Hong Kong Med J 2020 Aug;26(4):289–93 | Epub 30 Jul 2020
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE CME
Patterns of COVID-19 on computed tomography
imaging
SK Li, MB, ChB, FRCR; FH Ng, FHKCR, FHKAM (Radiology); KF Ma, FHKCR, FHKAM (Radiology); WH Luk, FHKAM (Radiology), FRCR; YC Lee, FHKAM (Radiology), FRCR; KS Yung, MB, BS
Department of Radiology, Princess Margaret Hospital, Hong Kong
Corresponding author: Dr SK Li (leskileskileskileski@gmail.com)
Abstract
Purpose: As the designated tertiary referral centre
for infectious diseases in Hong Kong, our hospital
received the city’s first group of patients diagnosed
with coronavirus disease 2019 (COVID-19). Herein,
we studied the earliest patients admitted to our
centre in order to clarify the typical radiological
findings, particularly computed tomography (CT)
findings, associated with COVID-19.
Methods: From 22 January 2020 to 29 February 2020,
19 patients with confirmed COVID-19 underwent
high-resolution or conventional CT scans of the
thorax in our centre. The CT imaging findings of
these patients with confirmed COVID-19 in Hong
Kong were reviewed in this study.
Results: Ground-glass opacities (GGO) with
peripheral subpleural distribution were found in all
patients (100%). No specific zonal predominance
was observed. All lobes were involved in 16 (84.2%)
patients, focal subsegmental consolidations were
observed in 14 (73.7%) patients, and interlobular
septal thickening was present in 12 (63.2%)
patients. No mediastinal lymph node enlargement,
centrilobular nodule, or pleural effusion was
detected in any of the patients. Other imaging features present in several patients include bronchial
dilatation, bronchial wall thickening, and crazy-paving
patterns.
Conclusion: Peripheral subpleural GGO without
zonal predominance in the absence of centrilobular
nodule, pleural effusion, and lymph node enlargement
were consistent findings in patients with confirmed
COVID-19. The observed radiological patterns on
CT scans can help identify COVID-19 and assess
affected patients in the context of the ongoing
outbreak.
New knowledge added by this study
- Peripheral subpleural ground-glass opacities without zonal predominance in the absence of centrilobular nodules, pleural effusion, and lymph node enlargement were consistent findings in initial thoracic computed tomography scans of patients with coronavirus disease 2019 (COVID-19) in Hong Kong.
- Lung changes in patients with COVID-19 have no zonal predominance, which contrasts with the findings in patients with severe acute respiratory syndrome or Middle East respiratory syndrome, which predominantly affect basal zones.
- Knowledge of common radiological patterns on computed tomography of the thorax can help discern the extent of pulmonary involvement and potentially facilitate identification of patients with pneumonia in Hong Kong during the COVID-19 outbreak.
- Air-space opacities are less frequent in patients with COVID-19 pneumonia, compared with patients with severe acute respiratory syndrome or Middle East respiratory syndrome, which implies that the course of COVID-19 pneumonia might be less aggressive.
Introduction
The Health Commission of Hubei province, China,
first announced a cluster of patients with atypical
pneumonia of unidentified pathogenic cause on
31 December 2019.1 The virus was isolated; its genome
was then sequenced by a number of Chinese scientists
who confirmed it to be a type of coronavirus. The
virus was named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and the resulting
disease was termed coronavirus disease 2019
(COVID-19) by the World Health Organization.2
The infectious disease centre at Princess Margaret
Hospital, Hong Kong, is the designated local tertiary
referral centre that provides treatment for patients
diagnosed with COVID-19. Case reports available
at the time of writing describe ground-glass lung changes in isolated patients with COVID-19.3 4 5
Herein, we evaluate the radiological features in the
earliest group of patients with confirmed COVID-19
in Hong Kong. The aim of the present study was to
provide insights into radiological identification and
assessment of COVID-19 pneumonia.
Methods
Patients in this study were confirmed to have
SARS-CoV-2 infection on the basis of a positive
nasopharyngeal aspirate reverse transcription
polymerase chain reaction result and/or a positive
serological testing result. The first 20 confirmed
patients from all hospitals in Hong Kong were sent
to our infectious disease unit for quarantine and
treatment.
The radiological images reviewed in this study
were obtained with high-resolution computed
tomography (CT) or conventional thoracic CT. The
examinations were performed with a multi-slice
16-head detector scanner (LightSpeed; GE Medical
Systems, Waukesha [WI], United States) in the
infectious disease centre, which is equipped with a
negative pressure ventilating system.
The following parameters were used for high-resolution
CT of the thorax: voltage, 120 kVp;
current, 30-300 mA (smart mA); field of view,
32-40 mm; and gantry rotation, 1.0 s. Conventional
CT was performed with the following parameters:
voltage, 120 kVp; current, 100-500 mA (smart mA);
diagonal field of view, 40 mm; and gantry rotation,
0.5 s.
Radiographers who performed CT scans of
patients with confirmed or suspected COVID-19
were required to wear full-body protective garments,
in accordance with guidelines from infection control
specialists. All radiographers wore disposable fluid-resistant
gowns, gloves, face shields, face masks with
a rating of at least N95 (3M; Aberdeen [SD], United
States), disposable shoe wraps, and protective
eyewear. Patients were also required to wear masks
with a rating of at least N95. All surfaces in contact
with or within 1 m of the patients were cleaned
with antiviral agents after completion of scanning.
Cleaning procedures were performed twice;
subsequently, the CT suite was not used for at least
30 minutes to allow for several air exchanges prior to
the entry of the next patient.
The radiological images were reviewed and
interpreted by consensus; the reviewers were two
consultant radiologists who were registered specialist
radiologists under Hong Kong Medical Council,
Fellows of the Royal College of Radiologists, and
Fellows of the Hong Kong College of Radiologists
with 20 years of experience each in body CT.
Results
From 22 January 2020 to 29 February 2020, our
hospital received 20 patients aged 25 to 80 years
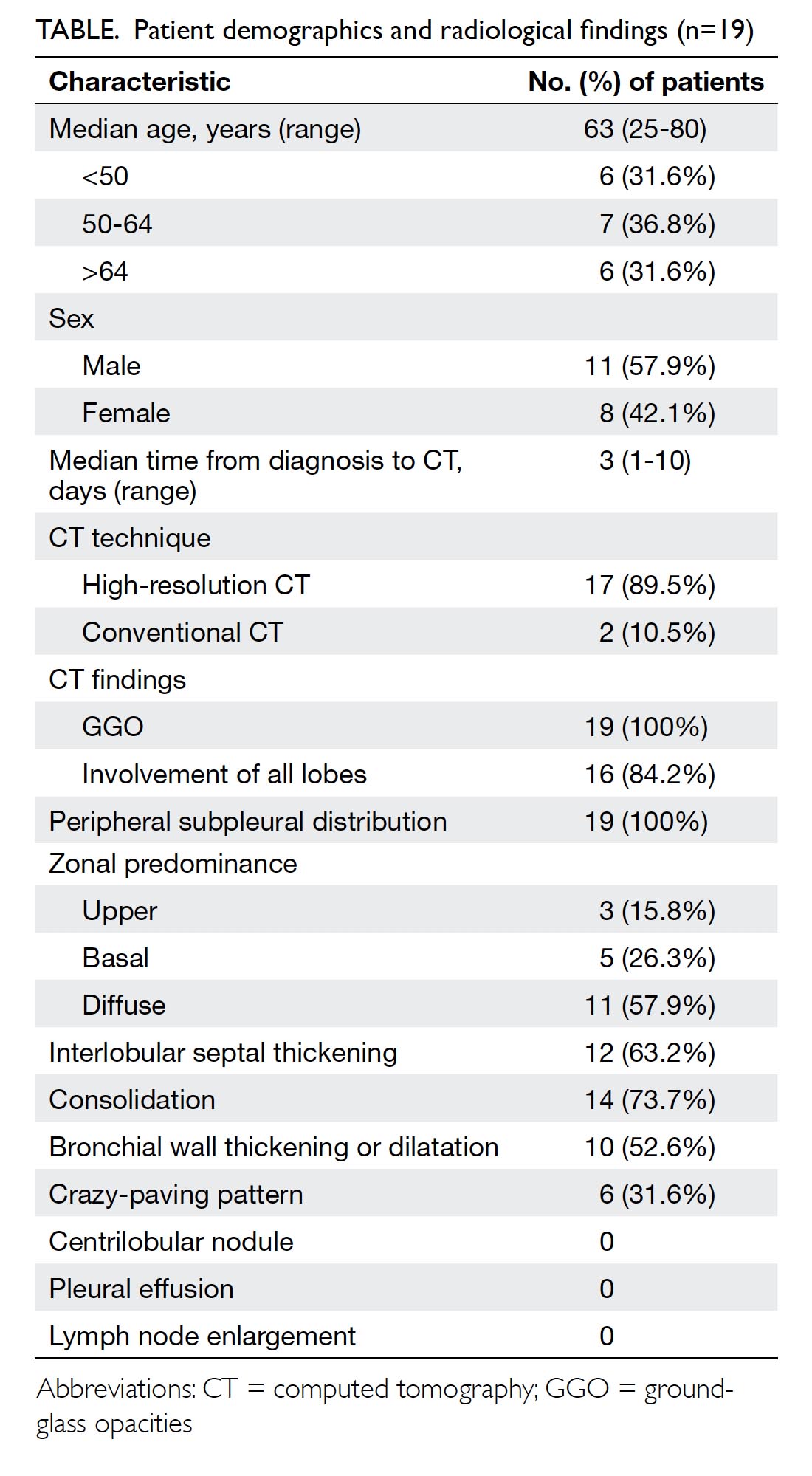
all with confirmed COVID-19 (Table). Chest
radiographs were performed for all patients
on admission; the most common finding was
bilateral non-specific pulmonary infiltrates (Fig 1).
Shortly after admission, 19 patients (11 men and
eight women) underwent high-resolution CT
or conventional plain CT thorax. One patient
was asymptomatic and exhibited normal chest
radiographs throughout the hospital stay; thus, no
CT scans were performed for further evaluation.
The median interval from confirmation of diagnosis
to CT scanning was 3 days.
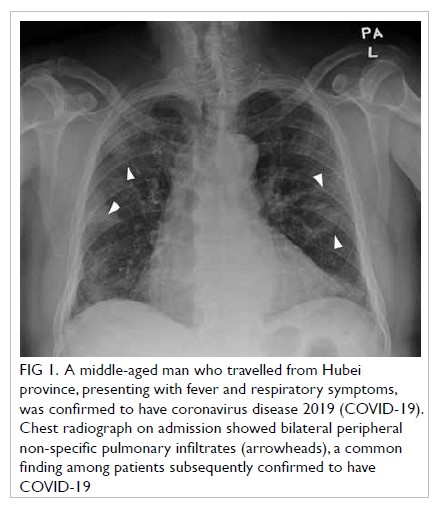
Figure 1. A middle-aged man who travelled from Hubei province, presenting with fever and respiratory symptoms, was confirmed to have coronavirus disease 2019 (COVID-19). Chest radiograph on admission showed bilateral peripheral non-specific pulmonary infiltrates (arrowheads), a common finding among patients subsequently confirmed to have COVID-19
As indicated in the Table, ground-glass opacities
(GGO) with peripheral subpleural distribution
were observed in all patients (100%) [Figs 2, 3a, b].
Furthermore, 57.9% of the patients exhibited diffuse
involvement of both upper and basal zones, 15.8%
demonstrated upper zone predominance, and 26.3%
demonstrated basal predominance. All lobes of the
lungs were involved in 16 (84.2%) patients (Fig 2),
subsegmental consolidative changes were present
in 14 (73.7%) patients (Fig 3a, c), interlobular septal
thickening was present in 12 (63.2%) patients (Fig 3a),
bronchial wall thickening or dilation was present
in 10 (52.6%) patients (Fig 3b), and crazy-paving
patterns were present in six (31.6%) patients (Fig 3).
Mediastinal lymph node enlargement (ie, short axis
>1 cm), centrilobular nodule, and pleural effusion
were not detected in any of the patients.
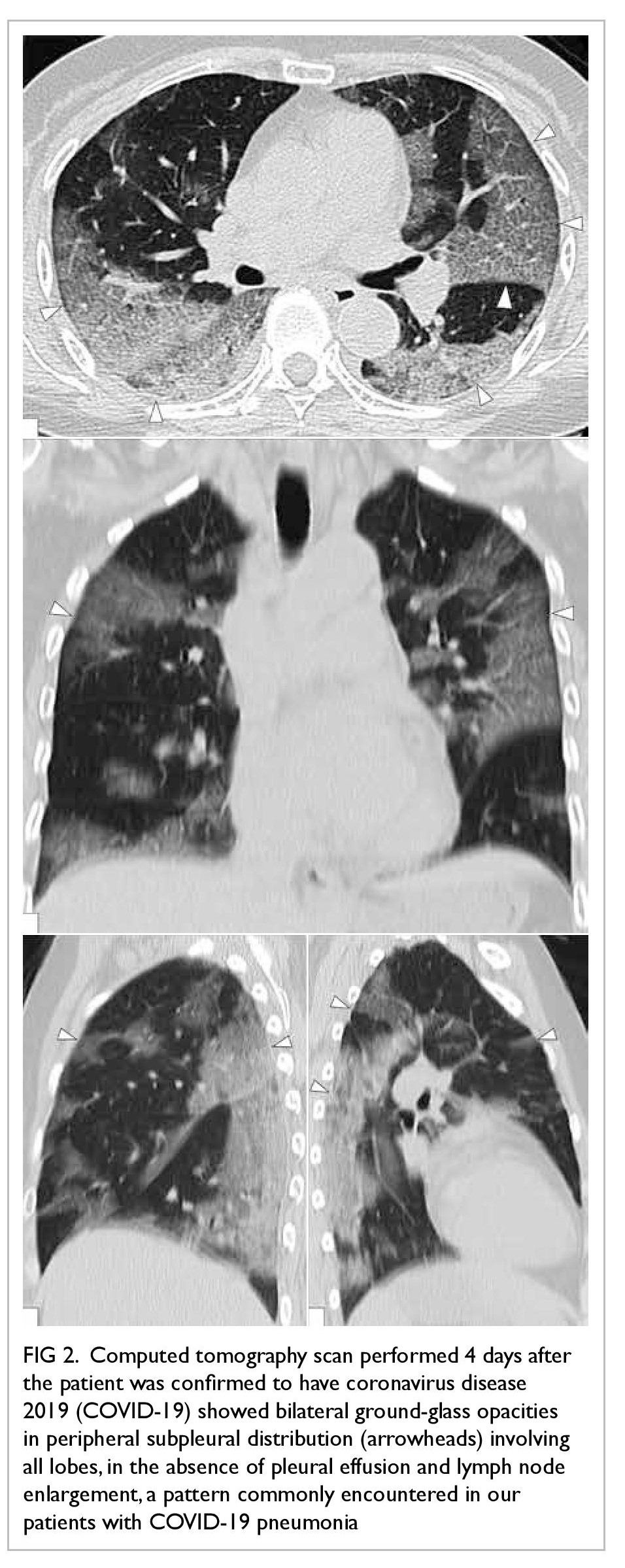
Figure 2. Computed tomography scan performed 4 days after the patient was confirmed to have coronavirus disease 2019 (COVID-19) showed bilateral ground-glass opacities in peripheral subpleural distribution (arrowheads) involving all lobes, in the absence of pleural effusion and lymph node enlargement, a pattern commonly encountered in our patients with COVID-19 pneumonia
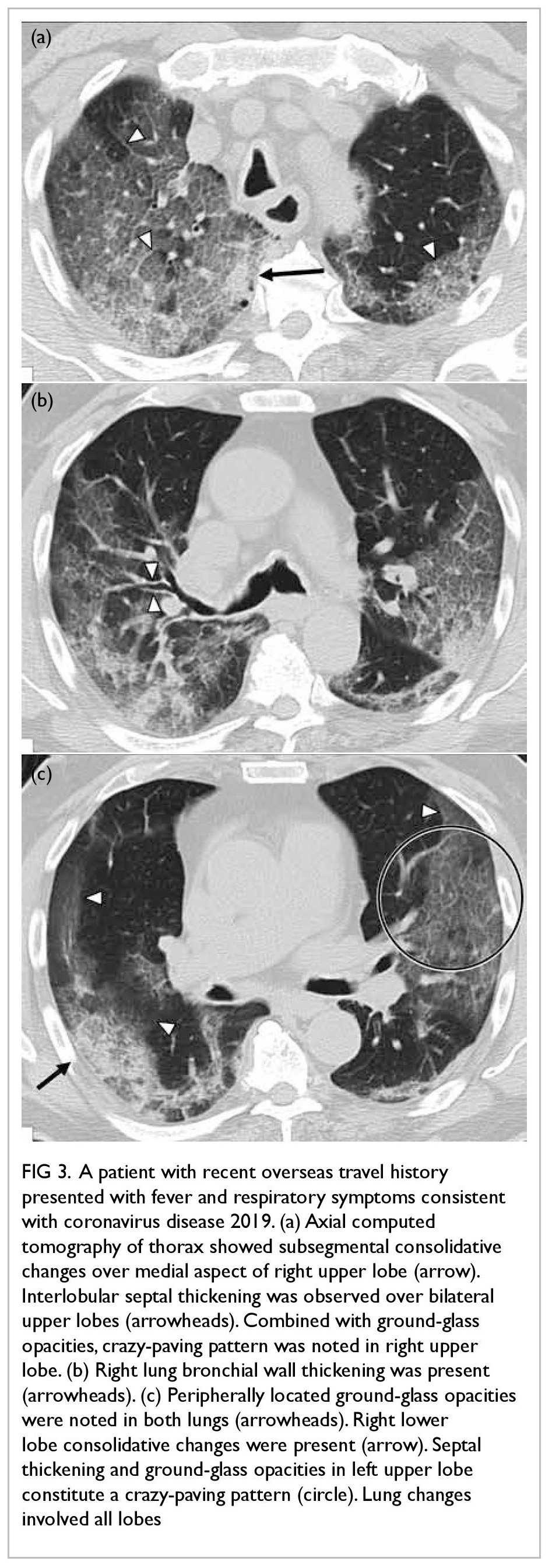
Figure 3. A patient with recent overseas travel history presented with fever and respiratory symptoms consistent with coronavirus disease 2019. (a) Axial computed tomography of thorax showed subsegmental consolidative changes over medial aspect of right upper lobe (arrow). Interlobular septal thickening was observed over bilateral upper lobes (arrowheads). Combined with ground-glass opacities, crazy-paving pattern was noted in right upper lobe. (b) Right lung bronchial wall thickening was present (arrowheads). (c) Peripherally located ground-glass opacities were noted in both lungs (arrowheads). Right lower lobe consolidative changes were present (arrow). Septal thickening and ground-glass opacities in left upper lobe constitute a crazy-paving pattern (circle). Lung changes involved all lobes
In summary, peripheral subpleural GGO
without zonal predominance in the absence of centrilobular nodules, pleural effusion, and lymph
node enlargement were consistent findings. Other
common findings included septal thickening,
consolidations, bronchial dilatation/wall thickening,
and crazy-paving patterns.
Discussion
The most common respiratory pathogens are
viruses. The imaging findings of viral pneumonia are diverse and often overlap with the findings of other
non-viral pneumonias and inflammatory conditions.
Imaging findings have been described in recent
outbreaks associated with emerging pathogens,
including severe acute respiratory syndrome (SARS)
coronavirus and Middle East respiratory syndrome
(MERS) coronavirus.6 7 Although a definite diagnosis
cannot be reached based on imaging features alone,
recognition of viral pneumonia patterns can aid
in identification of potentially infected patients,
especially during a specific viral outbreak.
Peripheral subpleural GGO without zonal
predominance in the absence of pleural effusion and
lymph node enlargement were consistent findings in
initial thoracic CT scans of patients with COVID-19.
These findings coincide with recent reports of single
patients in which the major findings comprised
multifocal patchy GGO, most evident around
the periphery.3 4 5 Several other findings including
bronchial wall thickening, bronchial dilatation,
septal thickening, and crazy-paving patterns were
also observed in a subset of patients.
Similar to our findings, diseases caused by
other β-coronaviruses (eg, SARS, MERS, and other
endemic human β-coronaviruses including OC43
and HKU1) are also characterised by multifocal
peripheral GGOs. Moreover, patients infected
with those viruses rarely exhibit cavitation,
lymphadenopathy, or pleural effusions,6 similar
to the findings in the present study. However, our
study showed that lung changes in patients with
COVID-19 have no zonal predominance, which
contrasts with the findings in patients with SARS
or MERS, which predominantly affect basal zones.6
Air-space opacities are less frequent in patients with
COVID-19 pneumonia, compared with patients
with SARS or MERS, which suggests that the course
of COVID-19 pneumonia may be less aggressive.
Nonetheless, conclusions should not be drawn
prematurely as this study only involved the initial
radiological assessment. More insights into the
temporal changes regarding radiological findings
during the progression of disease will become
available as these patients undergo follow-up scans.
Further studies that include the clinical course of
COVID-19 in these patients will be performed in the
future.
Conclusion
Coronavirus disease 2019 is a highly contagious
disease that requires high vigilance and rapid
detection. Knowledge of common radiological
patterns on CT thorax can help discern the extent
of pulmonary involvement and potentially facilitate
identification of patients with pneumonia in Hong
Kong during the COVID-19 outbreak.
Author contributions
Concept or design: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: SK Li, FH Ng.
Critical revision of the manuscript for important intellectual content: SK Li, FH Ng.
Acquisition of data: All authors.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: SK Li, FH Ng.
Critical revision of the manuscript for important intellectual content: SK Li, FH Ng.
All authors had full access to the data, contributed to the
study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
The authors have disclosed no conflicts of interest.
Acknowledgement
We would like to express our gratitude to the Infectious
Disease Team and “dirty team” physicians of Princess
Margaret Hospital, Hong Kong, for their professional patient
care and invaluable contribution to the understanding of a
novel disease.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This study was carried out with approval from the Kowloon West Cluster Ethics Committee (Ref KW/EX-20-032(144-20)). The requirement for patient consent was waived by the
committee.
References
1. Centre for Health Protection, Hong Kong SAR
Government. CHP closely monitors cluster of pneumonia
cases on Mainland. 31 December 2019. Available
from: https://www.info.gov.hk/gia/general/201912/31/P2019123100667.htm. Accessed 1 Feb 2020.
2. World Health Organization. Clinical management of
severe acute respiratory infection when COVID-19 is
suspected. Interim guidance. 12 January 2020. Available
from: https://www.who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected. Accessed 1 Feb 2020.
3. Chan JF, Yuan S, Kok KH, et al. A familial cluster of
pneumonia associated with the 2019 novel coronavirus
indicating person-to-person transmission: a study of a
family cluster. Lancet 2020;395:514-23. Crossref
4. Medlinkcn.com. 武漢19-nCoV 肺炎影像學表現初探
[in Chinese]. Available from: http://www.medlinkcn.
com/?id=138. Accessed 1 Feb 2020.
5. Lei J, Li J, Li X, Qi X. CT imaging of the 2019 novel
coronavirus (2019-nCoV) pneumonia. Radiology
2020;295:18. Crossref
6. Koo HJ, Lim S, Choe J, Choi SH, Sung H, Do KH.
Radiographic and CT features of viral pneumonia.
Radiographics 2018;38:719-39. Crossref
7. Franquet T. Imaging of pulmonary viral pneumonia.
Radiology 2011;260:18-39. Crossref