Hong Kong Med J 2020 Jun;26(3):236–9 | Epub 29 Apr 2020
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Imaging findings of critically ill patients with COVID-19 pneumonia: a case series
Stephanie C Woo, MB, BS# 1; KS Yung, MB, BS# 1;T Wong, FHKCR, FHKAM (Radiology)1; Ellen LM Yu, BSc, MSc2; SK Li, MB, ChB, FRCR1; HF Chan, FHKCR, FHKAM (Radiology)1; CH Chan, FHKCR, FHKAM (Radiology)1; YC Lee, FHKCR, FHKAM (Radiology)1; Jacky MC Chan, FHKCP, FHKAM (Medicine)3; WS Leung, FRCP, FHKAM (Medicine)3
1 Department of Radiology, Princess Margaret Hospital, Hong Kong
2 Clinical Research Centre, Princess Margaret Hospital, Hong Kong
3 Department of Medicine and Geriatrics, Princess Margaret Hospital, Hong Kong
# The first two authors contributed equally to the work
Corresponding author: Dr Stephanie C Woo (stephaniecheriwoo@gmail.com)
Introduction
Between 25 January 2020 and 7 February 2020, 22 patients admitted to Princess Margaret Hospital, Hong Kong had diagnosis of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection confirmed by real-time reverse transcription polymerase chain reaction of nasopharyngeal aspirate and throat swab. Of them, three (13.6%) patients required intensive care unit (ICU) admission. Their clinical and laboratory data as well as computed tomography (CT) images were reviewed.
Herein, we review the findings from unenhanced CT scans of the thorax and serial chest radiographs in these three patients with coronavirus disease 2019 (COVID-19). The aim of the study was to provide insights into possible prognostic indicators of COVID-19 from an imaging perspective.
Case 1
In January 2020, a 68-year-old woman with travel history to Wuhan, China, was admitted to out unit presenting with fever, productive cough, and sore throat. Blood test results showed elevated C-reactive protein (CRP) level (72.9 mg/L, reference range <5 mg/L) and lactate dehydrogenase (LDH) level (295 U/L, reference range <250 U/L).
A CT scan of the thorax showed peripheral and subpleural involvement of ground-glass opacities (GGOs) and consolidations with interlobular septal thickening giving rise to a crazy-paving appearance. These abnormalities involved all lobes with a posterior predominance. No pleural effusion or mediastinal lymphadenopathy was evident (Fig 1a).
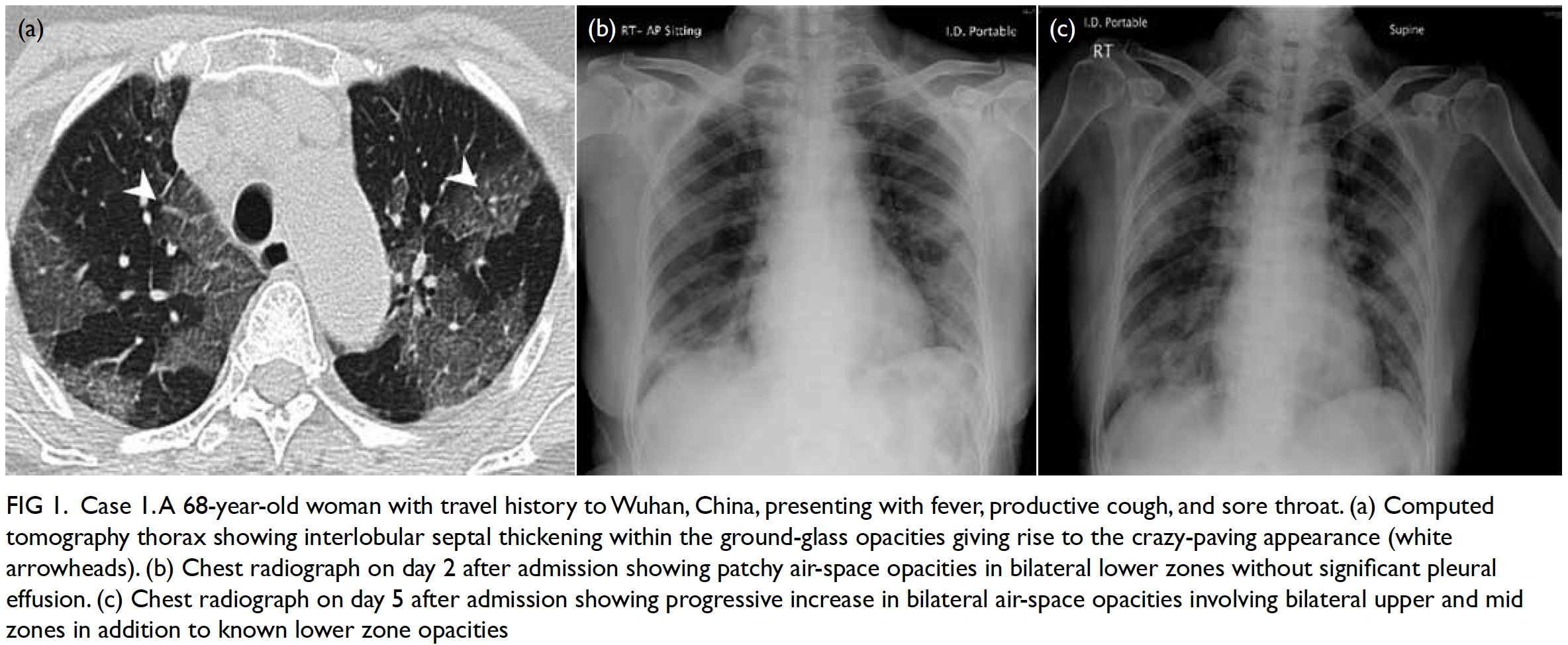
Figure 1. Case 1. A 68-year-old woman with travel history to Wuhan, China, presenting with fever, productive cough, and sore throat. (a) Computed tomography thorax showing interlobular septal thickening within the ground-glass opacities giving rise to the crazy-paving appearance (white arrowheads). (b) Chest radiograph on day 2 after admission showing patchy air-space opacities in bilateral lower zones without significant pleural effusion. (c) Chest radiograph on day 5 after admission showing progressive increase in bilateral air-space opacities involving bilateral upper and mid zones in addition to known lower zone opacities
Initial chest radiograph showed moderate bilateral air-space opacities with lower zonal predominance (Fig 1b). Subsequently, the patient’s condition deteriorated with worsening dyspnoea requiring increasing oxygen support. Serial chest radiographs showed progression of the air-space opacities (Fig 1c). However, costophrenic angles remained sharp despite disease progression, indicating the absence of significant pleural effusion. The patient was admitted to the ICU for intubation due to respiratory failure.
Case 2
In February 2020, a 64-year-old woman with travel history to Bangkok, Thailand, was admitted to out unit presenting with fever and dyspnoea, but no upper respiratory tract symptoms. Blood test results showed leucocytosis (12.6 × 109/L, reference range, 3.7-9.2 × 109/L) and elevated CRP (244 mg/L) and LDH (683 U/L) levels.
A CT scan of the thorax showed peripheral and subpleural involvement of GGOs and consolidations with interlobular septal thickening giving rise to a crazy-paving appearance. These abnormalities involved all lobes with a posterior predominance. No pleural effusion or mediastinal lymphadenopathy was evident (Fig 2a and b).
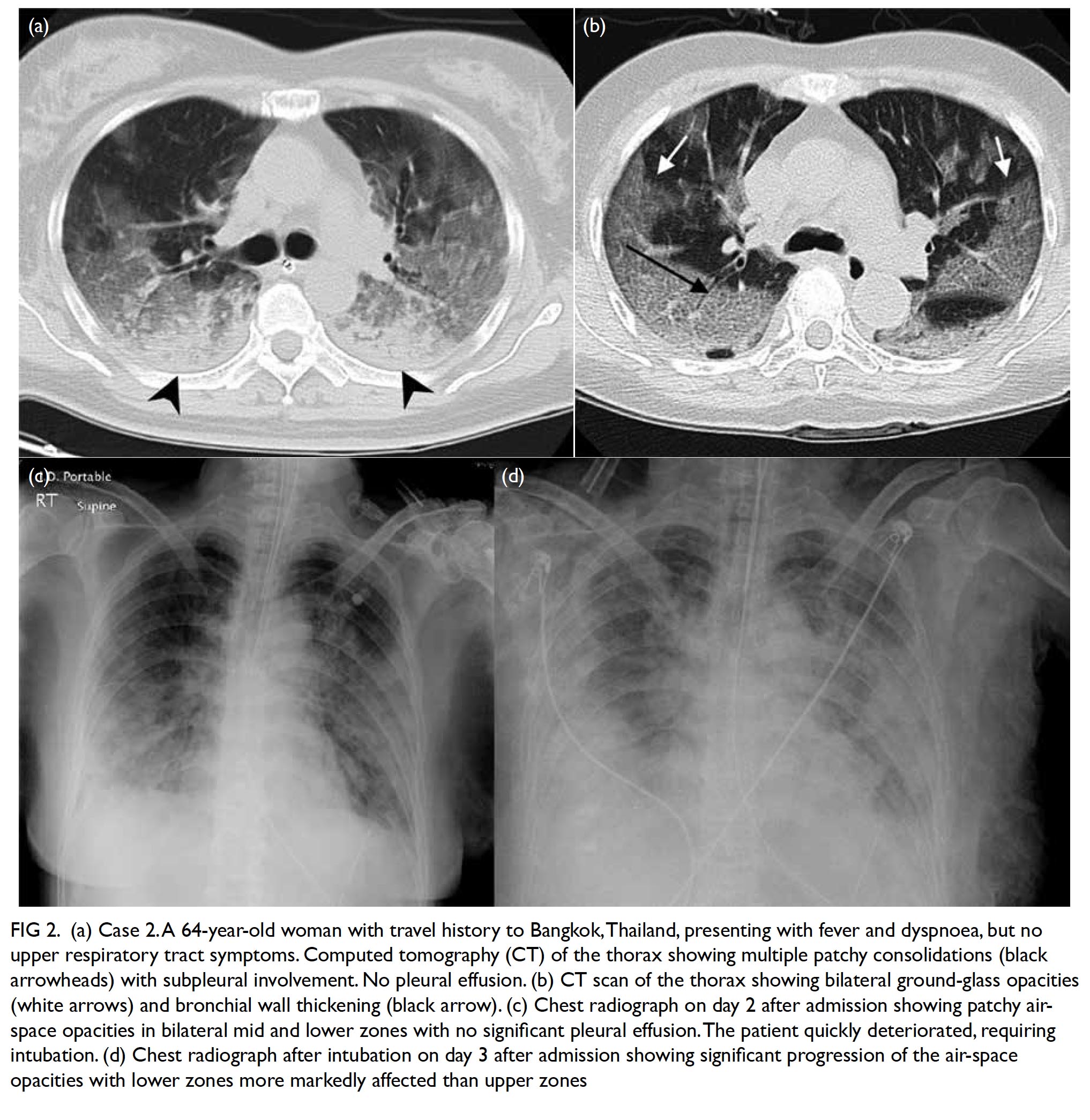
Figure 2. a) Case 2. A 64-year-old woman with travel history to Bangkok,Thailand, presenting with fever and dyspnoea, but no upper respiratory tract symptoms. Computed tomography (CT) of the thorax showing multiple patchy consolidations (black arrowheads) with subpleural involvement. No pleural effusion. (b) CT scan of the thorax showing bilateral ground-glass opacities (white arrows) and bronchial wall thickening (black arrow). (c) Chest radiograph on day 2 after admission showing patchy air-space opacities in bilateral mid and lower zones with no significant pleural effusion.The patient quickly deteriorated, requiring intubation. (d) Chest radiograph after intubation on day 3 after admission showing significant progression of the air-space opacities with lower zones more markedly affected than upper zones
Initial chest radiograph showed extensive
air-space opacities with lower zonal predominance (Fig 2c). Subsequently, the patient’s condition deteriorated with worsening dyspnoea requiring increasing oxygen support. Serial chest radiographs showed progression of the air-space opacities (Fig 2d). However, costophrenic angles remained sharp despite disease progression, indicating the absence of significant pleural effusion.
The patient was admitted to the ICU for intubation due to respiratory distress and rapid deterioration.
Case 3
In January 2020, a 56-year-old man with travel history to Wuhan, China, was admitted to out unit presenting with fever and productive cough. Blood test results showed lymphocytopenia (0.7 × 109/L, reference range 1.1-2.9 × 109/L) and elevated CRP (33.2 mg/L) and LDH (266 U/L) levels.
A CT scan of the thorax showed peripheral and subpleural involvement of GGOs and consolidations. These abnormalities involved all lobes with a posterior predominance. No pleural effusion or mediastinal lymphadenopathy was evident (Fig 3a).
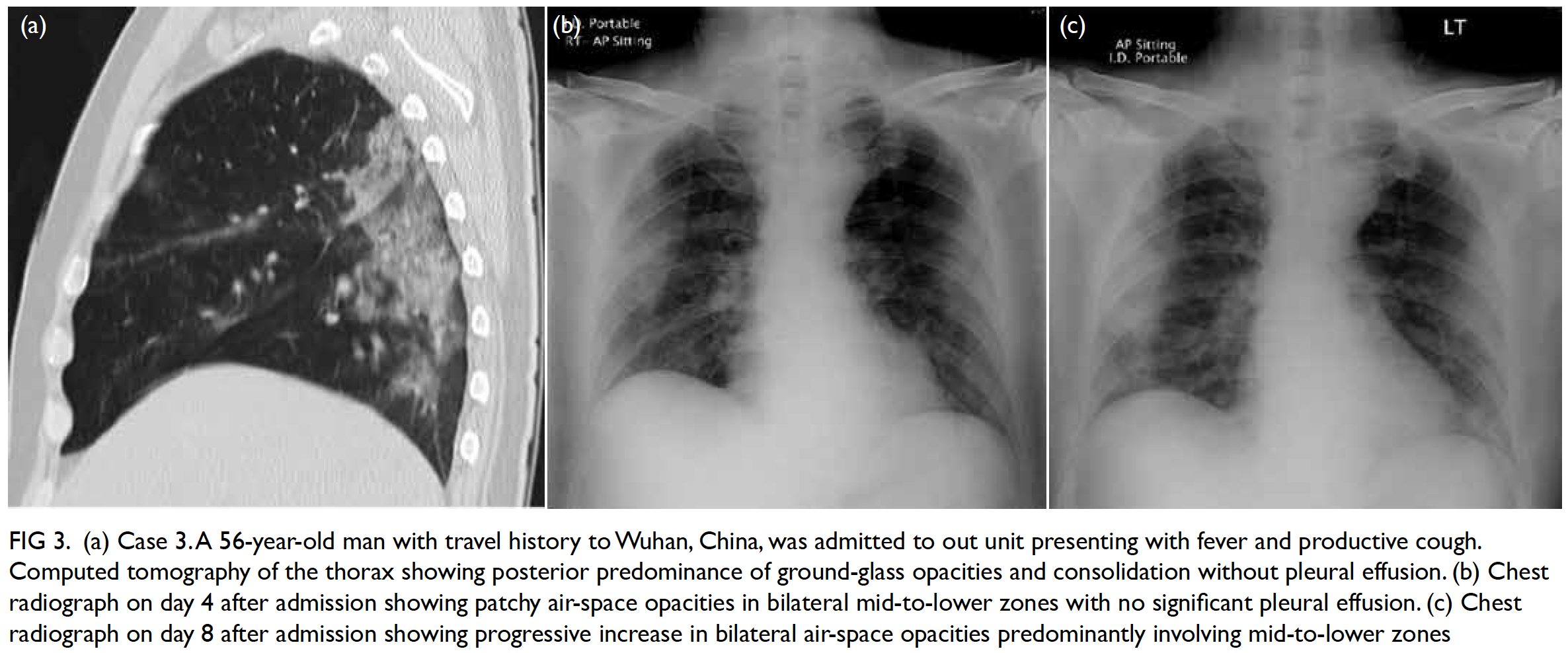
Figure 3. (a) Case 3. A 56-year-old man with travel history to Wuhan, China, was admitted to out unit presenting with fever and productive cough. Computed tomography of the thorax showing posterior predominance of ground-glass opacities and consolidation without pleural effusion. (b) Chest radiograph on day 4 after admission showing patchy air-space opacities in bilateral mid-to-lower zones with no significant pleural effusion. (c) Chest radiograph on day 8 after admission showing progressive increase in bilateral air-space opacities predominantly involving mid-to-lower zones
Initial chest radiograph showed mild to moderate air-space opacities with lower zonal predominance (Fig 3b). Subsequently, the patient’s condition deteriorated with worsening dyspnoea requiring increasing oxygen support. Serial chest radiographs showed progression of the air-space opacities (Fig 3c). However, costophrenic angles remained sharp despite disease progression, indicating the absence of significant pleural effusion.
The patient was admitted to the ICU for escalating need of high-flow nasal oxygen; intubation was not required.
Discussion
The current COVID-19 outbreak was first reported in Wuhan, China, in December 2019.1 On 23 January 2020, the first two confirmed cases of COVID-19 infection were reported in Hong Kong.2 In our patients, we observed a high frequency of occurrence of consolidations in addition to GGOs. The lesions showed bilateral peripheral involvement with initial lower zone predominance in all cases.
Multifocal peripheral GGOs in all of our patients are in keeping with findings of other recent studies on patients with COVID-19.3 4 This is also consistent with infections caused by other members of the betacoronavirus genus, including SARS-CoV5 and Middle East respiratory syndrome coronavirus (MERS-CoV).6 The presence of GGOs were reported to be up to 86% and 87% in the recently published reviews of patients with COVID-19 pneumonia.3 4 Different patterns of GGOs have been described in patients with COVID-19 pneumonia, with predominant posterior and peripheral lung distribution of GGOs being the most commonly described pattern.4 Such distribution is in line with observations of our patients but is less frequently reported in other non-coronavirus pneumonias.4
In contrast, consolidation is a much less common finding (ranging from 29% to 59%) in published studies of COVID-19 pneumonia.3 4 These studies included patients with varying disease severity. Since we only included critically ill patients requiring ICU admission, we postulate that the presence of consolidation can reflect a more aggressive disease, presenting a potential predictive feature for poorer prognosis. This observation is supported by a recent case review of COVID-19 pneumonia that found patients admitted to the ICU were more likely to have larger areas of bilateral consolidations on CT scans.3 On the contrary, GGOs are the main manifestation of patients who have milder disease.3 Pure GGOs without consolidations were reported in 77% of patients in another recent study.4 In addition, studies of MERS-CoV infection have also suggested that the presence of confluent consolidations is a radiological feature that might be predictive of poor prognosis.7 8
A limitation of the present case series is the limited sample size. Further studies with a larger sample size should be conducted to identify relevant radiological prognostic factors to confirm our initial findings.
Pleural effusion and mediastinal lymphadenopathy were absent in all of our cases. This is consistent with the low occurrence of these findings in other studies of patients with COVID-19 pneumonia. In one recent study, none of the patients were reported to have pleural effusion or mediastinal lymphadenopathy.3 In another study, pleural effusion and mediastinal lymphadenopathy were reported in 8% and 6% of patients, respectively.4 Previous studies of MERS-CoV infection found that pleural effusion may indicate poorer prognosis.7 8 However, this finding was absent in our patients.
All of our patients suffered from relatively rapid clinical deterioration with aggravation of air-space opacities on serial chest radiographs with GGOs and consolidations on CT scans of the thorax. Acute respiratory distress syndrome (ARDS) was found to be involved in a case series of patients with SARS-CoV infection.5 The authors of that case series concluded that the radiographic and CT findings of bilateral GGOs or consolidations and the rapid progression seen in some of their patients were consistent with ARDS, as autopsy findings of those deceased patients showed histological features identical to ARDS.5 This pathophysiology may also be applicable to COVID-19 pneumonia. This requires further verification by future studies with a larger sample size.
To conclude, we reported the radiological findings of three critically ill patients diagnosed with COVID-19 requiring ICU admission in Hong Kong. The presence of consolidations on CT of the thorax possibly indicates a more aggressive disease, and such observations are in line with the literature.
Author contributions
Concept or design: SC Woo, KS Yung, T Wong.
Acquisition of data: SC Woo, KS Yung, JMC Chan, WS Leung.
Analysis or interpretation of data: SC Woo, KS Yung, T Wong, ELM Yu, SK Li, HF Chan, CH Chan, YC Lee.
Drafting of the manuscript: SC Woo, KS Yung, T Wong, SK Li, HF Chan, CH Chan, YC Lee, JMC Chan, WS Leung.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: SC Woo, KS Yung, JMC Chan, WS Leung.
Analysis or interpretation of data: SC Woo, KS Yung, T Wong, ELM Yu, SK Li, HF Chan, CH Chan, YC Lee.
Drafting of the manuscript: SC Woo, KS Yung, T Wong, SK Li, HF Chan, CH Chan, YC Lee, JMC Chan, WS Leung.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
The authors have no conflicts of interest to disclose.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This study was approved by Kowloon West Cluster Research Ethics Committee (Ref EX-20-033(144-21)). The need for patient consent was waived by the Research Ethics Committee.
References
1. World Health Organization. Novel Coronavirus (2019- nCoV) Situation Report-1. 2020 Jan 20. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov.pdf?sfvrsn=20a99c10_4. Accessed 3 Feb 2020.
2. Centre for Health Protection, Hong Kong SAR Government. CHP announces latest situations and measures on imported cases of novel coronavirus infection [press release]. 2020 January 23. Available from: https://www.info.gov.hk/gia/general/202001/23/P2020012300914.htm. Accessed 3 Feb 2020.
3. Kanne JP. Chest CT findings in 2019 novel coronavirus (2019-nCoV) infections from Wuhan, China: key points for the radiologist. Radiology 2020;295:16-7. Crossref
4. Song F, Shi N, Shan F, et al. Emerging 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology 2020;295:210-7. Crossref
5. Müller NL, Ooi GC, Khong PL, Nicolaou S. Severe acute respiratory syndrome: radiographic and CT findings. AJR Am J Roentgenol 2003;181:3-8. Crossref
6. Ajlan AM, Ahyad RA, Jamjoom LG, Alherthy A, Madani TA. Middle East respiratory syndrome coronavirus (MERS-CoV) infection: chest CT findings. AJR Am J Roentgenol 2014;203:782-7. Crossref
7. Lee SE, Kim HL, Choi SM. A fatal case of Middle East respiratory syndrome corona virus infection in South Korea: chest radiography and CT findings. J Korean Soc Radiol 2016;74:407-11. Crossref
8. Das KM, Lee EY, Enani MA, et al. CT correlation with outcomes in 15 patients with acute Middle East respiratory syndrome coronavirus. AJR American J Roentgenol 2015;204:736-42. Crossref

