© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
LETTER TO THE EDITOR
Low mortality and severe complications despite high
influenza burden among Hong Kong children
KL Hon, MB, BS, MD1,2; Julian W Tang,
PhD, FRCPath3
1 Department of Paediatrics and
Adolescent Medicine, The Hong Kong Children’s Hospital, Kowloon Bay, Hong
Kong
2 Department of Paediatrics, The Chinese
University of Hong Kong, Shatin, Hong Kong
3 Department of Infection, Immunity and
Inflammation, University Hospitals of Leicester NHS Trust, United Kingdom
Corresponding author: Dr KL Hon (ehon@hotmail.com)
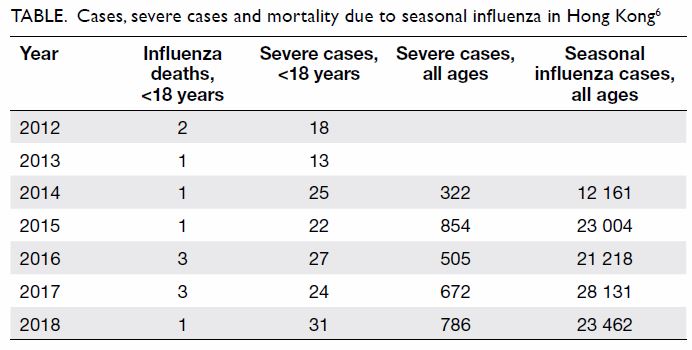
To the Editor—Every winter, the Hong Kong
Hospital Authority appeals to the public for understanding amid
overcrowding at the city’s public hospitals as influenza cases spike. The
Centre for Health Protection (CHP) has been reporting the annual influenza
burden and confirms that, in Hong Kong, there has been no significant
increase in mortality among patients with influenza aged <18 years.
Among paediatric patients, there are few severe cases and few deaths each
year, usually among unimmunised children, in a population of around 1.5
million children and youths.1 2 3 4 5
The burden on public hospitals may be due, in part,
to the low immunisation rate among children. Paediatric patients with
severe influenza may require in-patient stays of 1 to 2 days. Paediatric
patients who require urgent care must be prioritised and should not have
to wait for >8 hours pending assessment or admission. Yet this may be
inevitable if the department becomes overcrowded with too many competing
demands on staff time. Ideally, patients should be seen initially by their
family doctors and stay home to recover if their admission is not
necessary or urgent.
Excessive and exaggerated media publicity over the
relatively few annual influenza-related deaths and severe cases may
contribute to public panic, with increased admissions, some of which may
be unnecessary, leading to higher workloads for medical staff—all of which
may serve to delay the assessment of severe cases. The media may
constructively spend their energy in lobbying for immunisation in the
local healthcare system to help to relieve the pressure on an already
over-burdened and under-funded hospital healthcare system.
Seasonal influenza continues to cause significant
morbidity, but not mortality or intensive care admissions among children
and young persons in Hong Kong. Influenza-related morbidity in terms of
severe cases in patients aged <18 years has increased but the total
number is still low Table 6).
Immunisation rates can be enhanced using targeted
strategies for healthcare practices and providers. Sufficient vaccine
supply should be secured annually. School vaccination teams provide
excellent timely delivery of vaccines to schoolchildren. Private medical
practitioners are also generally willing to be involved and their
involvement would help to relieve the intense manpower needed for
influenza vaccination prior to (and sometimes during) the annual influenza
season.
Influenza is a serious public health concern
globally. Public misunderstandings, unfounded fears, and various myths
surrounding influenza, influenza vaccines, and other essential childhood
immunisations must be addressed. Prevention and prompt diagnosis and
treatment of influenza reduces morbidity.7
Physicians, school teachers, parents, and policy makers should cooperate
to effectively coordinate and deliver the annual seasonal influenza
immunisation programme, as well as the management of acute influenza
infections that present to our healthcare services. Children with
infectious diseases who are nevertheless still relatively well should try
to recover at home and avoid school, nurseries, or other public places, to
prevent the spread of infectious diseases such as influenza.
Author contributions
All authors have contributed to the concept,
acquisition of data, analysis of data, drafting of the article, and
critical revision for important intellectual content. All authors had full
access to the data, contributed to the study, approved the final version
for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors declared no conflicts of interest.
Funding/support
This report received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
References
1. Chan PK, Tam WW, Lee TC, et al.
Hospitalization incidence, mortality, and seasonality of common
respiratory viruses over a period of 15 years in a developed subtropical
city. Medicine (Baltimore) 2015;94:e2024. Crossref
2. Hon KL, Luk MP, Fung WM, et al.
Mortality, length of stay, bloodstream and respiratory viral infections in
a pediatric intensive care unit. J Crit Care 2017;38:57-61. Crossref
3. Hon KL, Leung TF, Cheung KL, Ng PC, Chan
PK. Influenza and parainfluenza associated pediatric ICU morbidity. Indian
J Pediatr 2010;77:1097-101. Crossref
4. Hon KL, Leung E, Tang J, et al.
Premorbid factors and outcome associated with respiratory virus infections
in a pediatric intensive care unit. Pediatr Pulmonol 2008;43:275-80. Crossref
5. Chiu SS, Kwan MY, Feng S, et al.
Influenza vaccine effectiveness against influenza A (H3N2)
hospitalizations in children in Hong Kong in a prolonged season, 2016/17.
J Infect Dis 2018;217:1365-71. Crossref
6. Cheung E. Girl, 3, becomes first child
fatality winter flu season in Hong Kong. South China Morning Post 2018 Jan
15. Available from:
https://www.scmp.com/news/hong-kong/health-environment/article/2128294/girl-3-becomes-first-child-fatality-winter-flu.
Accessed 28 May 2019.
7. Muthuri SG, Venkatesan S, Myles PR, et
al. Effectiveness of neuraminidase inhibitors in reducing mortality in
patients admitted to hospital with influenza A H1N1pdm09 virus infection:
a meta-analysis of individual participant data. Lancet Respir Med
2014;2:395-404. Crossref