Hong Kong Med J 2024;30:Epub 5 Dec 2024
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Incidence of 30-day readmission after total knee
arthroplasty and its associated factors in Hong Kong
Omar WK Tsui1; PK Chan, FHKAM (Orthopaedic Surgery), FHKCOS2; Jeffery HY Leung, BSc2; Amy Cheung, FHKAM (Orthopaedic Surgery), FHKCOS3; Vincent WK Chan, FHKAM (Orthopaedic Surgery), FHKCOS3; Michelle Hilda Luk, FHKAM (Orthopaedic Surgery), FHKCOS3; MH Cheung, FHKAM (Orthopaedic Surgery), FHKCOS2; Henry Fu, FHKAM (Orthopaedic Surgery), FHKCOS2; KY Chiu, FHKAM (Orthopaedic Surgery), FHKCOS2
1 Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong SAR, China
2 Department of Orthopaedics and Traumatology, School of Clinical Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong SAR, China
3 Department of Orthopaedics and Traumatology, Queen Mary Hospital, Hong Kong SAR, China
Corresponding author: Dr PK Chan (lewis@ortho.hku.hk)
Abstract
Introduction: Total knee arthroplasty (TKA) is
one of the most commonly performed orthopaedic
procedures worldwide, due to the increased
prevalence of osteoarthritis associated with an
ageing global population. Although many studies
have focused on the causes of readmission among
TKA patients within 30 days post-surgery, none
have been conducted in Hong Kong. This study
investigated the 30-day readmission rate, causes, and
risk factors among TKA patients in Hong Kong.
Methods: This retrospective review included
patients who underwent TKA at a local university-affiliated
hospital between 2001 and 2020. Eligible
patients were identified using the Clinical Data
Analysis and Reporting System and electronic patient
records. Their data were analysed to determine the
30-day readmission rate, risk factors, and underlying causes.
Results: Among the 3827 TKA patients included,
the male-to-female ratio was 1:2.78 (1012:2815) and
the mean age (±standard deviation) was 71.11±8.82
years. Of these patients, 3.4% underwent unplanned
readmission to hospitals through the Accident and
Emergency Department within 30 days of TKA. The
most common causes of readmission were knee pain
(33.1%), knee swelling (26.2%), and gastrointestinal-related
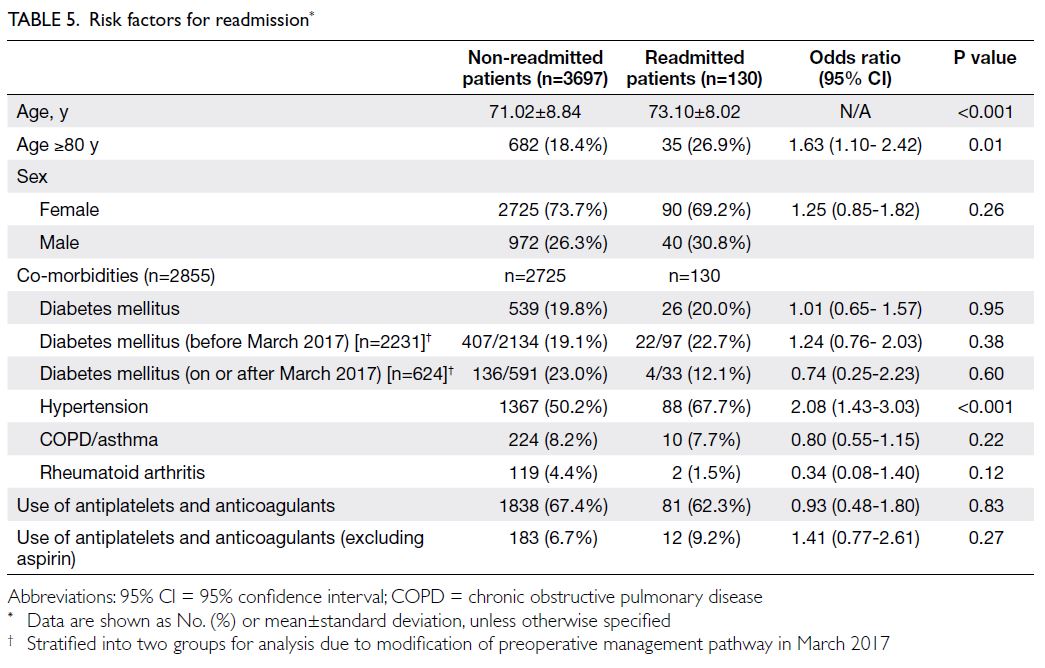
conditions (8.5%). Age ≥80 years (odds ratio
[OR]=1.63; P=0.01) and hypertension (OR=2.08;
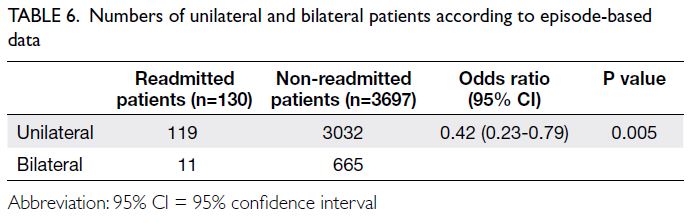
P<0.001) were risk factors for readmission. Bilateral simultaneous TKA (OR=0.42; P=0.005) was
associated with lower risk of readmission.
Conclusion: The readmission rate in this study
was 3.4%, comparable to rates in previous reports.
Enhanced patient education and optimised
perioperative pain management are needed to
minimise hospital readmissions. Fall prevention,
cautious painkiller prescribing, and improved nursing
care are recommended to prevent readmission.
New knowledge added by this study
- Pain (33.1%) and swelling (26.2%) are the most common causes of readmission after total knee arthroplasty (TKA) in Hong Kong.
- Age ≥80 years and hypertension are major risk factors for readmission, whereas simultaneous bilateral TKA is associated with a lower risk of readmission.
- The male-to-female ratio is 1:2.78 in Hong Kong, which is lower than the ratio in other countries.
- Pain management and education should be enhanced.
- Fall prevention, cautious painkiller prescribing, and improved nursing care are recommended.
Introduction
Due to the increasing incidence of osteoarthritis
associated with the ageing global population, total
knee arthroplasty (TKA) has become one of the
most commonly performed orthopaedic procedures worldwide. The most common approach to
determine causes and risk factors involves analysing
readmission episodes among TKA patients within
30 days post-surgery.1 2 The 30-day readmission
rate provides insight into the prevalence of postoperative complications, whereas the length of
stay after readmission reflects the severity of those
complications. A review of readmission causes is
needed to assess the quality of hospital care and
determine the adequacy of patient education (eg,
wound management).3 An understanding of the
30-day readmission rate, causes, and risk factors
can help hospitals improve clinical guidelines,
reduce medical and surgical complications,4 and
reduce the financial burden of treatment for these
complications.5
Although multiple studies worldwide have
adequately explored the 30-day readmission causes,
rate, and length of stay among TKA patients,6 7
revealing important clinical insights, no such studies
have been conducted in Hong Kong. The current
study aimed to investigate the 30-day readmission
rate, causes, and risk factors among TKA patients in
the city.
Methods
This retrospective study included all patients who
underwent TKA at our local university-affiliated
hospital and were readmitted through an Accident
and Emergency Department (AED) between
2001 and 2020. It evaluated the epidemiological
characteristics, readmission causes, and preoperative co-morbidities of TKA patients.
We utilised data from the Clinical Data Analysis
and Reporting System (CDARS), a well-established
platform developed by the Hospital Authority
(HA). The CDARS contains patient data, such as
laboratory reports and radiological images; it covers
all outpatients and inpatients at 43 public hospitals
and institutions across seven service clusters in Hong
Kong. Records in the CDARS include the details of
patients with unplanned 30-day readmission to the
AED of an HA hospital from either their homes or
rehabilitation facilities, along with their discharge
information. This platform is extensively used by
research teams across Hong Kong.8 We obtained
a list of TKA patients who underwent surgery at
the study hospital and were readmitted to an HA
hospital within 30 days. We matched these patient
names with their corresponding electronic patient
records to determine the reasons for readmission.
For patients who experienced 30-day
readmission, both the records in the CDARS and
electronic patient records were reviewed. For
patients who did not require 30-day readmission,
only CDARS records were reviewed. Medication
records (ie, dispensing dates, dosages, and durations)
were extracted from CDARS records to identify co-morbidities
(online supplementary Appendix). All
patient data were de-identified.
Based on factors described by Roger et al,6
we classified reasons for readmission into the
following categories: orthopaedics-related, surgery-related,
gastrointestinal-related, urological-related,
neurological-related, cardiac-related, respiratory-related,
renal-related, medication-related, and
others. Orthopaedic specialists performed the
classification to determine the cause of readmission.
The inclusion criteria were a recent history
of TKA at our institution, readmission through the
AED of an HA hospital, and inpatient admission.
The exclusion criteria were a history of knee
surgery, incomplete clinical assessment data, and/or orthopaedic tumours in the knee (for paediatric patients only).
Analyses of readmission cause, number, and
rate, as well as organ dysfunction episodes, were
episode-based. The analysis of risk factors for
readmission was patient-based. Risk factors/co-morbidities
were identified based on medications
prescribed to the patients. If a patient received
antihypertensive medication, that patient was
assumed to have hypertension.
Data analysis was performed using R (R
Foundation for Statistical Computing, Vienna,
Austria) and R Studio software. All statistical tests
were two-sided, and a 5% significance threshold
was applied. The investigators and their research
assistants were responsible for data collection and
had access to the source data and study records. To evaluate categorical variables, Chi squared tests and/or Fisher’s exact tests were conducted, depending on the observed frequencies. To evaluate continuous
variables, the Kruskal–Wallis test was used.
Results
In total, 3878 records were initially reviewed; of these,
43 were excluded due to the presence of tumours (ie,
osteosarcoma in the distal tibia), three were excluded
due to incorrect data entry for revision surgery,
and five were excluded because they constituted
duplicate entries for the same readmission episode
(online supplementary Fig 1).
Basic demographic data
Of the 3827 valid patient records, 2855 were
included in the initial analysis after removal of
duplicate records for 972 patients who underwent
two unilateral TKAs during different admission
episodes. Of the 3827 patients, 2815 (73.6%) were
women and 1012 (26.4%) were men. The mean ages
were 71.11 years for TKA patients who did not
experience readmission and 73.10 years for TKA
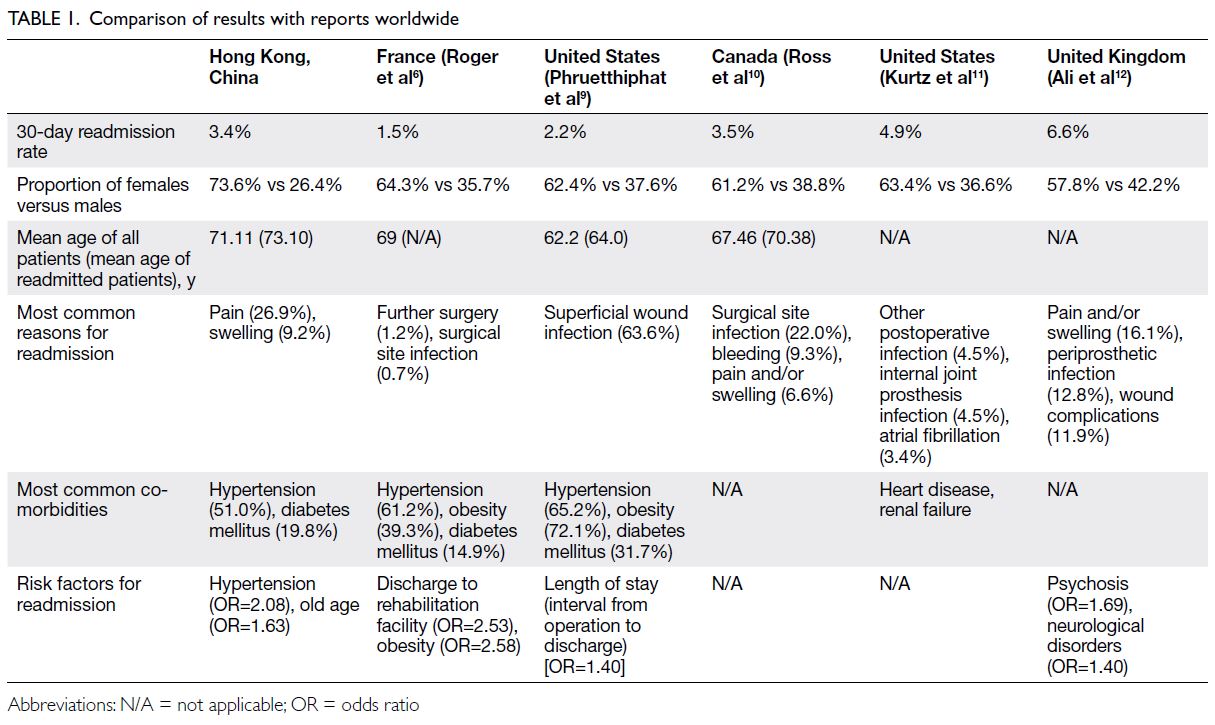
patients who experienced readmission (Table 16 9 10 11 12).
The mean postoperative length of stay (±standard
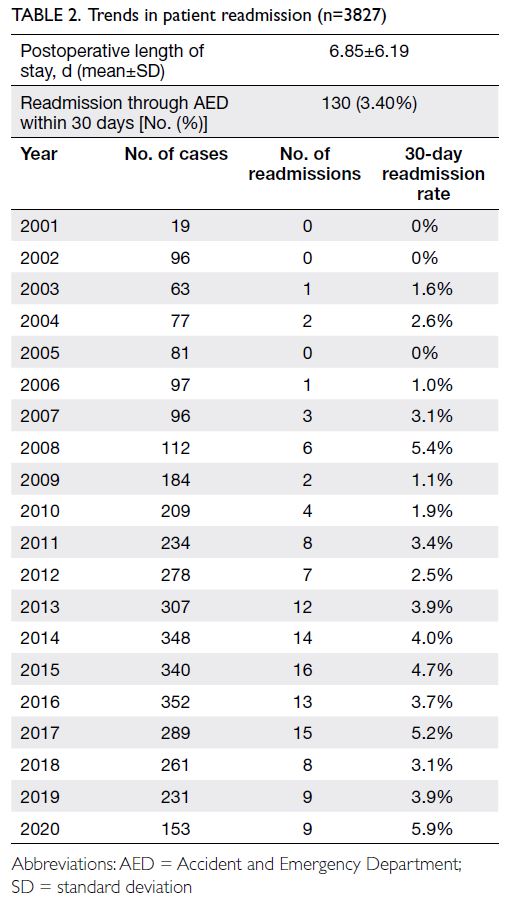
deviation) was 6.85±6.19 days (Table 2). Thus, the
readmission rate at our institution was 3.4%, similar
to rates reported worldwide (Table 1).6 7 13 There was an increase in the 30-day readmission rate between 2001 and 2020 (Table 2). The number of TKAs
performed in our institution increased from 2001
to 2014 and remained consistently high (>200 TKAs
annually except in 2020) [online supplementary Fig 2], in line with published literature.14
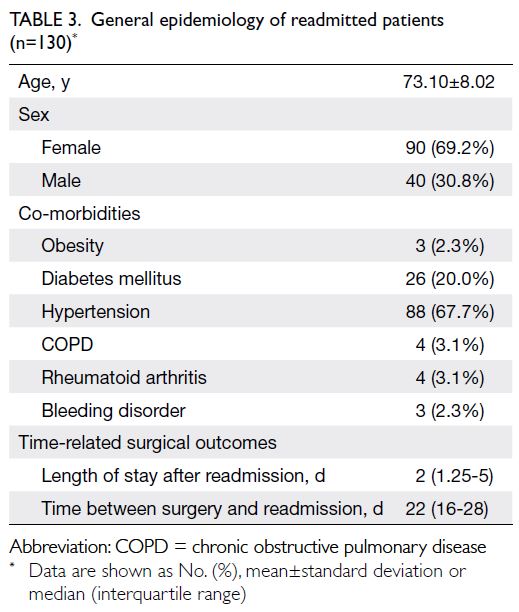
In total, 130 patients with valid readmission
records were analysed to identify causes and risk
factors (online supplementary Fig 1). Of these
patients, 90 (69.2%) were women and 40 (30.8%) were
men. The median length of stay after readmission
was 2 days (interquartile range=1.25-5) and the
mean time between surgery and readmission was 22
days (Table 3).
Causes of readmission and associated risk
factors
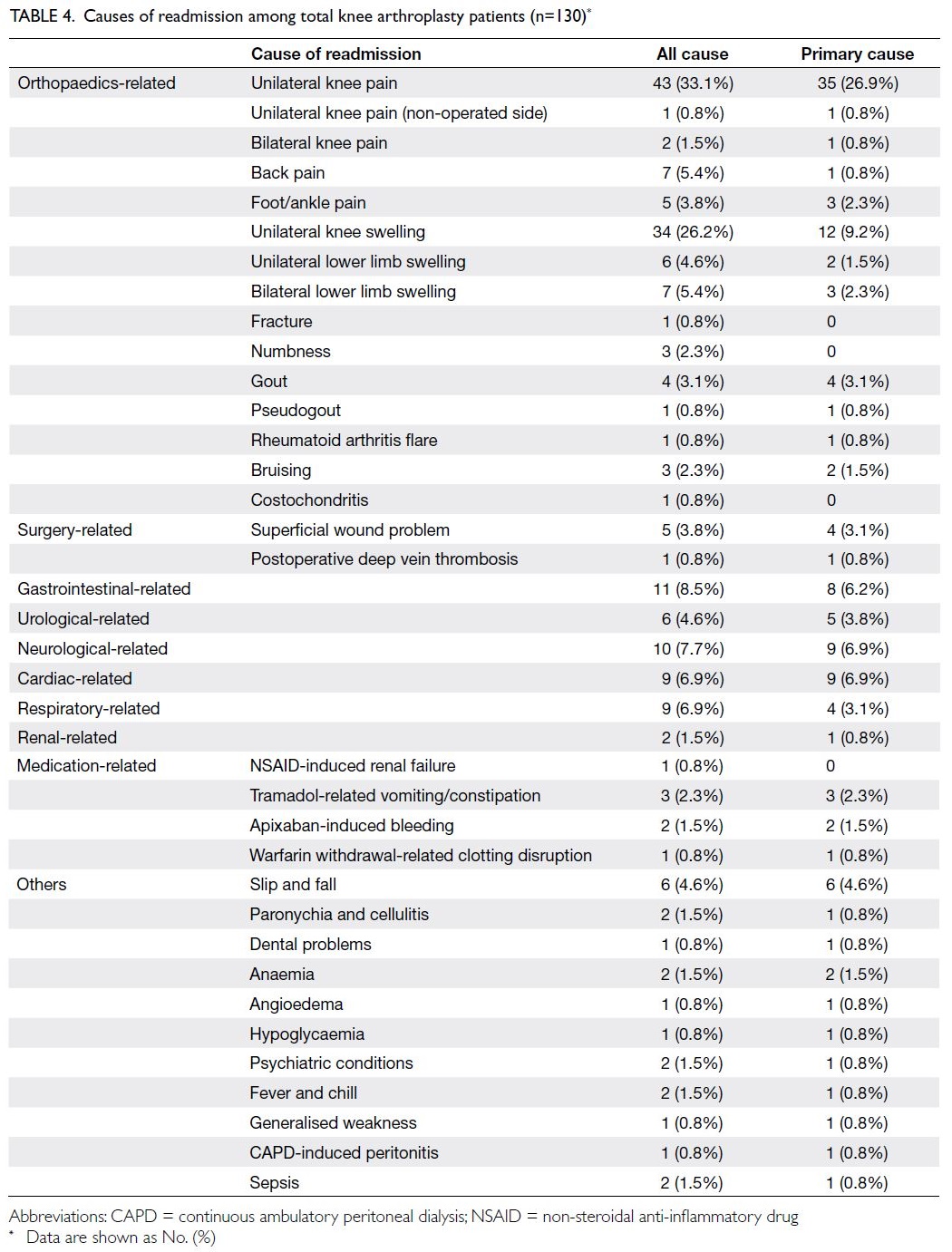
Unilateral knee pain (33.1%), unilateral knee
swelling (26.2%), and gastrointestinal-related
conditions (8.5%) were the most common causes
of readmission (Table 4). Hypertension (67.7%) and
diabetes mellitus (22.7% before March 2017 from
which our institution modified the preoperative
management pathway) were the most common
co-morbidities among readmitted patients.
Additionally, hypertension (odds ratio [OR]=2.08;
P<0.001) and age ≥80 years (OR=1.63; P=0.01) were
identified as significant risk factors for readmission (Table 5 and online supplementary Table 1). Patients
who underwent bilateral TKA had a 58% lower risk
of readmission (Table 6), possibly because they had
better health condition before surgery and received
more rigorous preoperative screening for high-risk
co-morbidities.
Discussion
Our results suggest that there is a substantial rate of
readmission due to pain and swelling among TKA
patients in Hong Kong, which is higher than the rates
in previous studies (Table 1).6 9 12 Hospital resources
should be reviewed to determine whether these
patients require admission because most readmitted
patients have non-severe conditions. To reduce
the unnecessary allocation of clinical resources to
non-severe cases, alternatives such as designated
nurse clinics15 and patient consultation hotlines
can provide medical advice for managing minor
conditions (eg, pain and swelling) at home. These
measures can reduce the workload of orthopaedic
surgeons and improve postoperative follow-up care.
Hypertension and age ≥80 years were significant
risk factors for readmission. The mean age of TKA
patients in Hong Kong was higher than the mean
ages of TKA patients in similar studies worldwide
(Table 1)6 9 10 11 12; this difference aligns with the fact that
Hong Kong has the longest life expectancy globally
(mean age of 85.16 years in 2022).16
The increased risk of readmission with old age,
consistent with findings in a previous study,17 may be
related to the greater likelihood for older individuals
to visit the AED for non-orthopaedic issues. In
contrast, patients who underwent simultaneous
bilateral TKA had a lower risk of readmission
(OR=0.42; P=0.005) [Table 6].
At our institution, patients who underwent
simultaneous bilateral TKA were aged <75 years
and had no clinically significant cardiovascular co-morbidities
(eg, stroke). Furthermore, in March
2017, our institution introduced routine glycated
haemoglobin screening to identify diabetic and
prediabetic patients, with the goal of minimising
postoperative complications. Diabetes mellitus is
known to increase the risk of periprosthetic joint
infection after surgery.18 Patients with elevated
glycated haemoglobin levels were referred to
endocrinologists for better management of diabetes
mellitus prior to TKA, thereby decreasing the
OR for readmission from 1.24 to 0.74 (Table 5
and online supplementary Table 1). Considering
that a substantial number of patients with the
aforementioned co-morbidities exhibit a higher risk
of readmission, the perioperative protocol could be
improved. Suggested changes could include better
coordination with each patient’s family medicine
specialists or general practitioners, who usually have
a better understanding of the patient’s underlying medical conditions, to develop effective preoperative and postoperative care plans.
Overall, 4.6% (n=6) of the patients were
readmitted primarily due to falls (Table 4).
This finding highlights the need for enhanced nursing support and education to prevent post-surgical
falls among TKA patients. Furthermore,
stronger occupational therapy and household aid
programmes can help prevent falls at home and
improve patient rehabilitation. Another 4.6% of patients were readmitted due to the adverse drug
effects (Table 4 and online supplementary Table 2),
particularly from tramadol/codeine/morphine and
related medications; symptoms included vomiting
and constipation. These results indicate a need for
cautious painkiller prescribing to prevent future
medication-related readmissions.
Strengths and limitations
To the best of our knowledge, this is the first study
on the readmission rate, causes, and risk factors
among TKA patients within 30 days post-surgery.
It also compared data collected in Hong Kong with
results from other studies, yielding insights for
local orthopaedic surgeons who seek to improve
suboptimal surgical outcomes.
Notably, there were some limitations. Patient
data in the CDARS may be incomplete because
some doctors might have omitted the International Classification of Diseases, Ninth Revision codes
for certain co-morbidities. To mitigate this issue,
prescribed drugs were used to identify patients’
co-morbidities. However, this approach may have
missed some patients with co-morbidities and no
associated medication records.
Conclusion
This study showed that older TKA patients with
hypertension were more likely to be readmitted
through the AED within 30 days post-surgery. The
most common reasons for readmission were pain,
swelling, and gastrointestinal-related symptoms. To
reduce readmissions, hospitals should place greater
emphasis on pain and wound management for TKA
patients. Furthermore, patient education efforts
should be strengthened to increase awareness of
pain and wound management.
Author contributions
Concept or design: OWK Tsui, PK Chan.
Acquisition of data: OWK Tsui, PK Chan, JHY Leung.
Analysis or interpretation of data: OWK Tsui, PK Chan, JHY Leung.
Drafting of the manuscript: OWK Tsui.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: OWK Tsui, PK Chan, JHY Leung.
Analysis or interpretation of data: OWK Tsui, PK Chan, JHY Leung.
Drafting of the manuscript: OWK Tsui.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Declaration
The research was presented at 42nd Annual Congress of the Hong Kong Orthopaedic Association, 5 November 2022,
Hong Kong.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This research was approved by the Institutional Review Board
of The University of Hong Kong/Hospital Authority Hong
Kong West Cluster, Hong Kong (Ref No.: UW-22-313). The
requirement for patient consent was waived by the Board due
to the retrospective nature of the research.
Supplementary material
The supplementary material was provided by the authors and
some information may not have been peer reviewed. Accepted
supplementary material will be published as submitted by the
authors, without any editing or formatting. Any opinions
or recommendations discussed are solely those of the
author(s) and are not endorsed by the Hong Kong Academy
of Medicine and the Hong Kong Medical Association.
The Hong Kong Academy of Medicine and the Hong Kong
Medical Association disclaim all liability and responsibility
arising from any reliance placed on the content.
References
1. Howie CM, Mears SC, Barnes CL, Stambough JB.
Readmission, complication, and disposition calculators in
total joint arthroplasty: a systemic review. J Arthroplasty
2021;36:1823-31. Crossref
2. D’Apuzzo M, Westrich G, Hidaka C, Jung Pan T, Lyman S.
All-cause versus complication-specific readmission
following total knee arthroplasty. J Bone Joint Surg Am
2017;99:1093-103. Crossref
3. Chambers MC, El-Othmani MM, Anoushiravani AA,
Sayeed Z, Saleh KJ. Reducing 30-day readmission after
joint replacement. Orthop Clin North Am 2016;47:673-80. Crossref
4. Bosco JA 3rd, Karkenny AJ, Hutzler LH, Slover JD,
Iorio R. Cost burden of 30-day readmissions following
Medicare total hip and knee arthroplasty. J Arthroplasty
2014;29:903-5. Crossref
5. Gould D, Dowsey MM, Spelman T, et al. Patient-related risk factors for unplanned 30-day hospital readmission following primary and revision total knee arthroplasty:
a systematic review and meta-analysis. J Clin Med 2021;10:134. Crossref
6. Roger C, Debuyzer E, Dehl M, et al. Factors associated
with hospital stay length, discharge destination, and 30-day
readmission rate after primary hip or knee arthroplasty:
retrospective cohort study. Orthop Traumatol Surg Res
2019;105:949-55. Crossref
7. Bovonratwet P, Shen TS, Ast MP, Mayman DJ, Haas SB,
Su EP. Reasons and risk factors for 30-day readmission
after outpatient total knee arthroplasty: a review of 3015
cases. J Arthroplasty 2020;35:2451-7. Crossref
8. Sing CW, Woo YC, Lee AC, et al. Validity of major
osteoporotic fracture diagnosis codes in the Clinical
Data Analysis and Reporting System in Hong Kong.
Pharmacoepidemiol Drug Saf 2017;26:973-6. Crossref
9. Phruetthiphat OA, Otero JE, Zampogna B, Vasta S, Gao Y,
Callaghan JJ. Predictors for readmission following primary
total hip and total knee arthroplasty. J Orthop Surg (Hong
Kong) 2020;28:2309499020959160. Crossref
10. Ross TD, Dvorani E, Saskin R, Khoshbin A, Atrey A,
Ward SE. Temporal trends and predictors of thirty-day
readmissions and emergency department visits following
total knee arthroplasty in Ontario between 2003 and 2016.
J Arthroplasty 2020;35:364-70. Crossref
11. Kurtz SM, Lau EC, Ong KL, Adler EM, Kolisek FR,
Manley MT. Which hospital and clinical factors drive
30- and 90-day readmission after TKA? J Arthroplasty
2016;31:2099-107. Crossref
12. Ali AM, Loeffler MD, Aylin P, Bottle A. Predictors of 30-day
readmission after total knee arthroplasty: analysis of
566,323 procedures in the United Kingdom. J Arthroplasty
2019;34:242-8.e1. Crossref
13. Urish KL, Qin Y, Li BY, et al. Predictors and cost of
readmission in total knee arthroplasty. J Arthroplasty
2018;33:2759-63. Crossref
14. Yan CH, Chiu KY, Ng FY. Total knee arthroplasty for
primary knee osteoarthritis: changing pattern over the past
10 years. Hong Kong Med J 2011;17:20-5.
15. Fan JC, Lo CK, Kwok CK, Fung KY. Nurse-led orthopaedic
clinic in total joint replacement. Hong Kong Med J
2014;20:511-8. Crossref
16. MacroTrends. Hong Kong life expectancy 1950-2024.
Available from: https://www.macrotrends.net/countries/HKG/hong-kong/life-expectancy. Accessed 28 Nov 2024.
17. Cheung A, Fu H, Cheung MH, et al. How well do elderly
patients do after total knee arthroplasty in the era of fasttrack
surgery? Arthroplasty 2020;2:16. Crossref
18. Chan VW, Chan PK, Woo YC, et al. Universal haemoglobin
A1c screening reveals high prevalence of dysglycaemia in
patients undergoing total knee arthroplasty. Hong Kong
Med J 2020;26:304-10. Crossref