© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PERSPECTIVE
Adapting selected international paediatric asthma guidelines for use in Hong Kong
KL Hon, MB, BS, MD1; Daniel KK Ng, MB, BS, MD2; WK Chiu, MB, BS, MRCPCH3; Alexander KC Leung, MB, BS, FRCPC4; DH Chen, MD5; WH Leung, MB, BS, MD6
1 Department of Paediatrics, CUHK Medical Centre, The Chinese University of Hong Kong, Hong Kong SAR, China
2 Department of Paediatrics, The Hong Kong Sanitorium & Hospital, Hong Kong SAR, China
3 Department of Paediatrics and Adolescent Medicine, United Christian Hospital, Hong Kong SAR, China
4 Department of Pediatrics, The University of Calgary and The Alberta Children’s Hospital, Calgary, Canada
5 The First Affiliated Hospital of Guangzhou Medical University, Guangzhou, China
6 Department of Paediatrics and Adolescent Medicine, The University of Hong Kong, Hong Kong SAR, China
Corresponding author: Prof KL Hon (ehon@hotmail.com)
Asthma is a chronic inflammatory airway disease
characterised by variable and recurring symptoms,
episodic reversible airflow obstruction, and easily
triggered bronchospasm.1 2 3 4 5 6 7 8 A combination of
environmental and genetic factors contributes to its
onset. Diagnosis is based on clinical presentation,
response to bronchodilators and inhaled
corticosteroids (ICS), and spirometric pulmonary
function test results.9 Asthma is classified according
to symptom frequency, forced expiratory volume
in 1 second (FEV1), peak expiratory flow (PEF), and
atopic versus non-atopic aetiology. Symptoms can
be prevented by avoiding triggers and suppressed
through the use of ICS.2 7 8 10
We previously conducted an extensive review of
eight widely accepted and implemented guidelines11;
however, management approaches vary across these
guidelines. These international guidelines provide
valuable recommendations for managing childhood
asthma, especially in many Asian cities where unified
national guidelines are unavailable.11
This article offers practical insights into current
recommendations for the management of childhood
asthma, specifically focusing on diagnosis, severity
classification, treatment options, and asthma
control. We reviewed the following guidelines from
selected countries and organisations in Asia, the
United States, the United Kingdom, the European
Union, and Australasia:
(1) the Chinese guidelines 201612 13;
(2) the Chinese Children’s Asthma Action Plan consensus 202014 15;
(3) Global Initiative for Asthma (GINA) guidelines 20218 16;
(4) the National Asthma Education and Prevention Program and the National Heart, Lung, and Blood Institute (NAEPP-NHLBI) Updates 202017;
(5) the European Respiratory Society/American Thoracic Society 2020 guidelines18;
(6) the United Kingdom’s National Institute for Health and Care Excellence (NICE) 2021 guidelines19;
(7) the joint British Thoracic Society and Scottish Intercollegiate Guidelines Network 2019 guidelines20;
(8) the European Academy of Allergy and Clinical Immunology Biologicals Guidelines 202021; and
(9) the Australian Asthma Handbook of the Thoracic Society of Australia and New Zealand National Asthma Committee (TSANZ/NAC).22
(2) the Chinese Children’s Asthma Action Plan consensus 202014 15;
(3) Global Initiative for Asthma (GINA) guidelines 20218 16;
(4) the National Asthma Education and Prevention Program and the National Heart, Lung, and Blood Institute (NAEPP-NHLBI) Updates 202017;
(5) the European Respiratory Society/American Thoracic Society 2020 guidelines18;
(6) the United Kingdom’s National Institute for Health and Care Excellence (NICE) 2021 guidelines19;
(7) the joint British Thoracic Society and Scottish Intercollegiate Guidelines Network 2019 guidelines20;
(8) the European Academy of Allergy and Clinical Immunology Biologicals Guidelines 202021; and
(9) the Australian Asthma Handbook of the Thoracic Society of Australia and New Zealand National Asthma Committee (TSANZ/NAC).22
Diagnosis
Many of the reviewed guidelines are similar to the
GINA8 16 and NICE guidelines.1 5 8 12 13 14 15 16 17 18 19 20 21 22 According to
the guidelines, clinical diagnosis of asthma is based
on the acquisition of a supporting history, physical
examination findings, and the results of relevant
investigations. Notably, several guidelines do not rely
on the supporting history and physical examination
components.17 18 21
The guidelines generally agree with some but
not all of the clinical and objective approaches to
diagnosing childhood asthma described by NICE.19
According to the GINA guidelines,8 the utility of
fractional exhaled nitric oxide (FeNO) in confirming
or ruling out a diagnosis of asthma has not been
established.
According to a subset of these major
guidelines,1 5 several conclusions can be drawn. A
clinical diagnosis of asthma should be considered
in children presenting with recurring or episodic
symptoms such as wheezing, breathlessness, cough,
and/or chest tightness without an alternative
explanation. Spirometry is recommended for all
patients with suspected asthma to confirm the
diagnosis, assess the severity of airflow limitation,
and monitor asthma control. Bronchodilator
reversibility can be assessed with a peak flow
meter. Importantly, the presence of bronchodilator
reversibility is neither diagnostic of asthma nor
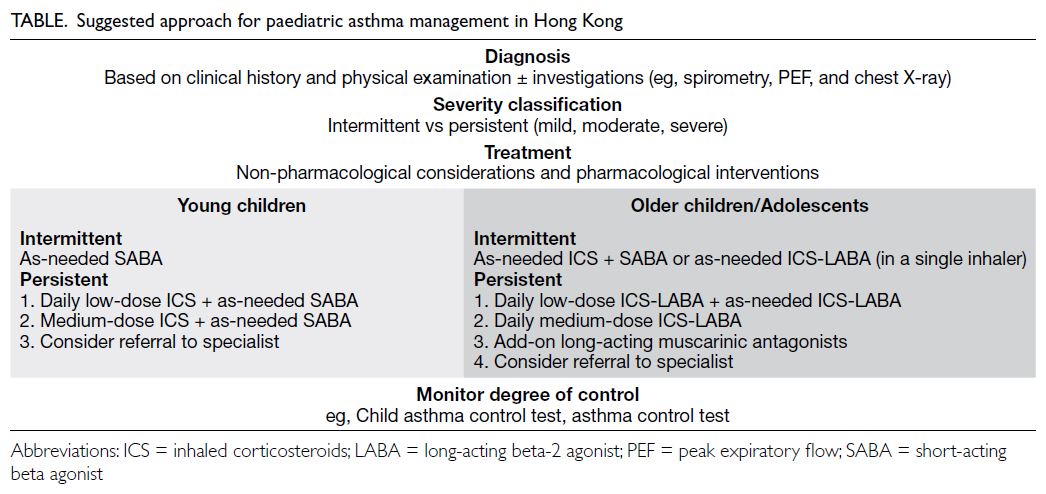
sufficient to rule it out.8 16 23 We propose a concise
reference of paediatric asthma management for local
practitioners (Table).
Severity
Classification of asthma severity is generally
recommended,1 5 8 12 13 14 15 16 18 20 21 22 except by the NAEPP-NHLBI17
and NICE guidelines.19 Asthma severity
is typically classified as mild, moderate, or severe.
According to the GINA guidelines,8 asthma severity
is not a static state and may change over time and is
currently assessed retrospectively based on the level
of treatment required for symptom and exacerbation
control. On the other hand, the NHLBI classifies
severity as intermittent or persistent and mild,
moderate, or severe.1 24
Treatment
Treatment comprises both pharmacological
and non-pharmacological interventions.1 5 8 12 13 14 15 16 17 18 19 20 21 22
Pharmacological interventions are similar across
guidelines, with specific recommendations for young
children and older children/adolescents. Notably,
the GINA8 and the Chinese guidelines12 13 14 are similar
in this regard. The GINA guidelines16 recommend
short-acting beta agonists (SABAs) as needed for
symptom relief across all management steps. Short
courses of oral corticosteroids may be necessary
for patients presenting with severe uncontrolled
asthma. The NAEPP-NHLBI guidelines5 17 24 also
recommend SABAs as needed for symptom relief
across all management steps. Stepwise management
for asthma differs according to age-group in the joint
British Thoracic Society and Scottish Intercollegiate
Guidelines Network20 and the TSANZ/NAC
guidelines.22 Similarly, the NICE guidelines19
recommend distinct stepwise management for
asthma according to age-group.
Treatment for adolescents is outlined in two
‘Tracks’ within the GINA guidelines.16 Track 1,
using ICS-formoterol for symptom relief, is the preferred approach. Track 2, utilising SABAs for
symptom relief, is a recommended alternative if
Track 1 is not feasible or preferred by a patient
who has not experienced exacerbations with their
current therapy.16 The guideline for children aged
6 to 11 years has been updated to include low-dose
budesonide-formoterol for maintenance and relief
therapy.16
The NAEPP-NHLBI 2020 guideline also
includes focused updates.2 17 Among children aged 0
to 4 years, a short course of daily ICS, rather than
as-needed SABAs, is recommended at the onset of a
respiratory tract infection.2 9 17 Among children aged
≥12 years with uncontrolled persistent asthma, the
addition of long-acting beta-2 agonist (LABA) to
ICS therapy is preferred over the addition of long-acting
muscarinic antagonists, as recommended by
the Chinese guidelines.12 13 14 The use of sublingual
immunotherapy for childhood asthma is not generally
recommended due to insufficient evidence.8 9 12 13 14 19 24
Inhaled corticosteroids are the preferred
controller medication for management of stable
asthma. Most of the clinical benefit from ICS
therapy is achieved at low to moderate doses.
Inhaled corticosteroids should be started at a low
to moderate dose (depending on initial symptom
severity) and used at the lowest possible effective
dose. High-dose ICS use should ideally be avoided
to minimise the risks of local and systemic side-effects.
Long-acting beta-2 agonist monotherapy
should not be used for stable asthma. The addition
of LABA to ICS therapy is preferred when symptoms
remain uncontrolled despite moderate doses of ICS
monotherapy.11
Leukotriene modifiers have no role in the
management of acute asthma. Monotherapy with
leukotriene receptor antagonists (LTRAs) may be
an acceptable alternative to ICS for patients with mild asthma who are unwilling or unable to receive
ICS therapy.8 16 The addition of LTRAs might benefit
patients whose asthma remains uncontrolled despite
ICS/LABA combination therapy.8 16 25 Tiotropium
may be considered as an add-on treatment if asthma
remains uncontrolled on moderate-to-high-dose
ICS/LABA combination therapy.18 Methylxanthine
monotherapy is less effective compared to ICS alone.
Short-acting beta agonists are the preferred
rescue medications for asthma. Short-acting
muscarinic antagonists are less preferred as
alternatives or add-ons to SABA for symptom
relief. Formoterol monotherapy for relief should
be avoided due to safety concerns associated with
LABA monotherapy. Oral beta 2 agonists are not
recommended for rescue use. It is preferable to
consider single-inhaler therapy, incorporating an
ICS/LABA combination (formoterol-based) for both
maintenance and relief purposes.11
Rapid-acting inhaled beta-2 agonists (eg,
salbutamol) are the preferred bronchodilators
for managing acute exacerbations of asthma.
The combination of ipratropium bromide with
salbutamol results in better bronchodilation than
either medication alone. Ipratropium should be
administered to all patients experiencing severe
exacerbations of asthma (eg, 500 μg once then 250 μg
every 4-6 hours). Metered-dose inhalers with spacers
are comparable to nebulisers for managing acute
asthma. Nebulisers require higher doses and have
greater potential for side-effects. Among patients
unable to use a metered-dose inhaler with a spacer,
medications can be delivered through a nebuliser.
After a patient has been stabilised, they should be
switched from a nebuliser to a spacer. Continuous
nebulisation (2.5 mg salbutamol every 15 minutes
or >4 nebulisations per hour) of rapid-acting SABAs
is better than intermittent nebulisation (2.5 mg
salbutamol every 20 minutes or ≤3 nebulisations per
hour). Subsequent doses of nebulised salbutamol
should be 2.5 mg every 2 to 4 hours, depending
on the clinical response. Formoterol offers no
additional benefit over salbutamol; therefore, it is
not recommended for routine use in patients with
acute asthma.11
Systemic glucocorticoids should be
administered to all patients with severe acute
asthma. The oral route is as effective as the parenteral
route, except in critically ill patients and in patients
with contraindications to enteral feeding. For most
patients, daily doses of glucocorticoids equivalent
to 1 to 2 mg/kg of prednisolone for 5 to 7 days are
sufficient. Systemic steroids can be discontinued
without tapering if administered for <3 weeks. In
cases of non-severe exacerbation, patients should
first receive an increased dose of inhaled SABA
(4-6 puffs of 100 μg salbutamol every 30 minutes). If
there is no response within 1 hour, oral prednisone (1-2 mg/kg) once daily for 5 to 7 days should be
initiated. Inhaled corticosteroids do not offer
added benefits when combined with systemic
corticosteroids and are thus not recommended for
acute asthma treatment.11
Omalizumab may be considered as adjunct
to ICS in patients with moderate to severe asthma,
characterised by elevated serum immunoglobulin
E (IgE) levels and a positive skin test result for at
least one perennial aeroallergen.26 Single-allergen
immunotherapy may provide modest benefits
to patients with mild-to-moderate asthma and
a skin allergy to that specific antigen. However,
multiple-allergen immunotherapy is not currently
recommended due to lack of evidence.
The NICE guideline also recommends other
therapeutic interventions for asthma management,
including oxygen therapy, traditional Chinese
medicine, breathing exercises, and vitamin D
supplementation.19 However, there is no consensus
among guidelines regarding non-pharmacological
management options,19 21 particularly in terms
of prevention/self-management and alternative
therapies. Alternative therapies are not generally
recommended. Trigger avoidance, patient
education, adolescent-to-adult care transition,
lifestyle modifications, and asthma action plans are
recommended.19 21
Monitoring control
Monitoring of asthma control is generally
recommended,1 5 8 12 13 14 15 16 17 19 20 22 except in the European
Respiratory Society/American Thoracic Society
202018 and European Academy of Allergy and
Clinical Immunology 2020 guidelines.21 Asthma
control should be classified as either adequate or
inadequate, considering daytime symptoms (or
rescue medication use), nighttime symptoms/awakening, activity limitations, and the results of
pulmonary function tests (eg, PEF or FEV1 value).
Spirometry or PEF variability assessment is
generally recommended, but there is no agreement
regarding specific thresholds.8 12 13 14 According to the
GINA guidelines,8 diurnal PEF variability of >13% in
children are considered excessive. If a patient’s FEV1
value falls within the predicted normal range during
symptom presentation, it is less likely that those
symptoms are attributable to asthma. However,
patients with a baseline FEV1 value >80% of the
predicted value can experience clinically significant
improvement in lung function with bronchodilator
or controller treatment. Predicted normal ranges
(especially for PEF) have limitations because no such
ranges have been established in children. Therefore,
the GINA guidelines recommend using the patient’s
own best reading as their ‘normal’ value.8 12 13 14
According to the Chinese guidelines and
recommendations, continuous monitoring of FeNO can help assess asthma control and guide
the development of an optimal asthma treatment
regimen.12 13 14 15 School-age children are generally
able to cooperate with the sputum induction
test procedure.8 12 13 14 Continuous monitoring of
induced sputum eosinophil count may be useful
to assess asthma control and guide optimisation of
management.8 12 13 14
Asthma management may require adjustments
to medication regimens through a control-based
cycle approach that involves timely treatment
escalation and de-escalation, along with regular
monitoring. Treatment escalation is indicated if
control is not achieved after reviewing patient
adherence, inhaler technique, and trigger control.19
Treatment de-escalation can be considered when
symptoms have been well-controlled for at least 3
months (as per the Chinese,12 13 14 15 NAEPP-NHLBI,17
and NICE guidelines19)5 24 or 6 months (with close
supervision within 4-6 weeks as per the TSANZ/NAC guidelines).22 Asthma control assessment is a
key component of asthma care. For children, self-monitoring
using an asthma diary is recommended
only by the Chinese12 13 and GINA guidelines.8 16
Peak expiratory flow measurements should
not be substituted for FEV1 measurements. Patient
self-monitoring of PEF is recommended to facilitate
better asthma control. Routine bronchoprovocation
testing is not recommended for diagnosing
asthma. However, methacholine challenge can
be utilised to rule out asthma as a differential
diagnosis, particularly when spirometry results are
normal. While chest radiographs are not routinely
recommended for patients with suspected asthma,
they may be considered if an alternative diagnosis or
asthma-related complication is suspected.24
Quantification of the eosinophil count in
sputum (<2% is considered normal while >2%
indicates eosinophilic inflammation) can guide
ICS therapy, potentially minimising the risk of
exacerbations in adults with moderate-to-severe
asthma.24
Routine measurement of FeNO is not
recommended in asthma management. Similarly,
routine assessments of allergic status, eg,
measurements of total IgE level, measurements
of IgE level specific to different environmental
allergens, and skin prick tests, are not recommended
for diagnosing and managing asthma.24
Oxygen saturation should be assessed using
pulse oximetry for all patients presenting with an
acute asthma attack. Non-severe exacerbations
usually do not require additional investigations.
Patients with a PEF <60% of predicted or personal
best should receive care in the emergency
department. Patients with oxygen saturation
levels <92% should be managed in the emergency
department or hospital ward and should undergo further investigation through arterial blood gas
analysis. Oxygen should only be administered to
hypoxaemic patients; it should be titrated to maintain
oxygen saturation level to stay between 93% and
95%. The absence of pulse oximetry or arterial blood
gas data should not preclude oxygen administration.
In patients requiring oxygen flow rates >8 L/min,
partial pressure of carbon dioxide should be closely
monitored.24
Pulmonary rehabilitation improves asthma
symptoms and quality of life, and significantly
improve exercise capacity. Pretreatment with
bronchodilator agents (SABAs, short-acting
muscarinic antagonists, and LABAs), as well as anti-inflammatory
agents (LTRAs but not ICS), is effective
in attenuating the reduction of FEV1 associated with
exercise-induced asthma.8 16 27 Regular use of ICS or
LTRAs is effective in preventing exercise-induced
asthma.27
Smoking cessation should be recommended
for all asthma patients who smoke. Optimal self-management
of asthma, involving patient education,
self-monitoring, regular physician review, and a
written asthma action plan, is recommended.
Conclusion
Despite the recent comprehensive update of the
GINA guidelines in 2023,28 29 it remains impractical
to fully adhere to these guidelines or any other
single set of guidelines in both public and private
paediatric healthcare settings within Hong Kong due
to multiple pragmatic issues.
Asthma is a heterogeneous syndrome
encompassing many underlying causes and patient
characteristics, along with varying degrees of
mucus hypersecretion, airway hyperreactivity, and
inflammation.30 A severity classification should be
established to guide treatment. Current clinical
management aims for disease control, including
symptom control, risk reduction, and prevention
of severe exacerbations. A personalised treatment
strategy, with inhaler therapy as the core, which
titrates airway inflammation and bronchodilation
therapies according to symptoms and objective
asthma assessments, should benefit most patients
with asthma. It can be difficult, if not impossible, for
general practitioners and paediatricians to follow
these guidelines due to various constraints, including
the availability of diagnostic tools, the need to
incorporate patient preferences, and the frequency
of guideline updates. For example, the latest update
to the GINA 2024 report was published on 22
May 2024 to clarify some medication doses.31 The
maintenance and as-needed use of ICS-formoterol,
as proposed by the GINA8 16 31 and NICE guidelines,19
offers a simple, flexible, and safe treatment option
for patients with asthma and clinicians. Short-acting
beta agonists with or without ICS remain the preferred treatment for young children. However,
inhaler therapy adherence, steroid phobia, and
mistrust of Western medicine remain important
health issues for patients with asthma and their
families.32
Guidelines should not be rigidly followed;
factors such as resources, family attitudes,
and compliance must be considered. In-depth
counselling and the establishment of good rapport
are key components to successful management of
this prevalent and challenging disease in Hong Kong.
Author contributions
All authors contributed to the concept or design, acquisition
of the data, analysis or interpretation of the data, drafting of
the manuscript, and critical revision of the manuscript for
important intellectual content. All authors had full access to
the data, contributed to the study, approved the final version
for publication, and take responsibility for its accuracy and
integrity.
Conflicts of interest
As an editor of the journal, KL Hon was not involved in the peer review process. Other authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
1. Agarwal R, Dhooria S, Aggarwal AN, et al. Guidelines for diagnosis and management of bronchial asthma: joint ICS/NCCP (I) recommendations. Lung India 2015;32(Suppl 1):S3-42. Crossref
2. Lee DL, Baptist AP. Understanding the updates in the asthma guidelines. Semin Respir Crit Care Med 2022;43:595-612. Crossref
3. Gupta RS, Weiss KB. The 2007 National Asthma Education and Prevention Program asthma guidelines: accelerating their implementation and facilitating their impact on children with asthma. Pediatrics 2009;123 Suppl 3:S193-8. Crossref
4. Khan L. Overview of the updates for the management of asthma guidelines. Pediatr Ann 2022;51:e132-5. Crossref
5. National Asthma Education and Prevention Program. Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007. J Allergy Clin Immunol 2007;120(5 Suppl):S94-138. Crossref
6. Urbano FL. Review of the NAEPP 2007 Expert Panel Report (EPR-3) on Asthma Diagnosis and Treatment Guidelines. J Manag Care Pharm 2008;14:41-9. Crossref
7. National Heart, Lung, and Blood Institute, National
Institutes of Health, United States Department of Health
and Human Services. National Asthma Education and
Prevention Program Expert Panel Report 3: Guidelines for
the Diagnosis and Management of Asthma—Full Report
2007. 2007 Aug 28. Available from: https://www.nhlbi.nih.gov/sites/default/files/media/docs/EPR-3_Asthma_Full_Report_2007.pdf. Accessed 29 Nov 2024.
8. Global Initiative for Asthma. Global Strategy for Asthma
Management and Prevention—Updated 2011. 2011. Available from: https://ginasthma.org/wp-content/uploads/2019/01/2011-GINA.pdf. Accessed 29 Nov 2024.
9. Lemans RF Jr, Busse WW. Asthma: clinical expression and molecular mechanisms. J Allergy Clin Immunol 2010;125(2 Suppl 2):S95-102. Crossref
10. Boulet LP, FitzGerald JM, Reddel HK. The revised 2014 GINA strategy report: opportunities for change. Curr Opin Pulm Med 2015;21:1-7. Crossref
11. Hon KL, Ng DK, Chiu WK, Leung AK. Insights from overviewing selective international guidelines for pediatric asthma. Curr Pediatr Rev 2024 Jan 29. Epub ahead of print. Crossref
12. Subspecialty Group of Respiratory Diseases, Society of Pediatrics, Chinese Medical Association; Editorial Board, Chinese Journal of Pediatrics. Guideline for the diagnosis and optimal management of asthma in children (2016) [in Chinese]. Zhonghua Er Ke Za Zhi 2016;54:167-81. Crossref
13. Hong J, Bao Y, Chen A, et al. Chinese guidelines for childhood asthma 2016: major updates, recommendations and key regional data. J Asthma 2018;55:1138-46. Crossref
14. Zhang B, Jin R, Guan RZ, et al. Evaluation of the efficacy of Chinese Children's Asthma Action Plan on the long-term management of children with asthma at home [in Chinese]. Zhonghua Yi Xue Za Zhi 2020;100:3702-5. Crossref
15. Zhu K, Xiang L, Shen K. Efficacy of Chinese Children's Asthma Action Plan in the management of children with asthma. Allergy Asthma Proc 2020;41:e3-10. Crossref
16. Reddel HK, Bacharier LB, Bateman ED, et al. Global Initiative for Asthma Strategy 2021: executive summary and rationale for key changes. J Allergy Clin Immunol Pract 2022;10:S1-18. Crossref
17. Expert Panel Working Group of the National Heart, Lung, and Blood Institute (NHLBI) administered and coordinated National Asthma Education and Prevention Program Coordinating Committee (NAEPPCC); Cloutier MM, Baptist AP, et al. 2020 focused updates to the asthma management guidelines: a report from the National Asthma Education and Prevention Program Coordinating Committee Expert Panel Working Group. J Allergy Clin Immunol 2020;146:1217-70. Crossref
18. Holguin F, Cardet JC, Chung KF, et al. Management of severe asthma: a European Respiratory Society/American Thoracic Society guideline. Eur Respir J 2020;55:1900588. Crossref
19. Asthma: diagnosis, monitoring and chronic asthma
management; NICE guideline [NG80]. London: National
Institute for Health and Care Excellence (NICE). Updated
2021 Mar 22. Available from: https://www.nice.org.uk/guidance/ng80. Accessed 29 Nov 2024.
20. Healthcare Improvement Scotland, United Kingdom.
British guideline on the management of asthma: a national
clinical guideline. Jul 2019 (revised). Available from:
https://digirepo.nlm.nih.gov/master/borndig/101772271/sign158.pdf. Accessed 9 Feb 2025.
21. Agache I, Akdis CA, Akdis M, et al. EAACI Biologicals Guidelines-recommendations for severe asthma. Allergy 2021;76:14-44. Crossref
22. National Asthma Council. Australian Asthma Handbook.
Available from: https://www.asthmahandbook.org.au/. Accessed 1 Mar 2023.
23. Tan DJ, Lodge CJ, Lowe AJ, et al. Bronchodilator reversibility as a diagnostic test for adult asthma: findings from the population-based Tasmanian Longitudinal Health Study. ERJ Open Res 2021;7:00042-2020. Crossref
24. Mammen JR, McGovern CM. Summary of the 2020 focused updates to U.S. asthma management guidelines: what has changed and what hasn't? J Am Assoc Nurse Pract 2021;34:238-41. Crossref
25. Sadatsafavi M, Lynd L, Marra C, Bedouch P, Fitzgerald M.
Comparative outcomes of leukotriene receptor antagonists
and long-acting β-agonists as add-on therapy in asthmatic
patients: a population-based study. J Allergy Clin Immunol
2013;132:63-9. Crossref
26. Lin CH, Cheng SL. A review of omalizumab for the
management of severe asthma. Drug Des Devel Ther
2016;10:2369-78. Crossref
27. Grzelewski T, Stelmach I. Exercise-induced
bronchoconstriction in asthmatic children: a comparative
systematic review of the available treatment options. Drugs
2009;69:1533-53. Crossref
28. Venkatesan P. 2023 GINA report for asthma. Lancet Respir
Med 2023;11:589. Crossref
29. Levy ML, Bacharier LB, Bateman E, et al. Key
recommendations for primary care from the 2022 Global
Initiative for Asthma (GINA) update. NPJ Prim Care
Respir Med 2023;33:7. Crossref
30. Pavord ID, Beasley R, Agusti A, et al. After asthma:
redefining airways diseases. Lancet 2018;391:350-400. Crossref
31. Global Initiative for Asthma. 2024 GINA Main Report.
Global Strategy for Asthma Management and Prevention.
2024. Available from: https://ginasthma.org/2024-report/. Accessed 29 Nov 2024.
32. Ip KI, Hon KL, Tsang KY, Leung TN. Steroid phobia, Chinese medicine and asthma control. Clin Respir J 2018;12:1559-64. Crossref