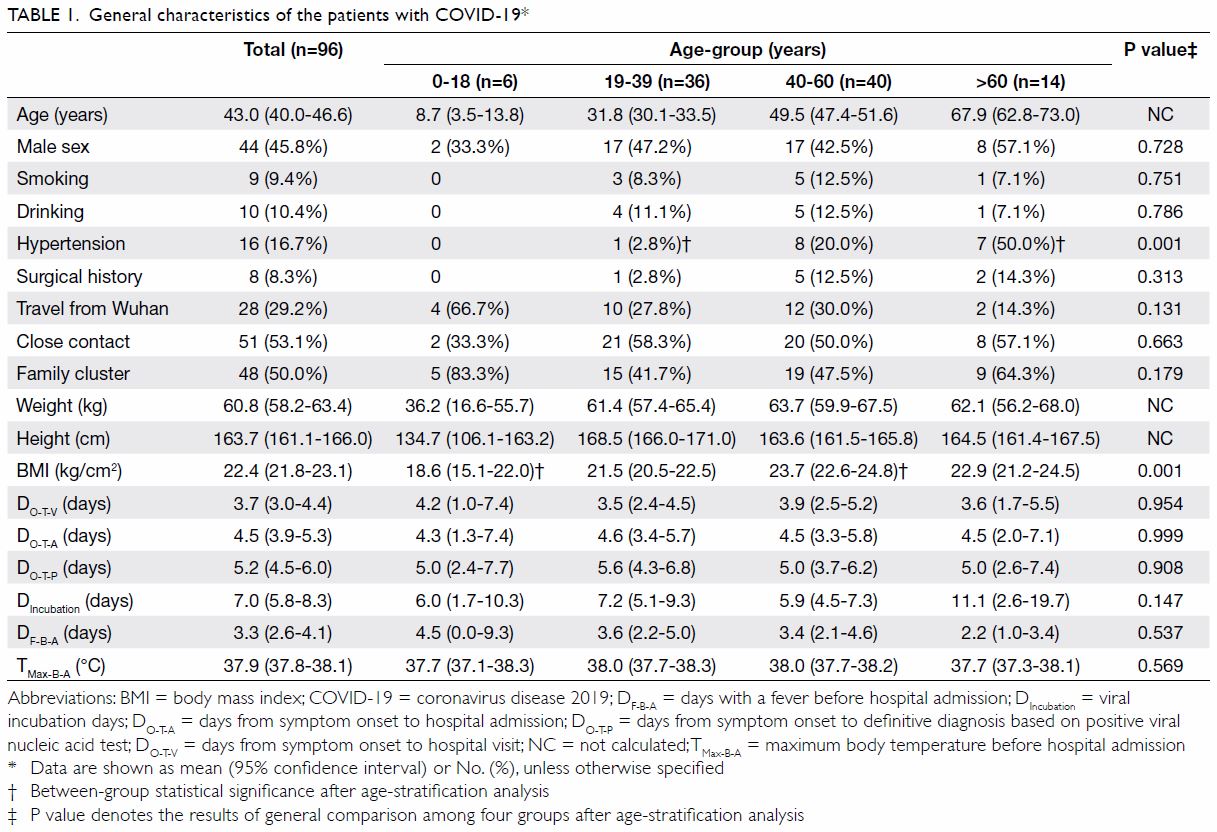
Among these 96 patients with COVID-19, six were
aged 0 to 18 years and 14 were aged >60 years
(Table 1). Most (79.2%) patients were aged between
19 and 60 years. No significant sex difference was
discovered. All patients had basically normal body
mass index values. Half of patients aged >60 years
had a history of hypertension. Eight adult patients had a surgical history involving pituitary tumour,
pulmonary abscess, coronary artery bypass grafting
because of coronary heart disease, gallbladder stone,
ovarian cyst, Caesarean section, or splenectomy
because of trauma. Other co-morbidities were
exclusively observed in patients aged >40 years,
including type 2 diabetes mellitus, fatty liver,
hepatitis B, liver cirrhosis, and bronchiectasis. A
history of smoking or drinking was reported by nine
(9.4%) and 10 (10.4%) patients, respectively.
Among 96 patients with confirmed infection,
28 (29.2%) had travelled from Wuhan City, and
51 cases were acquired via close contact. However,
a few patients had no definitive contact history,
even after rigorous tracing. Familial clusters of
the disease accounted for 48 of this study’s cases,
and 11 patients who had travelled from Wuhan
City presented in familial clusters. In most familial
clusters, two members were attacked, however,
six family members were also found to be infected in
two separate familial clusters.
The mean time from symptom onset to the first
visit was 3.7 days, and the time to hospital admission
was 4.5 days. The period from symptom onset to
definitive diagnosis based on positive viral nucleic
acid test was 5.2 days. The mean incubation time was
7.0 days. The mean time with fever before admission was 3.3 days, and the maximum body temperature before admission was 37.9°C.
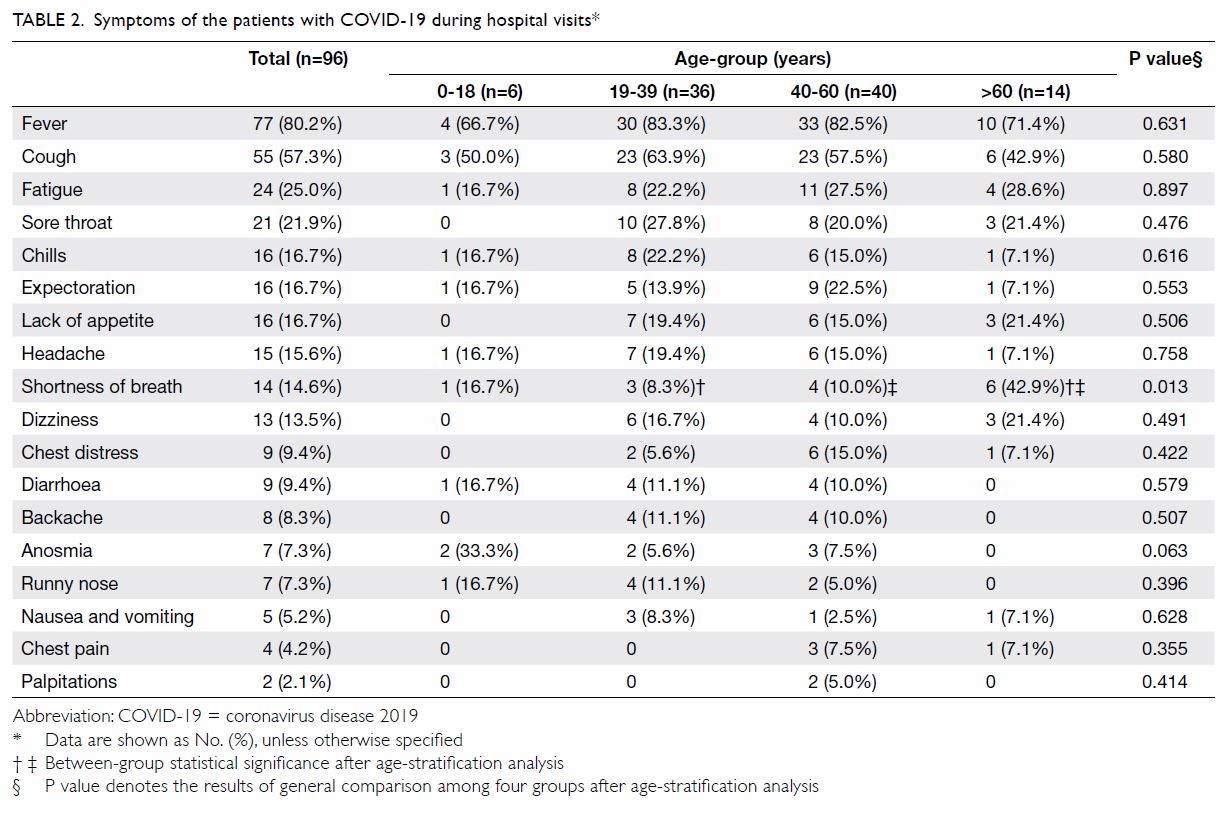
Symptoms recorded during hospital visits
The laboratory-confirmed patients’ main symptoms
were fever, cough, fatigue, sore throat, chills,
expectoration, shortness of breath, headache,
dizziness, decreased appetite, diarrhoea, nausea,
and vomiting (Table 2). These symptoms essentially
involved the respiratory system, in addition to
the alimentary and central nervous systems. The
symptoms were basically similar across different
age-groups, except that shortness of breath occurred
more commonly among patients aged >60 years.
First test results on hospital admission
As presented in Table 3, the mean white blood cell
count was not elevated. Besides white blood cells, the
levels of haemoglobin, eosinophil, and platelets were
basically within normal ranges. Lymphocytopenia
was observed predominantly in patients aged
>60 years. The concentrations of blood electrolytes,
glucose, lactate, triglycerides, and free fatty acids
were largely normal. Injury to the liver, kidney,
heart, and coagulation systems were not observed.
Further, hypoxaemia was not found in most cases on hospital admission, except for several patients aged
>60 years. The overall ratio of the partial pressure of
arterial oxygen to the fraction of inspired oxygen was about 340 mm Hg. Inflammatory biomarkers are
an acute-phase response to the virus insult and are
therefore involved in the development of the disease. Generally, the level of blood C-reactive protein was
slightly elevated on admission (16.2 mg/L), and
that of patients aged >60 years was relatively higher
(31.6 mg/L). Serum amyloid A concentration
increased in almost all cases (61.7 mg/L), especially
for patients aged >60 years (88.1 mg/L). The
procalcitonin level did not increase across all cases
on admission.
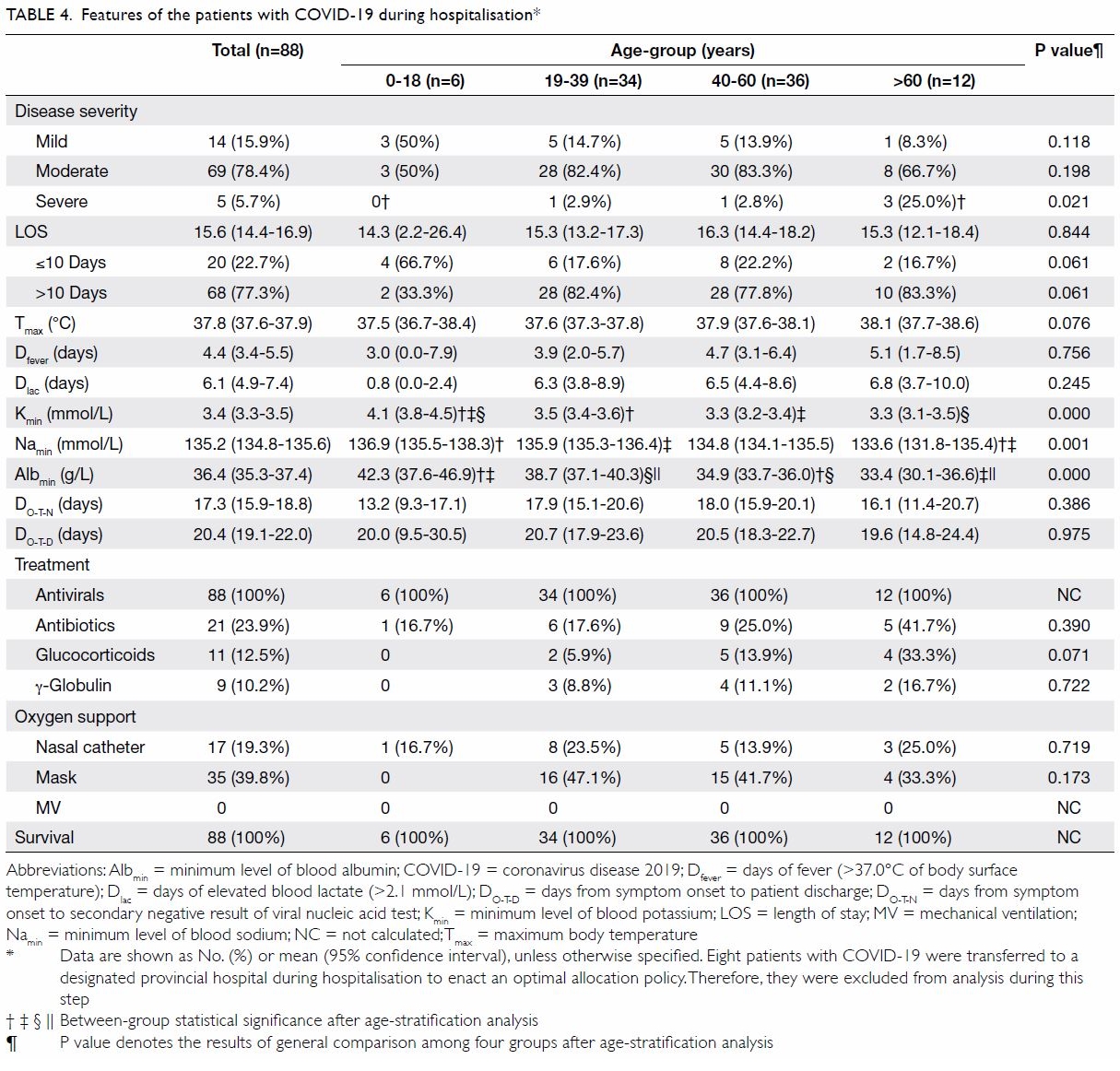
Features during hospitalisation
During hospitalisation, eight patients with COVID-19 were transferred to a designated provincial hospital
in Hangzhou to enact an optimal allocation policy.
Therefore, we analysed the clinical and laboratory features of 88 cases during hospitalisation (Table 4).
The severity of disease was mild or moderate in
83 patients (around 94%). Among 12 patients aged
>60 years, three (25%) had severe disease. The mean
length of stay across all cases was 15.6 days. The
mean time with fever during hospitalisation was
4.4 days. The mean maximum body temperature
was 37.8°C. Hypokalaemia, hyponatraemia, and
hypoalbuminaemia were more likely to develop in
patients aged >60 years. The time from symptom
onset to secondary negative result of a viral nucleic
acid test was about 17 days, and the mean time to
patient discharge was about 20 days.
Most cases (59.1%) were supported through nasal catheter or mask oxygen. No one was assisted
by non-invasive or invasive mechanical ventilation.
All patients were treated with one or two kinds of
antivirals, ie, α-interferon, lopinavir/ritonavir, or
abidor. Antibiotics like levofloxacin and moxifloxacin
were prescribed when bacterial infection was
suspected. Adjuvant therapy with glucocorticoids
(methylprednisolone, 40-80 mg/d) or γ-globulin was
implemented only in a small percentage of cases
(around 10%) and exclusively in adult patients. All
patients successfully recovered and were discharged.
No one progressed to the critically ill state, and the
absence of recurrence in all cases was confirmed by
follow-up until 20 June 2020.
Radiological manifestations during
hospitalisation
Radiological pulmonary imaging was evaluated
during hospitalisation of the patients with moderate
and severe disease (74 cases) [Table 5 and Fig]. A
total of 19 (25.7%) and 55 (74.3%) patients presented
with unilateral and bilateral pulmonary lesions, respectively. Ground-glass opacities in the lungs
were discovered on chest CT scan in approximately
50% of cases. Radiological pulmonary changes were
mostly distributed in the subpleural area (around
80%), and pleural effusion rarely occurred in any
age-stratified group. The mean time from symptom
onset to the worst CT imaging finding was 9 days, and
the mean time to the start of pulmonary infiltration
absorption on CT imaging was about 12 days.
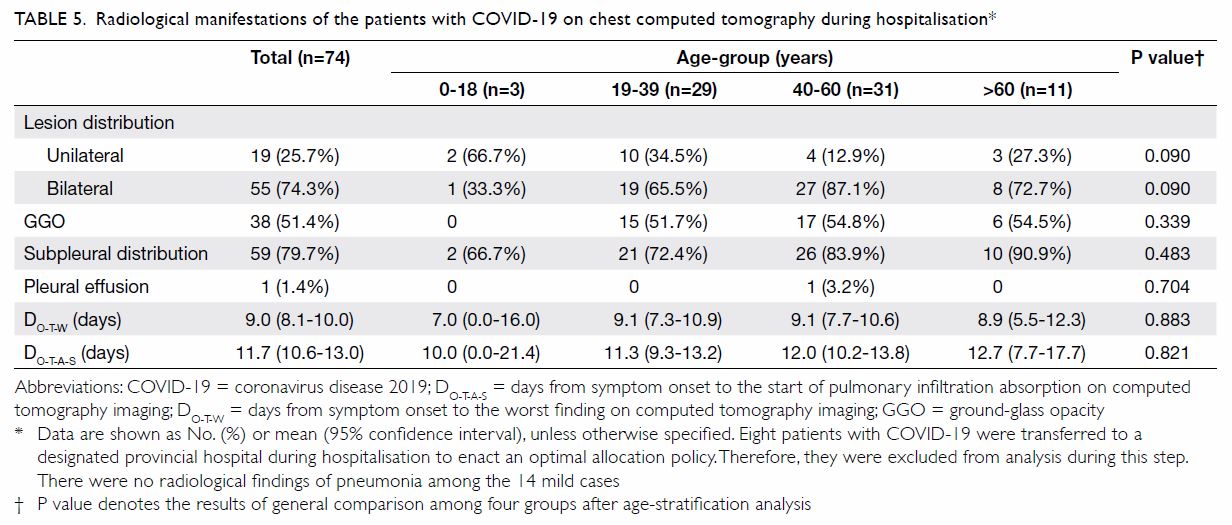
Table 5. Radiological manifestations of the patients with COVID-19 on chest computed tomography during hospitalisation
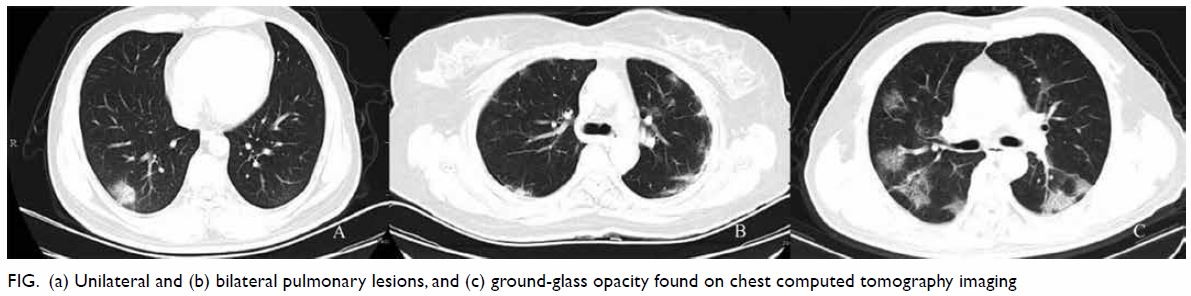
Figure. (a) Unilateral and (b) bilateral pulmonary lesions, and (c) ground-glass opacity found on chest computed tomography imaging
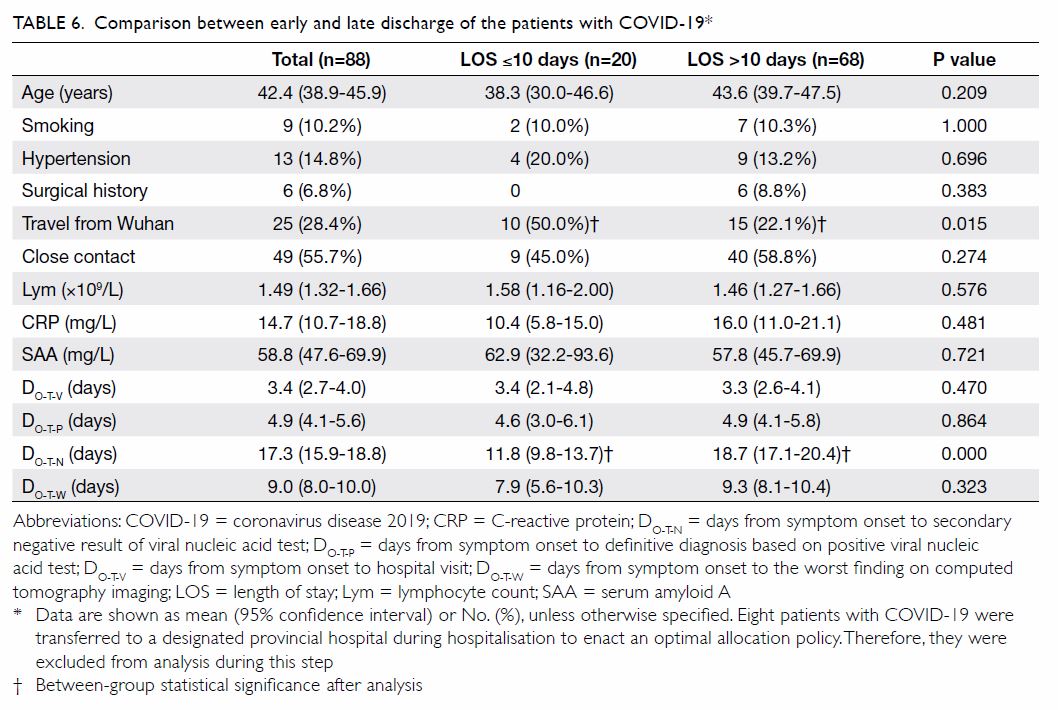
Potential factors associated with early
discharge
We explored the factors that could potentially be
associated with early discharge of patients with
COVID-19 (Table 6). Early discharge was defined
as a hospital length of stay (LOS) of ≤10 days. A
comparison was conducted between early (LOS
≤10 days) and late (LOS >10 days) discharge of
patients with COVID-19. Of the investigated
patients, 20 cases were discharged early, whereas
68 cases underwent late discharge. We compared
13 factors between the two groups. Two factors were significantly associated with early discharge: more
patients in the early discharge group compared
with the late discharge group had travelled from
Wuhan City (50.0% vs 22.1%). Further, the time
from symptom onset to secondary negative result
of a viral nucleic acid test was shorter in the early
discharge group than the late discharge group
(11.8 days vs 18.7 days).
Discussion
The emergence and spread of COVID-19 has
caused a new public health crisis to threaten the
world. Patient zero of the disease is still unknown,
although many of the initial cases in Wuhan City had
exposure to the Huanan Seafood Wholesale Market
in common.4 5 A probable bat origin of SARS-CoV-2
has been considered.6 Angiotensin-converting
enzyme II has been reported to be the entry receptor
on epithelial and endothelial cells within the lung,
heart, kidney, and intestine.6 7 As a highly contagious
disease, COVID-19 is transmitted by inhalation or
contact with infected droplets. On 23 January 2020,
Wuhan City, as the epicentre of COVID-19 in China,
was locked down to prevent the disease’s spread.
Before the lockdown, some infected people left
Wuhan City for other cities outside Hubei Province.
Then, extensive person-to-person transmission
occurred.8 9 Thanks to healthcare service providers,
all hospitalised patients with COVID-19 in our research survived, recovered successfully, and then
were eventually discharged. The findings of our
observational study can provide help with decision
making about public health policy involving
COVID-19 prevention and therapy.
This retrospective study reports the
epidemiological, demographic, clinical, laboratory,
and radiological findings of patients with COVID-19
who were treated at a designated hospital in
Hangzhou City. A comparative analysis according
to age stratification was implemented. Deterioration
was more probable in patients aged over 60 years
with underlying co-morbidities. The finding is
consistent with those of another previous report.10
Deterioration could be associated with the ageing
and dysfunction of organs, especially reduced
immune function as lymphocytopenia. Severe acute
respiratory syndrome coronavirus 2 can consume
lymphocytes, which is probably an important
cause of the proliferation and spread of the virus.
Although we did not detect the plasma levels of
pro-inflammatory mediators like tumour necrosis
factor and interleukin, the cytokine storm has been
previously reported to be associated with COVID-19
severity.11
Respiratory symptoms like fever, cough, sore
throat, and shortness of breath were commonly the
first presentations during hospital visits among the
patients in the present study. The disease should be
differentiated from influenza and common cold-causing rhinovirus or parainfluenza virus infections.
In the early stage of the pandemic, a policy of selfisolation
and home quarantine was implemented.
However, because of the high contagiousness of
SARS-CoV-2, 50% (48 of 96) of the cases in our
study appeared as familial clusters. Prior studies
also reported the discoveries of case clusters within
familial households.12 13 14 The basic reproductive
number (R0) has been revealed to be as high as 2.2 or
even 5.7.15 16 Therefore, strict control measures should
be implemented to avoid intrafamilial dissemination
during self-isolation and home quarantine.
The disease has very strong infectivity by
human-to-human transmission, even during the
incubation period. Based on the gradually increasing
understanding of the disease’s characteristics, the
policy for personnel travelling from the epidemic area
to Hangzhou City was changed from self-isolation
and home quarantine to centralised compulsory
isolation on 21 March 2020. Consequently, person-to-person transmission was effectively controlled.
Therefore, strict quarantine has been confirmed to
be the only effective intervention to decrease the
contagion rate.
Early negative turning of the viral nucleic acid
test was associated with early discharge of patients
with COVID-19 in this study. This may imply
early recovery of injured organs. A relatively high
proportion of patients who travelled from Wuhan
City were discharged early. Thus, SARS-CoV-2 could
have mutated and evolved. More research is needed
to clarify that whether its virulence has increased
or decreased after its propagation through
generations.
In this study, five (5.7%) patients had the severe
disease type, but no patients died. In a summary
report from Chinese Center for Disease Control and
Prevention with data updated through 11 February
2020, 14% of 44 415 confirmed cases were classified
as severe, and 5% were critical.13 The overall case-fatality
rate was 2.3% (1023 of 44 672 confirmed
cases). In Italy, the corresponding rate was reported
to be 7.2% (1625 deaths of 22 512 cases) based on
data through 17 March 2020.17 The case-fatality
rate of COVID-19 is much lower than those of the
prior SARS and Middle East Respiratory Syndrome,
which were 9.6% and 34.4%, respectively.13 However,
because of the shortage of PCR test kits and the
existence of false-negative PCR results, the actual
number of cases in the population is unknown.
Serological tests, when available, could be adopted
widely in the future for COVID-19 diagnosis.
Although the quantity of cases in this study is limited,
overall recovery from the disease will proceed well
when diagnosis and treatment are conducted early
and properly, if overcrowding of medical resources
is avoided.
Bilateral distribution of patchy shadows and ground-glass opacities in the subpleural area were
the most frequently discovered radiological findings
in the present study, and these are typical hallmarks
of radiological pulmonary imaging in COVID-19.18
Although multiple organs (eg, those of the
respiratory, alimentary, genitourinary, and central
nervous systems) can interact with SARS-CoV-2
owing to viraemia and the cytokine storm, the lungs
are still the principal target of the virus. Generally,
the pulmonary presentation is consistent with the
clinical severity of COVID-19. Because there were
no critical cases in our study, more severe chest
imaging findings were not present (eg, entire lungs
involved in exudation and consolidation). Certain
critical patients in intensive care units with severe
acute respiratory distress syndrome even need
extracorporeal membrane oxygenation support.19 In
epidemic areas, chest CT could also be adopted as an
early supplementary diagnostic tool.20
So far, there is no specifically proven antiviral
treatment for COVID-19. The mainstay of therapy
is optimised supportive care, including proper
oxygen supply. The efficacy of antiviral drugs,
including lopinavir/ritonavir, is still unknown.21
The pharmacotherapies used in the present study,
including antiviral and immunomodulating
treatments, are only empirical and palliative. Further
randomised clinical trials are urgently needed
to determine the most effective evidence-based
treatments.
The current study has several limitations. First,
this is a retrospective study with data from a single
centre. The number of included cases is relatively
small. However, it is meaningful for the evaluation
of characteristics of early cases outside of Wuhan
City, especially for policy makers. Second, no
potentially effective antiviral drugs can be proposed
by the present study. Further basic and clinical
research is required to elucidate effective and safe
pharmacotherapies, as to date, no proven antiviral
drugs are available. Third, asymptomatic infection
of COVID-19 is currently an important issue. We
do not have enough data to provide associated
information. More studies are needed to provide
diagnosis and differentiation of asymptomatic cases,
particularly involving the serological and nucleic
acid tests that have recently become available to the
general population.
Conclusion
During the early stage of the COVID-19 outbreak,
half of the patients from a designated hospital in
Hangzhou City were discovered as familial clusters.
Therefore, strict prevention and control measures
should be implemented during self-isolation. Patients
aged >60 years with underlying co-morbidities were
prone to lymphocytopenia and severe infection.
Author contributions
Concept or design: J Gao, S Zhang.
Acquisition of data: K Zhou, X Zhao, J Liu.
Analysis or interpretation of data: J Gao, Z Pu.
Drafting of the manuscript: J Gao, Z Pu.
Critical revision of the manuscript for important intellectual content: S Zhang, K Zhou, X Zhao, J Liu.
Acquisition of data: K Zhou, X Zhao, J Liu.
Analysis or interpretation of data: J Gao, Z Pu.
Drafting of the manuscript: J Gao, Z Pu.
Critical revision of the manuscript for important intellectual content: S Zhang, K Zhou, X Zhao, J Liu.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
All authors thank all of the patients with COVID-19 and
healthcare service providers at XiXi Hospital of Hangzhou,
China.
Funding/support
This research was supported by the Innovative Talents
Supportive Project from Medical Health Science and
Technology Programme of Zhejiang Provincial Health
Commission, China (Ref 2020RC072). The funder had no role
in study design, data collection/analysis/interpretation, or
manuscript preparation.
Ethics approval
The study was approved by the Ethics Committee of the XiXi Hospital of Hangzhou, China (Ref 2020-31). The requirement
for informed consent was waived because of the retrospective
nature of this study.
References
1. World Health Organization. Coronavirus disease
(COVID-2019) situation report. 6 Nov 2020. Available
from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/. Accessed 8 Nov 2020.
2. Zhao JY, Yan JY, Qu JM. Interpretations of “diagnosis and
treatment protocol for novel coronavirus pneumonia (Trial
Version 7)”. Chin Med J (Engl) 2020;133:1347-9. Crossref
3. Jin YH, Cai L, Cheng ZS, et al. A rapid advice guideline
for the diagnosis and treatment of 2019 novel coronavirus
(2019-nCoV) infected pneumonia (standard version). Mil
Med Res 2020;7:4. Crossref
4. Forster P, Forster L, Renfrew C, Forster M. Phylogenetic
network analysis of SARS-CoV-2 genomes. Proc Natl Acad
Sci USA 2020;117:9241-3. Crossref
5. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from
patients with pneumonia in China, 2019. N Engl J Med
2020;382:727-33. Crossref
6. Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin.
Nature 2020;579:270-3. Crossref
7. Yan R, Zhang Y, Li Y, Xia L, Guo Y, Zhou Q. Structural basis
for the recognition of SARS-CoV-2 by full-length human
ACE2. Science 2020;367:1444-8. Crossref
8. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics
of coronavirus disease 2019 in China. N Engl J Med
2020;382:1708-20. Crossref
9. Li X, Zai J, Wang X, Li Y. Potential of large “first generation”
human-to-human transmission of 2019-nCoV. J Med Virol
2020;92:448-54. Crossref
10. Chen N, Zhou M, Dong X, et al. Epidemiological and
clinical characteristics of 99 cases of 2019 novel coronavirus
pneumonia in Wuhan, China: a descriptive study. Lancet
2020;395:507-13. Crossref
11. Huang C, Wang Y, Li X, et al. Clinical features of patients
infected with 2019 novel coronavirus in Wuhan, China.
Lancet 2020;395:497-506. Crossref
12. Chan JF, Yuan S, Kok KH, et al. A familial cluster of
pneumonia associated with the 2019 novel coronavirus
indicating person-to-person transmission: a study of a
family cluster. Lancet 2020;395:514-23. Crossref
13. Wu Z, McGoogan JM. Characteristics of and important
lessons from the coronavirus disease 2019 (COVID-19)
outbreak in China: summary of a report of 72 314 cases
from the Chinese Center for Disease Control and
Prevention. JAMA 2020;323:1239-42. Crossref
14. Yu P, Zhu J, Zhang Z, Han Y. A familial cluster of infection
associated with the 2019 novel coronavirus indicating
possible person-to-person transmission during the
incubation period. J Infect Dis 2020;221:1757-61. Crossref
15. Li Q, Guan X, Wu P, et al. Early transmission dynamics in
Wuhan, China, of novel coronavirus-infected pneumonia.
N Engl J Med 2020;382:1199-207. Crossref
16. Sanche S, Lin YT, Xu C, Romero-Severson E, Hengartner N,
Ke R. High contagiousness and rapid spread of severe
acute respiratory syndrome coronavirus 2. Emerg Infect
Dis 2020;26:1470-7. Crossref
17. Onder G, Rezzz G, Brusaferro S. Case-fatality rate and
characteristics of patients dying in relation to COVID-19
in Italy. JAMA 2020;323:1775-6. Crossref
18. Cao Y, Liu X, Xiong L, Cai K. Imaging and clinical features
of patients with 2019 novel coronavirus SARS-CoV-2: a
systematic review and meta-analysis. J Med Virol 2020 Apr
3. Epub ahead of print. Crossref
19. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138
hospitalized patients with 2019 novel coronavirus-infected
pneumonia in Wuhan, China. JAMA 2020;323:1061-9. Crossref
20. Ai T, Yang Z, Hou H, et al. Correlation of chest CT and
RT-PCR testing in coronavirus disease 2019 (COVID-19)
in China: a report of 1014 cases. Radiology 2020;296:E32-
40. Crossref
21. Cao B, Wang Y, Wen D, et al. A trial of lopinavir–ritonavir
in adults hospitalized with severe COVID-19. N Engl J
Med 2020;382:1787-99. Crossref