Hong Kong Med J 2025;31:Epub 14 Apr 2025
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Willingness to pay and preferences for mindfulness-based interventions among patients with chronic low back pain in the Hong Kong public healthcare sector
Mengting Zhu, PhD1; Phoenix KH Mo, PhD1; Kailu Wang, PhD1; Hermione HM Lo, MSc1; YK Choi, PGDip2; SW Law, MSc3; Regina WS Sit1, MD
1 The Jockey Club School of Public Health and Primary Care, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong SAR, China
2 Department of Family Medicine, The New Territories East Cluster, Hospital Authority, Hong Kong SAR, China
3 Department of Orthopaedics and Traumatology, Alice Ho Miu Ling Nethersole Hospital, Hong Kong SAR, China
Corresponding author: Prof Regina WS Sit (reginasit@cuhk.edu.hk)
Abstract
Introduction: Low back pain (LBP) is a leading
cause of disability worldwide. Mindfulness-based
interventions (MBIs) are effective for LBP
management when combined with medication and
physical therapy. An understanding of patients’
willingness to pay (WTP) and preferences is needed
to integrate MBIs into standard LBP care. We
examined WTP and preferences for MBIs, as well as
associated factors, among patients with chronic LBP
in the Hong Kong public healthcare sector.
Methods: A cross-sectional survey was conducted
in two Hong Kong public hospitals. We used the
payment card method to assess patients’ WTP for
MBIs and performed a discrete choice experiment
to examine patients’ preferences for MBIs. Tobit
regression was utilised to analyse factors associated
with WTP for MBIs. Patients’ relative preferences for
MBIs were estimated through a mixed logit model.
Results: Mean WTP for an eight-session course of
MBIs was HK$258.75±508.11. Higher pain scores,
monthly family income >HK$30 000, high school
education, higher treatment expenses, and stronger
belief in MBIs were associated with greater WTP.
Patients were more likely to choose MBIs with lower
costs, greater improvements in pain relief and the
ability to perform daily activities, and a face-to-face
delivery mode.
Conclusion: Patients with chronic LBP exhibited
low WTP for MBIs. Strategies to improve education
and awareness may enhance WTP; affordability and
accessibility should be considered for individuals
from diverse socio-economic backgrounds. The
identified preferences provide insights for designing
MBIs that align with patient needs. These findings
offer valuable methodological references for other
healthcare evaluations.
New knowledge added by this study
- Patients with chronic low back pain have a low willingness to pay for mindfulness-based interventions (MBIs).
- Individuals experiencing more severe pain and possessing greater financial capacity are more willing to pay for MBIs.
- Patients prefer MBIs with lower costs, greater treatment effectiveness, and a face-to-face delivery mode.
- These findings have practical implications for the future implementation of MBIs in chronic pain management.
- This study provides a methodological reference that could be adapted for evaluation of similar treatments in diverse international settings.
Introduction
Low back pain (LBP) is a prevalent health condition
that can have disabling effects on individuals of
all ages.1 This condition also imposes substantial
socio-economic costs, as evidenced by studies
demonstrating its impacts on healthcare systems
and workforce productivity worldwide.2 3
Psychological treatments, particularly when
combined with medication and physical therapy,
are effective in managing LBP.4 Mindfulness-based
interventions (MBIs; ie, evidence-based
psychological approaches) have been shown to
reduce pain, disability, and psychological distress
associated with LBP.5 Moreover, studies have emphasised the cost-effectiveness of MBIs in
reducing chronic pain–related healthcare expenses
and productivity losses.6 7 Although the exact
mechanisms through which MBIs alleviate pain have
not been elucidated, there is evidence that they may
alter pain signal processing in the brain, fostering
acceptance and non-judgemental awareness. These
outcomes enhance pain tolerance and reduce
emotional reactivity to pain.8
Other commonly used social and
psychotherapeutic modalities include cognitive-behavioural
therapy and acceptance and commitment
therapy. Cognitive-behavioural therapy targets
maladaptive thought patterns and behaviours,9
whereas acceptance and commitment therapy
focuses on promoting psychological flexibility
despite the presence of pain.10 Mindfulness-based
interventions uniquely emphasise cultivating
present-moment awareness and acceptance of pain
sensations.11 Key advantages of MBIs include their
accessibility and cost-effectiveness: they can be
efficiently delivered in group settings (either online
or face-to-face), facilitating scalability for public
healthcare initiatives.12 13 Moreover, they have the
potential to enhance self-management skills for
sustainable pain management.14 Acceptance and
commitment therapy has limited empirical support
and mixed results regarding its effectiveness in terms of improving pain intensity among patients
with chronic pain.15 16 Cognitive-behavioural therapy
is a widely used and well-researched therapeutic
approach for chronic pain.12 However, it is considered
suitable for one-on-one (rather than group-based)
formats because it requires personalised
treatment plans that address the unique needs and
concerns of each patient.17 Furthermore, MBIs have
demonstrated greater cost-effectiveness relative to
cognitive-behavioural therapy among patients with
chronic LBP.18
In Hong Kong, approximately 90% of specialist
and inpatient care services and 30% of primary
care services are provided by the public sector.19
Given the absence of universal health insurance or
co-payment, the majority of chronic diseases (eg,
LBP) are managed within the public healthcare
system.20 The incorporation of MBIs into standard
LBP treatment within this system requires an
understanding of patients’ willingness to pay (WTP)
and preferences. Relatively few studies have explored
WTP or preferences for MBIs among patients with
chronic LBP. An understanding of WTP is crucial
for efforts to assess the perceived value of healthcare
interventions, inform policy decisions, and guide
resource allocation.21 22 Consideration of patient
preferences in healthcare service decisions can
improve uptake, adherence, efficiency, and patient
satisfaction while reducing costs.23 24
This study aimed to estimate WTP and
preferences for MBIs among patients with chronic
LBP in the public healthcare sector and to explore
factors associated with WTP and preferences for
MBIs.
Chronic LBP is significantly influenced by
psychological factors; social determinants play a
crucial role in the interpretation of chronic LBP
and the ways that individuals seek and receive pain
treatment.25 26 The socio-psychobiological model
of chronic pain represents a paradigmatic shift
from the conventional biopsychosocial model.27 28
Whereas the latter model recognises the interplay
of social, psychological, and biological factors, it
tends to prioritise biological determinants over
social and psychological aspects.27 28 In contrast, the
socio-psychobiological model primarily emphasises
social determinants, followed by psychological and
biological factors.27 28
Our research, which assesses WTP and
preferences for MBIs in the context of chronic
LBP, aligns with the socio-psychobiological model
for pain management. The examination of WTP
and preferences can provide valuable insights into
the socio-economic backgrounds of individuals
with chronic LBP, which may strongly influence
their experiences of pain and responses to pain
management interventions. The findings may
also clarify patients’ abilities to access and afford pain management strategies.29 This aspect is
particularly important because it underscores the
social dimensions of chronic pain management,
highlighting disparities and barriers that may exist in
pain experiences and access to effective interventions.
Furthermore, MBIs constitute a psychological and
group-based approach to chronic pain management,
addressing both psychological and social factors
emphasised within the socio-psychobiological
model.12 30 These interventions provide individuals
with skills to manage psychological distress linked
to chronic LBP while also promoting social support
and connectivity in group settings.31 32 By fostering
mindfulness practices, MBIs equip individuals with
coping mechanisms to navigate the psychological
distress often associated with chronic LBP, while also
enhancing social support and connectivity within
group settings.31 32
Methods
Study design and setting
We conducted a prospective cross-sectional
survey using convenience sampling to recruit
eligible patients with chronic LBP from two Hong
Kong public hospitals between September 2022
and February 2023. We utilised a discrete choice
experiment (DCE) design to examine preferences
for MBIs. This study adhered to the STROBE
(Strengthening the Reporting of Observational
Studies in Epidemiology) guidelines.
Participants
The inclusion criteria for this study were age ≥18
years, chronic non-specific LBP, and the ability
to speak and understand Chinese. Chronic non-specific
LBP was defined as pain in the lumbosacral
region, with or without sciatica, that persisted for
>3 months and lacked a clearly identifiable cause
or pathology based on clinical evaluation, imaging,
or laboratory tests. Exclusion criteria were chronic
LBP with a specific identifiable cause or pathology,
such as inflammatory diseases, tumours, infections,
fractures, structural abnormalities, or other spinal
pathologies evident on clinical evaluation, imaging,
or laboratory tests. Patients who did not provide
written informed consent, were pregnant, or were
<6 months postpartum or post-weaning were also
excluded.
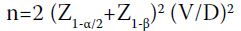
Sample size calculation
To determine the sample size for evaluating WTP,
we used the payment card elicitation format sample
size formula established by Mitchell and Carson.33
The formula is:
where n is the minimum required sample size, Z1-α/2
represents the desired confidence interval, Z1-β corresponds to the value for power, V denotes the
coefficient of variation (ie, ratio of estimated standard
deviation of WTP to estimated mean WTP), and D is
the designed effect (ie, percentage difference between
true WTP and mean of estimated WTP bids). For
this study, assuming α=0.05, β=0.20, V=0.98 (based
on a previous study evaluating WTP for reduced
pain intensity among patients with chronic pain),34
and D=0.20, the calculated minimum sample size
was 470, considering a 20% non-response rate.
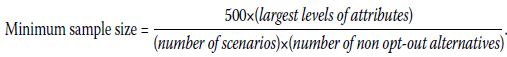
To explore preferences for MBI receipt using a
DCE design, we applied the rule of thumb described
by Orme35 and Johnson and Orme.36 The minimum
sample size required for the main effects was
calculated as follows:
Under conditions of two alternatives, a maximum of
four attribute levels and eight scenarios per patient, a
minimum of 125 patients was required. Considering
two subgroups with different characteristics and
a 20% non-response rate, the adjusted minimum
sample size was 312.
Survey data
A self-administered questionnaire was used to
collect data. An onsite research assistant invited
patients in the clinic waiting area to participate in
the survey and was available to provide assistance if
needed.
Independent variable
The independent variables of the study are as follows:
- Socio-demographic characteristics: Age, gender, education level, employment status, and personal and family income were recorded.
- General self-reported health status: A single-item self-rated health scale was used to assess participants’ self-rated health, with response options ranging from ‘Very good’ to ‘Very poor.’37 Studies have shown that this scale is associated with patients’ WTP for pain treatments.38 39 40 41
- Knowledge and usage of MBIs: Knowledge of mindfulness was assessed using two items adapted from a previous study that investigated health professionals’ and health profession students’ knowledge of and attitudes toward mindfulness.42 The items were as follows: (1) What is the extent of your knowledge of MBIs? (2) Might MBIs be useful for treating chronic pain? Usage of MBIs was determined using two items adapted from a previous study that evaluated employees’ preferences for accessing MBIs.43 The items were as follows: (1) Have you ever participated in mindfulness courses? (2) How many mindfulness sessions have you attended?
- Pain-related characteristics: Pain-related characteristics included pain duration, pain intensity, disability, and frequency of treatment for chronic LBP. Pain intensity was measured using an 11-point Numeric Rating Scale (NRS).44 Disability was assessed using the Roland-Morris Disability Questionnaire.45 Pain duration was determined by asking participants to report the number of months they had experienced an ongoing LBP problem. Frequency of treatment was evaluated by asking participants to report how many times they had consulted a doctor or other healthcare professional for LBP in the past 12 months.
- Satisfaction with current treatment: An item was adapted from a previous study that assessed treatment satisfaction in patients with osteoarthritis and LBP.46 This item asked participants to rate their satisfaction with the effectiveness of current treatment in controlling LBP.
- Monthly expenses on current treatment: Participants were asked to report their monthly expenses with respect to chronic LBP treatment.
Dependent variables
Willingness to pay and preferences for MBIs were
the two dependent variables of the current study.
The payment card method was used to assess WTP
for MBIs.47 This approach minimises starting point
bias and reduces the high rate of item non-response
relative to other elicitation methods.48 To ensure that
participants were familiar with MBIs, we provided
an introduction using a text description and a video
before each participant responded to the WTP
question (online supplementary Fig). Participants
were presented with a range of monetary values
(HK$0 to HK$10 000) and asked to select the value
that best represented the amount they would be
willing to pay for MBIs. Additionally, WTP for
pain reduction was evaluated using two items
adapted from a previous study that assessed WTP
for reductions in chronic LBP and neck pain using
the payment card method.49 These items asked
participants to indicate the amount they would be
willing and able to pay out-of-pocket per month for
their chronic LBP to be reduced by half or entirely
eliminated. Participants unwilling to pay any amount
were asked to specify their reasons.
Participants were invited to respond to
eight choice sets evaluating patient preferences
for MBIs. In each choice task, they were asked
to select their most preferred option from two
hypothetical MBIs with different attribute levels. To
ensure comprehension, we included a test scenario
with a dominant alternative. If participants did
not choose the dominant option, research staff
provided clarification. Internal validity was assessed
by including a choice set with dominant pairs, in which one alternative was clearly superior across
all attributes.
Statistical analyses
Complete-case analysis was utilised for the
dependent variable of WTP for MBIs. The Tobit
regression model was used to estimate the
associated factors.50 This model was selected
because WTP measures exhibited left-censoring
(ie, a substantial proportion of zero values [46.6%
of the sample]; the remaining responses indicated
positive WTP for MBIs). Multicollinearity was
examined using tolerance and the variance inflation
factor (VIF). Continuous variables were presented
as mean±standard deviation. The level of statistical
significance was set at 5%.51
Study design
A DCE design was used in this study to examine
the preferences of individuals with chronic LBP
for MBIs. The DCE comprised four key steps: (1)
conducting a literature review to identify conceptual
attributes and levels; (2) conducting qualitative
research to determine contextual attributes and
levels; (3) integrating attributes and levels into
choice sets, conducting pilot tests, and refining the
questionnaire; and (4) collecting experimental data
and performing data analysis.
Systematic review
A systematic review of DCEs examining patient
preferences for non-surgical treatments in chronic
musculoskeletal pain was conducted.52 Studies that
used DCEs to evaluate patient preferences for the
management of chronic musculoskeletal pain were
included.
Qualitative research
Participants with chronic LBP were invited to discuss
characteristics of MBIs they might consider valuable
when deciding whether to participate in MBIs. These
valued characteristics were summarised. A panel
of experts from relevant fields (chronic pain, DCE
methodology, and psychology) then reviewed and
refined the attributes and levels, selecting six to eight
attributes for inclusion.
Generation of choice sets, piloting, and refinement
of the questionnaire
A D-efficient experimental design was used to
generate choice sets, which were randomly assigned
to five blocks. A pilot DCE survey was conducted to
assess cognitive difficulty and questionnaire length.
Twenty patients with chronic LBP participated in the
pilot study; they provided feedback and suggestions
for improvement.
Experimental data collection and data analysis
Discrete choice experiment data were collected as
part of the cross-sectional survey. Respondents’
relative preferences were estimated using a mixed
logit model with panel specification to adjust
for correlated choices within individuals. The
coefficients of four variables—‘improvement in
capacity to perform daily life activities’, ‘risk of
adverse events’, ‘improvement in pain relief’, and
‘out-of-pocket costs’—were assumed to be random,
following a zero-bounded triangular distribution
because the distribution of these random
parameters should comprise only positive or
negative values. ‘Out-of-pocket costs’ was specified
as a continuous variable in the mixed logit model.
The marginal WTP for different levels within each
attribute was calculated through division of the
negative estimated beta coefficient for each level
by the estimated beta coefficient for ‘out-of-pocket
costs’. The log-likelihood and adjusted McFadden’s
pseudo–R-squared were calculated to assess model
goodness of fit. Higher log-likelihood and adjusted
McFadden’s pseudo–R-squared values indicate a
better-fitting model.53 54 Subgroup analyses were
conducted to assess preference heterogeneity
across characteristics, including age, gender, family
monthly income, and education.
Results
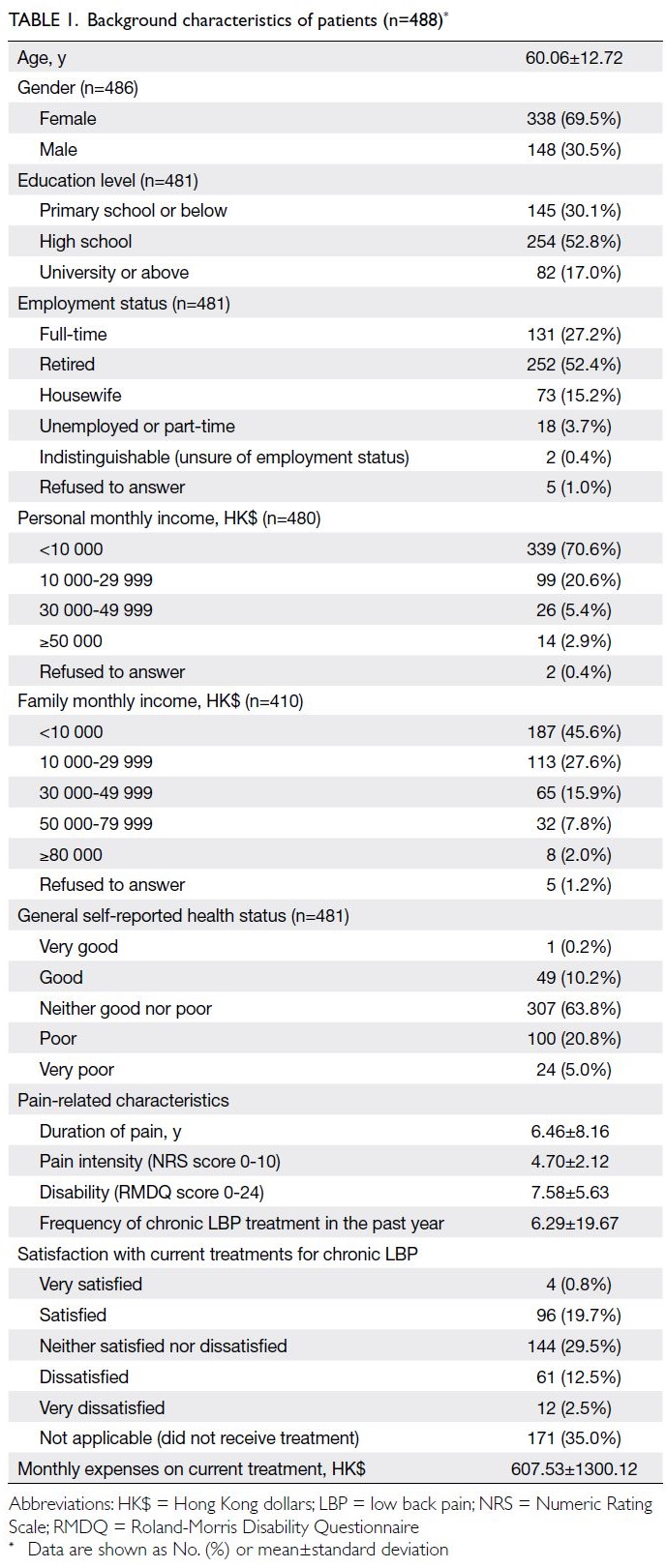
Participant characteristics
Of the 589 participants invited, 488 questionnaires
were returned, yielding a response rate of 82.9%. The
study sample had a mean age of 60.06±12.72 years;
69.5% of the participants were women. The average
pain duration was 6.46±8.16 years; mean NRS and
Roland-Morris Disability Questionnaire scores were
4.70±2.12 and 7.58±5.63, respectively. Participant
characteristics are summarised in Table 1.
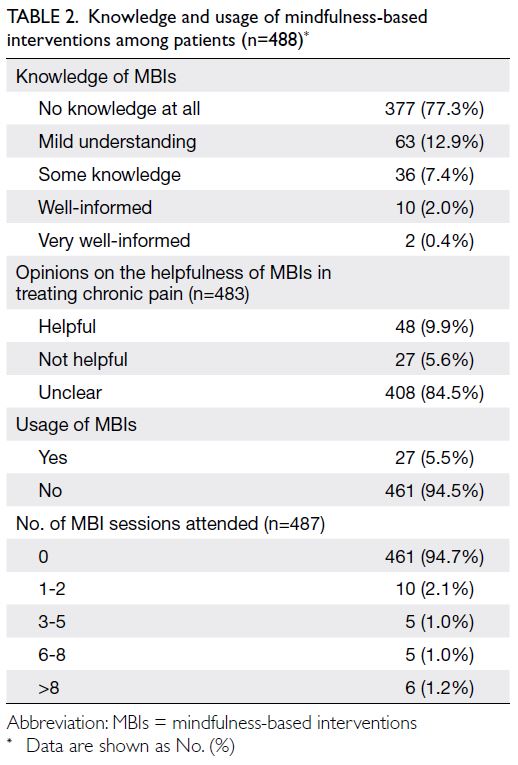
Knowledge and usage of mindfulness-based
interventions
Regarding knowledge and usage of MBIs, 77.3%
of participants were unfamiliar with MBIs, 84.5%
were uncertain about their effectiveness in treating
chronic LBP, and 94.5% had never attended an
MBI session. Knowledge and usage of MBIs are
summarised in Table 2.
Willingness to pay for pain reduction and
mindfulness-based interventions
The mean monthly WTP values for MBIs to reduce
pain by half and to entirely eliminate pain were
HK$684.68±1347.43 and HK$1102.70±1983.83,
respectively. The overall mean WTP for an eightsession
MBI programme was HK$258.75±508.11.
Among the participants, 237 were not willing to pay for MBIs, citing reasons such as limited
knowledge of MBIs, unwillingness to spend money
on treatment, lack of time, and scepticism regarding
MBI effectiveness (online supplementary Table 1).
Results of multicollinearity tests
Multicollinearity among the independent variables
was assessed; all tolerance values were >0.25 and VIF
values were <4, except for two similar variables (ie,
usage of MBIs measured as a binary variable [‘Yes’
or ‘No’] and number of MBI sessions attended).
Given that only a small number of participants had
attended MBIs, the variable measuring the number
of MBI sessions was selected for inclusion in the
Tobit regression model (online supplementary Table 2).
Factors associated with willingness to pay for
mindfulness-based interventions
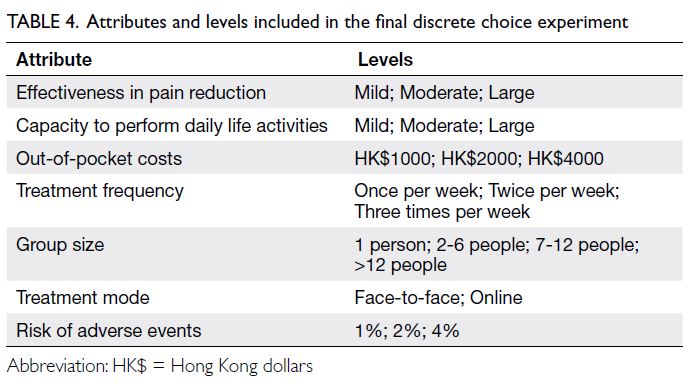
Factors associated with WTP for MBIs are
summarised in Table 3. Participants with a higher
NRS score (β=81.26; P=0.003), family monthly
income of ≥HK$30 000 (β=320.1; P=0.035), high
school education (β=242.94; P=0.045), and higher
monthly expenses on chronic LBP treatment
(β=0.11; P=0.003) were more willing to pay for MBIs.
Conversely, participants who did not believe in the
usefulness of MBIs (β=-528.88; P=0.033) were less
willing to pay for them.
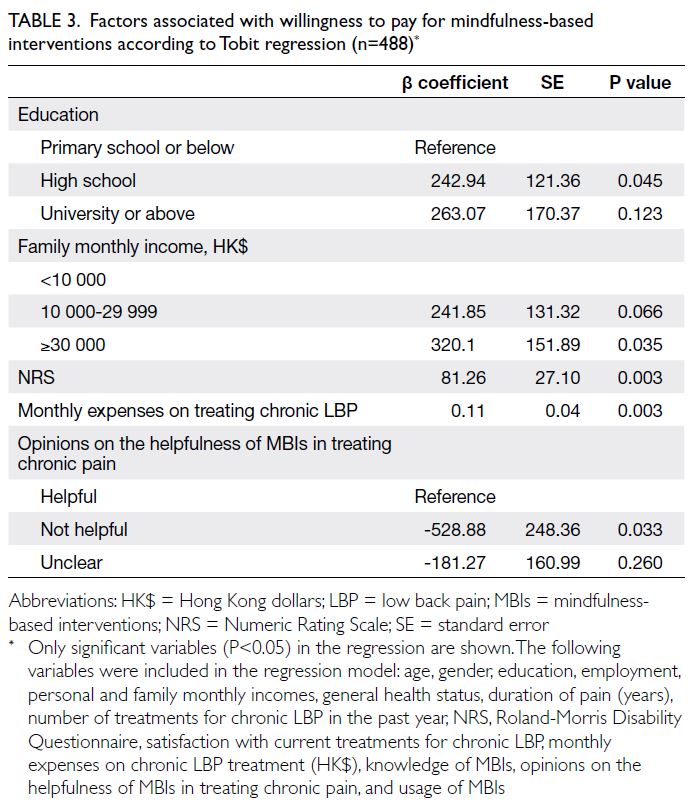
Table 3. Factors associated with willingness to pay for mindfulness-based interventions according to Tobit regression (n=488)
Evaluation of patient preferences for
mindfulness-based interventions
Conceptual attributes and levels identified
through literature review
In total, 15 eligible studies were included.52 The
attributes most frequently cited were ‘capacity to
realize daily life activities’, ‘risk of adverse events’,
‘effectiveness in pain reduction’, and ‘out-of-pocket
costs’, which were also ranked among the top three
most important attributes. Other attributes, cited
less frequently but revealing important preferences,
included ‘treatment frequency’ and ‘onset of
treatment efficacy’.52
Contextual attributes and levels identified
through qualitative research
Eight patients with chronic LBP participated in this
stage of developing contextual attributes through
patient-public involvement. Two focus group
interviews were conducted to identify contextual
attributes. Valued characteristics of MBIs were
summarised, including effectiveness in pain
reduction, mood regulation, and sleep improvement;
treatment environment; reliability of mindfulness
instructors; reputation of the organisation; safety;
affordability; flexibility (availability of online
resources at all times); availability of follow-up courses; and a group-based course format. Three
experts finalised the selection of seven attributes for
inclusion (Table 4).
Pilot study of discrete choice experiment
Only minor changes in terminology were applied to
attribute levels after the pilot study. This pilot study
verified the attributes and their levels, as presented
in Table 4. The pilot study also indicated that most patients understood the instructions and attributes.
Only minor layout adjustments were made—some
participants reported that the font size was too small.
Factors associated with patients’ preferences for
mindfulness-based interventions
After the exclusion of participants who declined
to answer DCE questions due to difficulties in
comprehension or unwillingness to respond (n=69,
14.1%) and those with missing DCE responses (n=4,
0.8%), the final participant count was reduced to 415.
Among these participants, six (1.4%) did not pass the dominance test; thus, 409 participants were included
in the analysis. The results of the DCE examining
factors associated with patients’ preferences for
MBIs are presented in Table 5. Participants were
more likely to choose MBIs with lower out-of-pocket
costs, higher levels of pain relief, and greater improvements in capacity to perform daily
life activities. Face-to-face treatment modes were
preferred over online formats. Regarding model fit,
the log-likelihood and adjusted McFadden’s pseudo–R-squared for the mixed logit model were -1502.8
and 0.330, respectively.
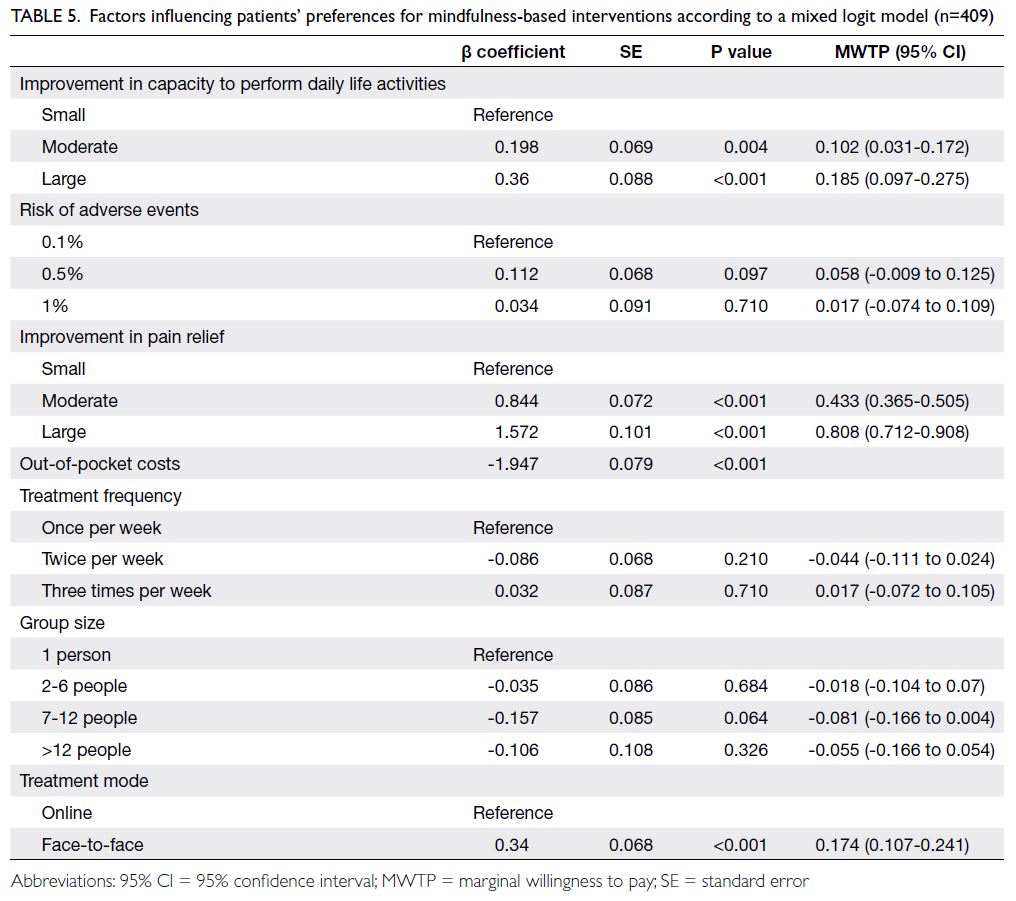
Table 5. Factors influencing patients’ preferences for mindfulness-based interventions according to a mixed logit model (n=409)
Subgroup analyses
The results of subgroup analyses are presented in
online supplementary Tables 3 to 6. Preferences
differed substantially between age-groups, family
income levels, and education levels, but showed no
gender-based significant differences. Improvement
in the capacity to perform daily life activities
was an important attribute when selecting MBIs
for older participants, those with lower family
monthly income, and those with higher education
level; this attribute was not important for younger
participants and those with higher family monthly
income and lower education level. Group size was
an important attribute for younger participants and
those with higher family monthly income but not
for older participants or those with lower family
monthly income. Younger participants and those
with higher family monthly income preferred MBIs
with a group size of one person, rather than 7 to 12
people. Treatment mode was an important attribute
for participants with lower family monthly income
and higher education level but not for those with
higher family monthly income and lower education.
Participants with lower family monthly income and
higher education preferred face-to-face treatment
over online treatment. Furthermore, participants
with lower family monthly income and older age
placed greater priority on out-of-pocket costs for
MBIs, as indicated by substantially larger regression
coefficients for out-of-pocket costs in subgroup
analyses.
Discussion
Consistent with previous studies,34 49 we found
that patients with higher pain scores, higher
family income, and higher monthly expenses on
LBP treatment were more willing to pay for MBIs.
Comparison of WTP for MBIs in this study to
a national survey on WTP for complementary
and alternative medicine treatments in England55
revealed that participants in the present study had
a lower WTP. One possible explanation for this
discrepancy is that complementary and alternative
medicine practices, such as acupuncture and herbal
medicine, are more established in some cultures;
MBIs are relatively new and may be less familiar to
our study population.
In Hong Kong’s public healthcare system,
physiotherapy and occupational therapy for chronic
pain cost HK$80 per visit. If MBIs followed this fee structure, eight sessions would cost a total of
HK$640. However, the current WTP for MBIs is
HK$258.75, approximately 40% of this cost. Notably,
WTP was calculated in a population with limited
knowledge of MBIs. Increased awareness of their
efficacy may enhance WTP, aligning it more closely
with the existing fee structure.
Our study evaluating preferences for MBIs
confirmed previous findings that chronic pain
treatment preferences are significantly influenced by
treatment effectiveness and out-of-pocket costs.52 56 57
However, in contrast to prior studies,52 56 57 we found
that the risk of adverse events was not an attribute
considered important by patients with chronic LBP
during MBI selection. One possible explanation is
that the risk of adverse events from psychological
interventions is lower and less severe than the risk
of such events associated with pharmacological
or exercise-based interventions.58 59 60 Additionally,
we observed that treatment mode constituted
an important attribute of MBIs, consistent with
investigations of exercise therapy preferences among
patients with chronic pain.39
Our study focused on assessing WTP and
preferences for MBIs in chronic LBP, following the
socio-psychobiological model that prioritises social
and psychological factors over biological factors.27 28
This approach provides insights into the socio-economic
backgrounds of patients with chronic
LBP and highlights their pain experiences and
access to pain management strategies, emphasising
the social dimension of chronic pain management.
Mindfulness-based interventions, as a psychological
and group-based approach, equip individuals with
skills to manage psychological distress related to
chronic LBP while fostering social support and
connectivity through group interaction.
The current approach to chronic pain care
often results in the underutilisation of high-value
care (eg, psychological therapies) and overuse of low-value
care, including invasive procedures and opioid
medications.4 28 The adoption and implementation
of a socio-psychobiological model could serve as an
effective strategy for establishing pain care systems
that prioritise high-value care.27 28
Despite the recognised value of MBIs in
chronic pain management, their limited integration
into clinical practice may be attributed to patients’
unfamiliarity and lack of knowledge about these
interventions, coupled with insufficient investment
in primary care resources. Additionally, economic
incentives often favour high-volume practice models
in primary care settings.28 Thus, there is an urgent
need for educational initiatives to enhance awareness
and knowledge of MBIs among individuals with
chronic LBP, as well as increased investment in
primary care resources.
This study provided critical insights into the integration of MBIs for chronic LBP management
within the Hong Kong public healthcare system. In
the context of Hong Kong’s public healthcare settings,
we propose integrating MBIs as an intermediary
step between primary care and specialist care for
chronic LBP management. Primary care providers
could identify patients experiencing psychological
and social distress who may benefit from MBIs and
facilitate their referral for MBI treatment. Patients
whose condition does not improve after an MBI
could then be referred to specialist clinics. This
approach could substantially reduce waiting times
for chronic LBP treatment within the Hong Kong
public healthcare system.
Strengths and limitations
This study has several strengths. To our knowledge,
it is the first investigation to assess WTP and
preferences for MBIs in chronic pain management;
it included a comprehensive list of independent
variables covering key factors that influence WTP.
Additionally, the study utilised a mixed logit
model to consider preference heterogeneity within
the sample. Furthermore, a rigorous systematic
review and qualitative interviews informed the
attributes and levels used in the DCE. However,
certain limitations should be acknowledged. First,
participants’ limited knowledge of MBIs may
have influenced WTP and preferences. Second,
participants were recruited through convenience
sampling from outpatient clinics in two Hong
Kong public hospitals, which may have introduced
selection bias that skewed the sample composition
and limited its representativeness. This limitation
may affect the generalisability of the findings beyond
the specific group sampled. Third, the cross-sectional
design of the study precluded establishment of
causal relationships between WTP and preferences
for MBIs, as well as associated factors.
Although WTP and preferences are essential
considerations for MBI implementation, they
should not be the sole determinants. Factors such
as cost-effectiveness, impact on quality of life, and
infrastructure availability must also be considered.
Further research is required to provide additional
evidence for implementation within the Hong
Kong public healthcare system. Nevertheless, this
study established a rationale for assessing WTP
and preferences for MBIs, with a methodology that
can be adapted for healthcare evaluations in other
countries.
Conclusion
This study highlights the need to increase awareness
of MBIs for chronic LBP management within the
public healthcare system. The findings indicate
low WTP among participants, suggesting a gap in understanding and utilisation. Notably, individuals
with higher pain scores, higher family income, and
higher monthly LBP treatment expenses, as well as
a stronger belief in MBIs, were more willing to pay
for such interventions; these observations indicate
targeted demand. Patient preferences favoured
lower costs, face-to-face treatment, and enhanced
effectiveness. These findings provide practical
insights for designing patient preference–aligned
MBIs and will serve as valuable references for future
healthcare evaluations.
Author contributions
Concept or design: M Zhu, PKH Mo, RWS Sit.
Acquisition of data: M Zhu.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: M Zhu.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: M Zhu.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: M Zhu.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
As an editor of the journal, RWS Sit was not involved in the
peer review process. Other authors have disclosed no conflicts
of interest.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This research was approved by the Joint Chinese University of
Hong Kong–New Territories East Cluster Clinical Research
Ethics Committee, Hong Kong (Ref. No.: 2022.279). The
research was conducted in accordance with the Declaration of
Helsinki. All participants provided written informed consent
before completing the questionnaire.
Data availability
The datasets generated during and/or analysed during
the current study are not publicly available due to ethics
restrictions. A request for the code can be made directly to
the corresponding author.
Supplementary material
The supplementary material was provided by the authors and
some information may not have been peer reviewed. Accepted
supplementary material will be published as submitted by the
authors, without any editing or formatting. Any opinions
or recommendations discussed are solely those of the
author(s) and are not endorsed by the Hong Kong Academy
of Medicine and the Hong Kong Medical Association.
The Hong Kong Academy of Medicine and the Hong Kong
Medical Association disclaim all liability and responsibility
arising from any reliance placed on the content.
References
1. Hoy D, March L, Brooks P, et al. The global burden of low
back pain: estimates from the Global Burden of Disease
2010 study. Ann Rheum Dis 2014;73:968-74. Crossref
2. Dieleman JL, Cao J, Chapin A, et al. US health care
spending by payer and health condition, 1996-2016. JAMA
2020;323:863-84. Crossref
3. Hong J, Reed C, Novick D, Happich M. Costs associated
with treatment of chronic low back pain: an analysis of the
UK General Practice Research Database. Spine (Phila Pa
1976) 2013;38:75-82. Crossref
4. Foster NE, Anema JR, Cherkin D, et al. Prevention and
treatment of low back pain: evidence, challenges, and
promising directions. Lancet 2018;391:2368-83. Crossref
5. Anheyer D, Haller H, Barth J, Lauche R, Dobos G, Cramer H.
Mindfulness-based stress reduction for treating low back
pain: a systematic review and meta-analysis. Ann Intern
Med 2017;166:799-807. Crossref
6. Herman PM, Anderson ML, Sherman KJ, Balderson BH,
Turner JA, Cherkin DC. Cost-effectiveness of mindfulness-based
stress reduction versus cognitive behavioral therapy
or usual care among adults with chronic low back pain.
Spine (Phila Pa 1976) 2017;42:1511-20. Crossref
7. Pérez-Aranda A, D’Amico F, Feliu-Soler A, et al. Cost-utility
of mindfulness-based stress reduction for fibromyalgia
versus a multicomponent intervention and usual care:
a 12-month randomized controlled trial (EUDAIMON
study). J Clin Med 2019;8:1068. Crossref
8. Day MA, Jensen MP, Ehde DM, Thorn BE. Toward
a theoretical model for mindfulness-based pain
management. J Pain 2014;15:691-703. Crossref
9. Ehde DM, Dillworth TM, Turner JA. Cognitive-behavioral
therapy for individuals with chronic pain: efficacy,
innovations, and directions for research. Am Psychol
2014;69:153-66. Crossref
10. Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J.
Acceptance and commitment therapy: model, processes
and outcomes. Behav Res Ther 2006;44:1-25. Crossref
11. Zhang D, Lee EK, Mak EC, Ho CY, Wong SY. Mindfulness-based
interventions: an overall review. Br Med Bull
2021;138:41-57. Crossref
12. Khoo EL, Small R, Cheng W, et al. Comparative evaluation
of group-based mindfulness-based stress reduction
and cognitive behavioural therapy for the treatment
and management of chronic pain: a systematic review
and network meta-analysis. Evid Based Ment Health
2019;22:26-35. Crossref
13. Liu Z, Jia Y, Li M, et al. Effectiveness of online mindfulness-based
interventions for improving mental health in
patients with physical health conditions: systematic review
and meta-analysis. Arch Psychiatr Nurs 2022;37:52-60. Crossref
14. Khusid MA, Vythilingam M. The emerging role of
mindfulness meditation as effective self-management
strategy, part 2: clinical implications for chronic pain,
substance misuse, and insomnia. Mil Med 2016;181:969-75. Crossref
15. Veehof MM, Trompetter HR, Bohlmeijer ET, Schreurs KM.
Acceptance- and mindfulness-based interventions for the
treatment of chronic pain: a meta-analytic review. Cogn
Behav Ther 2016;45:5-31. Crossref
16. Hughes LS, Clark J, Colclough JA, Dale E, McMillan D.
Acceptance and commitment therapy (ACT) for chronic
pain: a systematic review and meta-analyses. Clin J Pain 2017;33:552-68. Crossref
17. Gryesten JR, Poulsen S, Moltu C, Biering EB, Møller K,
Arnfred SM. Patients’ and therapists’ experiences of
standardized group cognitive behavioral therapy: needs
for a personalized approach. Adm Policy Ment Health
2024;51:617-33. Crossref
18. Zhang L, Lopes S, Lavelle T, et al. Economic evaluations
of mindfulness-based interventions: a systematic review.
Mindfulness (N Y) 2022;13:2359-78. Crossref
19. Census and Statistics Department, Hong Kong SAR
Government. Thematic Household Survey Report No.
50. Jan 2013. Available from: https://www.statistics.gov.hk/pub/B11302502013XXXXB0100.pdf. Accessed 7 Apr 2025.
20. Health Bureau, Hong Kong SAR Government. The
healthcare challenges in Hong Kong. 2022. Available
from: https://www.primaryhealthcare.gov.hk/bp/en/supplementary-documents/challenges/. Accessed 18 Mar 2025.
21. Abbas SM, Usmani A, Imran M. Willingness to pay and its
role in health economics. JBUMDC 2019;9:62-6.
22. Liu S, Yam CH, Huang OH, Griffiths SM. Willingness to
pay for private primary care services in Hong Kong: are
elderly ready to move from the public sector? Health Policy
Plan 2013;28:717-29. Crossref
23. Krist AH, Tong ST, Aycock RA, Longo DR. Engaging
patients in decision-making and behavior change to
promote prevention. Stud Health Technol Inform
2017;240:284-302. Crossref
24. Ostermann J, Brown DS, de Bekker-Grob EW,
Mühlbacher AC, Reed SD. Preferences for health
interventions: improving uptake, adherence, and efficiency.
Patient 2017;10:511-4. Crossref
25. Alhowimel A, AlOtaibi M, Radford K, Coulson N.
Psychosocial factors associated with change in pain and
disability outcomes in chronic low back pain patients
treated by physiotherapist: a systematic review. SAGE
Open Med 2018;6:2050312118757387. Crossref
26. Karran EL, Grant AR, Moseley GL. Low back pain and
the social determinants of health: a systematic review and
narrative synthesis. Pain 2020;161:2476-93. Crossref
27. Carr DB, Bradshaw YS. Time to flip the pain curriculum?
Anesthesiology 2014;120:12-4. Crossref
28. Mardian AS, Hanson ER, Villarroel L, et al. Flipping the
pain care model: a sociopsychobiological approach to
high-value chronic pain care. Pain Med 2020;21:1168-80. Crossref
29. Allen-Watts K, Sims AM, Buchanan TL, et al.
Sociodemographic differences in pain medication
usage and healthcare provider utilization among adults
with chronic low back pain. Front Pain Res (Lausanne)
2022;2:806310. Crossref
30. Majeed MH, Ali AA, Sudak DM. Mindfulness-based
interventions for chronic pain: evidence and applications.
Asian J Psychiatr 2018;32:79-83. Crossref
31. Smith SL, Langen WH. A systematic review of mindfulness
practices for improving outcomes in chronic low back pain.
Int J Yoga 2020;13:177-82. Crossref
32. Petrucci G, Papalia GF, Russo F, et al. Psychological
approaches for the integrative care of chronic low back
pain: a systematic review and metanalysis. Int J Environ
Res Public Health 2021;19:60. Crossref
33. Mitchell RC, Carson RT. Using Surveys to Value Public
Goods: The Contingent Valuation Method. New York and London: Resources for the Future; 1989.
34. Chuck A, Adamowicz W, Jacobs P, Ohinmaa A, Dick B,
Rashiq S. The willingness to pay for reducing pain and
pain-related disability. Value Health 2009;12:498-506. Crossref
35. Orme BK. Sample size issues for conjoint analysis studies.
In: Orme BK, editor. Getting Started with Conjoint
Analysis: Strategies for Product Design and Pricing
Research. 4th ed. Madison [WI]: Research Publishers LLC;
1998: 57-65.
36. Johnson R, Orme B. Sawtooth Software Research Paper
Series. Getting the most from CBC. WA: Sawtooth
Software; 2003. Available from: https://sawtoothsoftware.com/resources/technical-papers/getting-the-most-from-cbc. Accessed 24 Mar 2025.
37. Hanmer J. Measuring population health: association
of self-rated health and PROMIS measures with social
determinants of health in a cross-sectional survey of the
US population. Health Qual Life Outcomes 2021;19:221. Crossref
38. Copsey B, Buchanan J, Fitzpatrick R, Lamb SE, Dutton SJ,
Cook JA. Duration of treatment effect should be considered
in the design and interpretation of clinical trials: results
of a discrete choice experiment. Med Decis Making
2019;39:461-73. Crossref
39. Cranen K, Groothuis-Oudshoorn CG, Vollenbroek-Hutten MM, IJzerman MJ. Toward patient-centered
telerehabilitation design: understanding chronic
pain patients’ preferences for web-based exercise
telerehabilitation using a discrete choice experiment. J
Med Internet Res 2017;19:e26. Crossref
40. Ferreira GE, Howard K, Zadro JR, O’Keeffe M, Lin CC,
Maher CG. People considering exercise to prevent low
back pain recurrence prefer exercise programs that differ
from programs known to be effective: a discrete choice
experiment. J Physiother 2020;66:249-55. Crossref
41. Laba TL, Brien JA, Fransen M, Jan S. Patient preferences
for adherence to treatment for osteoarthritis: the
MEdication Decisions in Osteoarthritis Study (MEDOS).
BMC Musculoskelet Disord 2013;14:160. Crossref
42. McKenzie SP, Hassed CS, Gear JL. Medical and psychology
students’ knowledge of and attitudes towards mindfulness
as a clinical intervention. Explore (NY) 2012;8:360-7. Crossref
43. Lau MA, Colley L, Willett BR, Lynd LD. Employee’s
preferences for access to mindfulness-based cognitive
therapy to reduce the risk of depressive relapse—a discrete
choice experiment. Mindfulness 2012;3:318-26. Crossref
44. Atisook R, Euasobhon P, Saengsanon A, Jensen MP.
Validity and utility of four pain intensity measures for use
in international research. J Pain Res 2021;14:1129-39. Crossref
45. Yamato TP, Maher CG, Saragiotto BT, Catley MJ,
McAuley JH. The Roland-Morris Disability Questionnaire:
one or more dimensions? Eur Spine J 2017;26:301-8. Crossref
46. Turk D, Boeri M, Abraham L, et al. Patient preferences for
osteoarthritis pain and chronic low back pain treatments
in the United States: a discrete-choice experiment.
Osteoarthritis Cartilage 2020;28:1202-13. Crossref
47. Tian X, Yu X, Holst R. Applying the payment card approach
to estimate the WTP for green food in China. In: IAMO
Forum 2011; 2011 Jun 23-24; Halle, Germany; 2011: No.23.
48. Soeteman L, van Exel J, Bobinac A. The impact of the
design of payment scales on the willingness to pay for
health gains. Eur J Health Econ 2017;18:743-60. Crossref
49. Herman PM, Luoto JE, Kommareddi M, Sorbero ME,
Coulter ID. Patient willingness to pay for reductions
in chronic low back pain and chronic neck pain. J Pain
2019;20:1317-27. Crossref
50. Pavel MS, Chakrabarty S, Gow J. Assessing willingness to
pay for health care quality improvements. BMC Health
Serv Res 2015;15:43. Crossref
51. Kanter G, Komesu Y, Qaedan F, Rogers R. 5: Mindfulness-based
stress reduction as a novel treatment for interstitial
cystitis/bladder pain syndrome: a randomized controlled
trial [abstract]. Am J Obstet Gynecol 2016;214(4 Suppl
1):S457-8. Crossref
52. Zhu M, Dong D, Lo HH, Wong SY, Mo PK, Sit RW. Patient
preferences in the treatment of chronic musculoskeletal
pain: a systematic review of discrete choice experiments.
Pain 2023;164:675-89. Crossref
53. UCLA: Statistical Consulting Group. FAQ: How are the
likelihood ratio, wald, and lagrange multiplier (score) tests
different and/or similar? Available from: https://stats.oarc.ucla.edu/other/mult-pkg/faq/general/faqhow-are-the-likelihood-ratio-wald-and-lagrange-multiplier-score-tests-different-andor-similar/#:~:text=The%20log%20likelihood%20(i.e.%2C%20the,model%20with%20a%20likelihood%20function . Accessed 12 May 2024.
54. Hu B, Shao J, Palta M. PSEUDO-R 2 in logistic regression
model. Stat Sin 2006;16:847-60.
55. Sharp D, Lorenc A, Morris R, et al. Complementary
medicine use, views, and experiences: a national survey in
England. BJGP Open 2018;2:bjgpopen18X101614. Crossref
56. Al-Omari B, McMeekin P, Bate A. Systematic review of
studies using conjoint analysis techniques to investigate
patients’ preferences regarding osteoarthritis treatment.
Patient Prefer Adherence 2021;15:197-211. Crossref
57. Poder TG, Beffarat M. Attributes underlying non-surgical
treatment choice for people with low back pain: a
systematic mixed studies review. Int J Health Policy Manag
2021;10:201-10. Crossref
58. Ho EK, Chen L, Simic M, et al. Psychological interventions
for chronic, non-specific low back pain: systematic review
with network meta-analysis. BMJ 2022;376:e067718. Crossref
59. Els C, Jackson TD, Kunyk D, et al. Adverse events
associated with medium- and long-term use of opioids
for chronic non-cancer pain: an overview of Cochrane
Reviews. Cochrane Database Syst Rev 2017;10:CD012509. Crossref
60. Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA,
Smith BH. Physical activity and exercise for chronic pain
in adults: an overview of Cochrane Reviews. Cochrane
Database Syst Rev 2017;4:CD011279. Crossref