© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Megacolon as the presenting feature of multiple
endocrine neoplasia type 2B: a case report
L Xu, MB, BS1; KW Shek, MB, BS, FHKAM
(Radiology)1; KC Wong, MB, BS2; KL Tong, MB, BS,
FHKAM (Surgery)2; MN Hau, MB, BS3
1 Department of Radiology and Imaging,
Queen Elizabeth Hospital, Jordan, Hong Kong
2 Department of Surgery, Queen Elizabeth
Hospital, Jordan, Hong Kong
3 Department of Pathology, Queen
Elizabeth Hospital, Jordan, Hong Kong
Corresponding author: Dr L Xu (xl599@ha.org.hk)
Case report
A 29-year-old Chinese man with good past health
presented in October 2018 with acute abdominal pain and distension. On
admission, he was afebrile and normotensive (blood pressure 116/79, pulse
74). Physical examination revealed a grossly distended abdomen with
sluggish bowel sounds and mild diffuse tenderness but no guarding or
rigidity. Preliminary blood tests showed leucocytosis (17.7 × 109/L)
and metabolic acidosis (pH 7.29, base excess -4.3).
Markedly dilated large bowel loops were seen on
radiograph. A flexible sigmoidoscopy performed to exclude sigmoid volvulus
revealed no twisting point but was incomplete due to the presence of large
amounts of stool. Urgent contrast computed tomography abdomen and pelvis
showed that the entire length of the colon was grossly dilated up to 13 cm
in diameter with loss of haustration and no obstructive mass, suggestive
of megacolon. Several segments showed diminished mural enhancement.
Bilateral avidly enhancing heterogeneous adrenal masses were noted,
measuring up to 3.1 cm on the left and 3.8 cm on the right. They had a
density of about 52 HU pre-contrast and almost 150 HU in the arterial
phase. In view of their intense arterial enhancement, bilateral
pheochromocytoma was suspected (Fig 1).
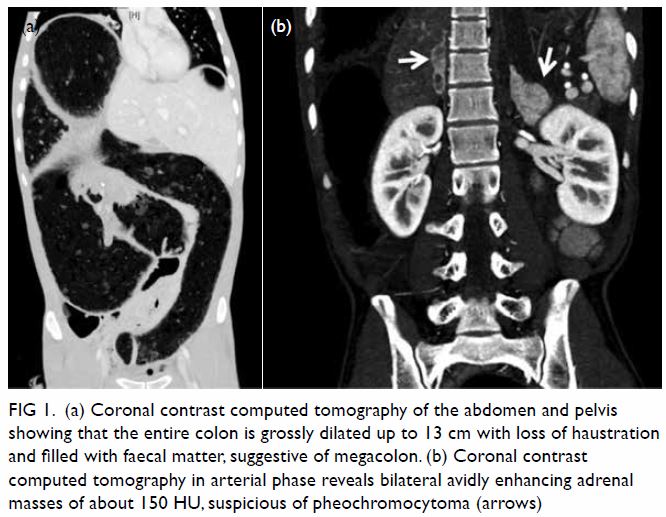
Figure 1. (a) Coronal contrast computed tomography of the abdomen and pelvis showing that the entire colon is grossly dilated up to 13 cm with loss of haustration and filled with faecal matter, suggestive of megacolon. (b) Coronal contrast computed tomography in arterial phase reveals bilateral avidly enhancing adrenal masses of about 150 HU, suspicious of pheochromocytoma (arrows)
Urgent laparotomy was deemed necessary. Due to the
suspected pheochromocytomas, the patient was prescribed an alpha blocker
to prevent catecholamine crisis and had intensive intra-operative and
postoperative blood pressure monitoring.
Laparotomy revealed that the entire large bowel was
grossly dilated with the caecum and ascending colon showing doubtful
viability. The small bowel was only mildly dilated at the terminal ileum.
Subtotal colectomy with ileostomy was therefore performed. Blood pressure
remained stable intra-operatively.
The gross subtotal colectomy specimen was extremely
dilated, up to 13 cm in diameter, with no tumour mass or perforation.
Microscopic examination revealed diffuse expansion of the myenteric plexus
in the muscularis propria, accompanied by many ganglion cells. There was
extension of the myenteric plexus into the muscles, almost reaching the
serosa, and many abnormally thick nerve bundles in the submucosa. The
appendix and the terminal ileum were also involved, with thick nerve
fibres in the lamina propria. Pathological findings were suggestive of
diffuse ganglioneuromatosis (Fig 2).
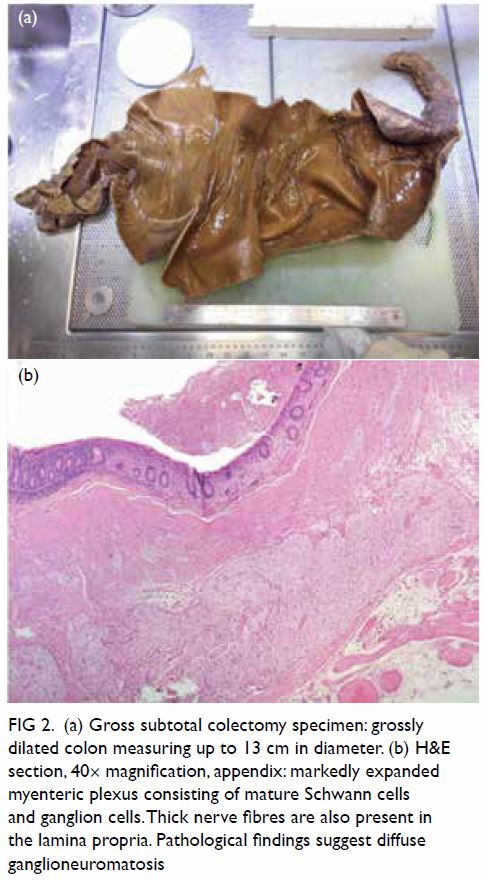
Figure 2. (a) Gross subtotal colectomy specimen: grossly dilated colon measuring up to 13 cm in diameter. (b) H&E section, 40× magnification, appendix: markedly expanded myenteric plexus consisting of mature Schwann cells and ganglion cells. Thick nerve fibres are also present in the lamina propria. Pathological findings suggest diffuse ganglioneuromatosis
Multiple 24-hour urine catecholamine tests were
performed over weeks to avoid the confounding effects of stress in the
immediate postoperative period. They confirmed the diagnosis of
pheochromocytoma with persistently and markedly raised catecholamines:
adrenaline up to 4371 nmol/d (ref <90), noradrenaline 4523 nmol/d (ref
<610), normetanephrine 1286 nmol/d (ref <320), and free metanephrine
3341 nmol/d (ref <271).
Subsequent I-131 meta-iodobenzylguanidine (MIBG)
whole-body scan showed markedly increased MIBG uptake at the left adrenal
region and moderately increased uptake at the right, in keeping with
bilateral pheochromocytoma. There was no scintigraphic evidence of
MIBG-avid metastasis. Serum calcitonin level was also found to be elevated
at 101 pmol/L (ref ≤2.8).
Given the elevated calcitonin and possibility of
multiple endocrine neoplasia type 2B (MEN 2B), ultrasound of the thyroid
was performed and revealed sub-centimetre, taller-than-wide hypoechoic
nodules with internal echogenic foci in both thyroid lobes and multiple
enlarged right cervical lymph nodes, also with echogenic foci (Fig
3). Ultrasound guided fine needle aspiration and cytology results
determined both thyroid nodules to be medullary carcinoma, showing
clusters of abnormal cells with immunostaining positive for calcitonin and
chromogranin. A right level IV cervical lymph node was suggestive of
metastatic medullary thyroid carcinoma (MTC).
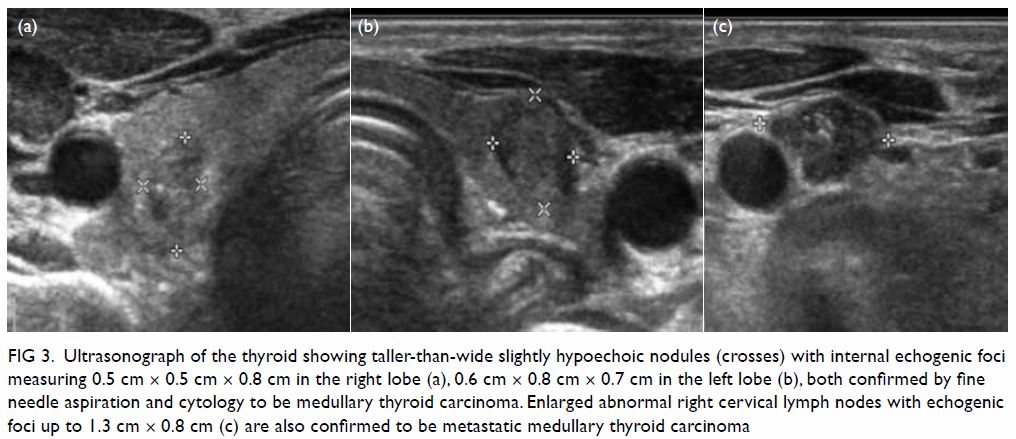
Figure 3. Ultrasonograph of the thyroid showing taller-than-wide slightly hypoechoic nodules (crosses) with internal echogenic foci measuring 0.5 cm × 0.5 cm × 0.8 cm in the right lobe (a), 0.6 cm × 0.8 cm × 0.7 cm in the left lobe (b), both confirmed by fine needle aspiration and cytology to be medullary thyroid carcinoma. Enlarged abnormal right cervical lymph nodes with echogenic foci up to 1.3 cm × 0.8 cm (c) are also confirmed to be metastatic medullary thyroid carcinoma
The diagnosis of MEN 2B was made clinically and
later confirmed by genetic testing that revealed a RET 918 mutation. This
may have been a sporadic mutation since the patient had no positive family
history. Staged surgeries for bilateral adrenalectomy followed by total
thyroidectomy and neck dissection were subsequently performed.
Discussion
Megacolon is the abnormal, often irreversible,
dilatation of the colon, greater than 12 cm in the caecum, 8 cm in the
ascending colon and 6.5 cm in the rectosigmoid region.1 The differential diagnoses for megacolon include
congenital aganglionic megacolon in Hirschsprung’s disease and toxic
megacolon in inflammatory bowel disease and infections, in particular Clostridium
difficile that can lead to pseudomembranous colitis. Other causes
include Chagas’, and Parkinson’s disease, diabetic neuropathy, myotonic
dystrophy, hypothyroidism, amyloidosis, and medications such as
risperidone and loperamide.2
Although MEN 2B associated with ganglioneuromatosis
and pheochromocytoma can also lead to megacolon, owing to its rarity, it
is often not considered in the early diagnosis of megacolon.
Multiple endocrine neoplasia is an autosomal
dominant endocrine disorder comprised of MEN type 1 and the rarer MEN type
2, and caused by familial or sporadic germline mutations in the RET
protooncogene. Multiple endocrine neoplasia 2A accounts for 80% of all MEN
type 2 cases, whereas MEN 2B, the most aggressive and rarest variant,
accounts for 5%.3 The prevalence of
MEN 2 is estimated to be one in 35 000 population, while that of MEN 2B is
approximately one in 500 000 population.4
Multiple endocrine neoplasia type 2B is
characterised by the presence of medullary thyroid cancer (100% of cases),
pheochromocytomas (40%-50% of cases), multiple neuromas and/or diffuse
gastrointestinal ganglioneuromatosis (40% of cases) as well as facial and
skeletal abnormalities, including mucosal neuromas of the lips and tongue,
medullated corneal nerve fibres, distinctive facies with enlarged lips and
in particular Marfanoid habitus.3
Gastrointestinal ganglioneuromatosis is the
predominant aetiology of gastrointestinal symptoms in MEN 2B, and results
in thickening of the myenteric plexi with hypertrophy and increased
ganglion cells, supportive cells and nerve fibres in all layers of the
bowel wall,2 as demonstrated in our
case. This leads to loss of normal bowel tone, segmental dilatation, and
megacolon, with symptoms often presenting in infancy or early childhood.
It is also important to note that sustained high
catecholamine levels secreted by pheochromocytomas can decrease intestinal
peristalsis and tone that on its own can precipitate ileus, leading to
megacolon and bowel ischaemia.5 The
bilateral pheochromocytomas in our patient may have also contributed to
the development of megacolon. Pheochromocytoma classically presents with
hypertension, palpitations, headache, and diaphoresis, although not in our
patient. It can be diagnosed clinically by elevated 24-hour urinary
excretion of catecholamines and their metabolites. On computed tomography,
pheochromocytoma is usually evident as a heterogeneous mass with areas of
necrosis and cystic change, typically enhancing avidly (attenuation ≥110
HU on arterial phase).6 Due to the
presence of these features, pheochromocytoma was suspected early on in
this case, allowing for prompt diagnosis and treatment to prevent
catecholamine crises. On magnetic resonance imaging, which is considered
the most sensitive modality with a sensitivity of 98%, pheochromocytoma is
slightly hypointense on T1-weighted and markedly hyperintense (lightbulb
sign) on T2-weighted imaging with prolonged contrast enhancement.6 Meta-iodobenzylguanidine scintigraphy may be helpful in
multifocal or extra-adrenal pheochromocytoma.
The definitive treatment is adrenalectomy and
should ideally be performed before thyroidectomy or other surgical
intervention. Adequate preoperative alpha-adrenergic receptor blockade
before beta blockade is crucial to control blood pressure and avoid
intra-operative catecholamine crisis that may lead to haemodynamic
instability and end-organ damage or dysfunction.3
Medullary thyroid carcinoma, originating from the
parafollicular calcitonin-producing cells, occurs in all MEN 2 patients.
It is the first clinical manifestation in most cases, appearing between
the age of 5 and 25 years in MEN 2A patients and is more aggressive,
developing a decade earlier in MEN 2B patients.1
Individuals with MEN 2B who do not undergo thyroidectomy by age 1 year are
prone to metastatic disease and have an average life expectancy of 21
years. Surprisingly, our patient again presented late.
Medullary thyroid carcinoma correlates with
increased serum levels of calcitonin. On ultrasound, primary thyroid
lesions and metastatic lymph nodes show punctate high echogenic foci, as
seen in our case. About 30% of MTCs show uptake in MIBG scan.
Fluorodeoxyglucose–positron emission tomography may be used for metastatic
disease and is about 75% sensitive.7
The MEN 2B is a rare but important disease complex.
Early diagnosis is necessary due to the risk of endocrine malignancies,
particularly MTC, and prophylactic thyroidectomy is advised. As
demonstrated in this case, although the patient had a rather late
presentation and no family history, earlier diagnosis of MEN 2B can be
achieved by recognising its phenotypical features and understanding that
gastrointestinal ganglioneuromatosis as well as associated
pheochromocytoma, which often have characteristic clinical and
radiological features, may lead to loss of bowel tone, causing bowel
dilatation and even megacolon.
Author contributions
All authors contributed to the concept of study,
acquisition and analysis of data, drafting of the article, and critical
revision for important intellectual content. All authors had full access
to the data, contributed to the study, approved the final version for
publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of
interest.
Funding/support
This case report received no specific grant from
any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patient was treated in accordance with the
Declaration of Helsinki. The patient provided informed consent for all
procedures.
References
1. Camilleri M, Szarka L. Dysmotility of
the small intestine and colon. In: Yamada T, Alpers DH, Kalloo AN,
editors. Textbook of Gastroenterology. 5th ed. Oxford: Wiley-Blackwell;
2011: 1108-56. Crossref
2. Barwick KW. Gastrointestinal
manifestations of multiple endocrine neoplasia, type IIB. J Clin
Gastroenterol 1983;5:83-7. Crossref
3. Marini F, Falchetti A, Del Monte F, et
al. Multiple endocrine neoplasia type 2. Orphanet J Rare Dis 2006;1:45. Crossref
4. Znaczko A, Donnelly DE, Morrison PJ.
Epidemiology, clinical features, and genetics of multiple endocrine
neoplasia type 2B in a complete population. Oncologist 2014;19:1284-6. Crossref
5. Sweeney AT, Malabanan AO, Blake MA, de
las Morenas A, Cachecho R, Melby JC. Megacolon as the presenting feature
in pheochromocytoma. J Clin Endocrinol Metab 2000;85:3968-72. Crossref
6. Blake MA, Boland GW. Adrenal Imaging.
Totowa, NJ: Humana Press; 2009. Crossref
7. Ganeshan D, Paulson E, Duran C,
Cabanillas ME, Busaidy NL, Charnsangavej C. Current update on medullary
thyroid carcinoma. AJR Am J Roentgenol 2013;201:W867-76. Crossref

