© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Factors affecting human papillomavirus vaccine acceptance among parents of Primary 4 to 6 boys and girls in Hong Kong
Jody KP Chu, MClinPharm1; CW Sing, PhD1; Y Li, BPharm1; Patrick H Wong, BSc2; Eric YT So, MPH2; Ian CK Wong, PhD1,3
1 Department of Pharmacology and Pharmacy, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong SAR, China
2 Merck Sharp and Dohme (Asia) Ltd, Hong Kong SAR, China
3 Research Department of Practice and Policy, School of Pharmacy, University College London, London, United Kingdom
Corresponding author: Ms Jody KP Chu (chukpj@hku.hk)
Abstract
Introduction: Human papillomavirus (HPV) poses a
substantial but underestimated healthcare burden in
Hong Kong. This study investigated factors affecting
parental acceptance of HPV vaccination after
the introduction of an immunisation programme
for primary school girls. We assessed parental
perceptions and related factors concerning HPV
vaccination for both boys and girls.
Methods: We conducted a cross-sectional survey
between December 2021 and February 2022 among
parents of Primary 4 to 6 students in Hong Kong.
Our self-administered online survey collected
data regarding socio-demographic characteristics,
awareness and knowledge of HPV vaccination,
attitudes towards HPV vaccination, and acceptance
of HPV vaccination. Characteristics were compared
between boys’ parents and girls’ parents. Factors
associated with vaccine acceptance were analysed by
multivariate logistic regression.
Results: We observed high awareness of HPV
vaccination among boys’ parents and girls’
parents; however, they demonstrated relatively
poor knowledge of HPV and the HPV vaccine. An
alarming low HPV vaccination uptake rate was also
observed. Attitudes towards the HPV vaccine were
similar between parent groups. A majority of parents
believed that the HPV vaccine was safe and effective
in preventing infection. Parents of boys showed lower HPV vaccine acceptance. Factors associated
with acceptance differed between parent groups.
Conclusion: High awareness of HPV and HPV
vaccine is predictive of vaccine acceptance. Boys’
parents are less likely to accept HPV vaccination
and emphasis should be placed on addressing
potential HPV vaccine hesitancy in this group.
Public education should also aim to raise awareness
of government vaccination programme, and
implementation of catch-up vaccination programme
to school children beyond primary school should be
considered.
New knowledge added by this study
- Awareness of human papillomavirus (HPV) was similar between parents of boys and parents of girls (P=0.346); 81.4% of boys’ parents and 78.5% of girls’ parents had heard of HPV.
- Overall, attitudes towards HPV and the HPV vaccine were similar between parents of boys and parents of girls.
- High acceptance of their child receiving the HPV vaccine in both parents of boys and girls was observed; parents of girls were more likely to accept the vaccine, compared with parents of boys (89.7% vs 73.8%; P<0.001).
- The awareness of the HPV vaccination programme among girls’ parents is low, echoing the problem of insufficient information provision concerning HPV vaccination, especially during the coronavirus disease 2019 pandemic.
- To prevent future healthcare burdens caused by immunisation gaps, catch-up vaccination services for affected children should be considered and implemented as soon as possible.
Introduction
Human papillomavirus (HPV) is a common sexually
transmitted infection that constitutes a substantial global healthcare burden. It is associated with genital
warts and various cancers (eg, cervical, penile, anal,
oropharyngeal, and head and neck cancers). Human papillomavirus causes 4.5% (630 000) of all new
cancer cases worldwide.1
In Hong Kong, cervical cancer is the ninth
most common cancer, with a crude incidence of 12.9
per 100 000 women and girls.2 3 There are limited
data regarding HPV infection or HPV-associated
cancers in men and boys. A local study estimated
that the incidence of genital warts in Hong Kong was
203.7 per 100 000 person-years. Men and boys had
a higher incidence compared with women and girls
(292.2 per 100 000 person-years vs 124.9 per 100 000
person-years, respectively), suggesting a similar or
possibly higher prevalence of HPV infection in men
and boys.4
Human papillomavirus vaccination is a
highly effective preventive measure against HPV
infection and its complications. National HPV
vaccination programmes targeting adolescent girls
have significantly reduced the incidences of HPV-associated
diseases.5 The World Health Organization
recommends including HPV vaccination in routine
programmes for girls aged 9 to 14 years, with possible
extension to boys if feasible.6
Universal HPV vaccination programmes,
covering both adolescent boys and adolescent girls,
have become increasingly common in recent years,
particularly in developed countries such as the
United States, Canada, Australia, and 20 European
nations. Female-only vaccination programmes with
high vaccine coverage rates have demonstrated
substantial public health impact concerning several
HPV-related diseases and cancers.7 Gender-neutral
vaccination programmes, targeting both boys and
girls, have shown greater resilience8 and faster
elimination of cervical cancer9; they also provide
direct protection to reduce disease burden in all men
and in subpopulations of men (eg, men who have
sex with men and men who have sex abroad).10 11 12
The achievement of an 80% vaccination rate in both
sexes is expected to enable the elimination of HPV
subtypes 6, 11, 16, and 18.13
Despite the benefits of a high vaccination rate,
the current rate of HPV vaccine is much lower than
desired. In Hong Kong, the rate of vaccine uptake
reportedly ranged from 2.2% to 7.2% in adolescent
girls and 0.6% in adolescent boys before the HPV
vaccine was incorporated into the Hong Kong
Childhood Immunisation Programme (HKCIP).14 15 16
The 9-valent HPV vaccine was introduced into the
Programme for Primary 5 and 6 girls, with a reported
first-dose uptake rate of 85% among Primary 5 girls
in 2020.17 However, vaccination rates are expected to
remain low among adolescent boys.
Prior to the inclusion of HPV vaccination in the
HKCIP, few local studies explored parental decision-making14 15 16 18; those that did primarily focused on
girls, with limited examination of factors influencing
vaccine acceptance or uptake. One survey did include parents of adolescent boys but was hindered by its
small sample size (162 boys’ parents).14 Considering
the recent implementation of the HPV vaccination
programme for primary school girls and the lack
of sufficient data concerning HPV vaccination in
Hong Kong, further local research is warranted. An
understanding of parental acceptance, particularly
for boys, can inform strategies to improve vaccine
uptake.
This study aimed to identify factors affecting
HPV vaccination acceptance among Hong Kong
parents of Primary 4 to 6 students. It compared
the knowledge, attitudes, and acceptance between
girls’ parents and boys’ parents, then explored the
underlying reasons for their vaccination decisions.
Methods
Study design
This cross-sectional survey was conducted from
December 2021 to February 2022. Invitation letters
were sent to 554 primary schools in Hong Kong,
including public local schools, private local schools,
and Direct Subsidy Scheme schools. In total, 65
schools agreed to participate. After consent had
been obtained from participating schools, parents
of Primary 4 to 6 students at those schools received
a self-administered online survey through the
Qualtrics platform.
Measures
The survey was divided into four sections, namely, (1) socio-demographic characteristics, (2) awareness and knowledge regarding HPV and HPV vaccination,
(3) attitudes towards HPV vaccination, and (4)
acceptance of HPV vaccination. The questionnaires
were available in both English and Chinese (online supplementary Appendices 1 and 2, respectively).
A detailed description of the survey sections is
provided in online supplementary Appendix 3. Upon
completion of the online survey, the results were
stored in the Qualtrics platform for further analysis.
Data analysis
Human papillomavirus vaccination attitudes were
measured using a five-point Likert scale. Two
statements (Questions 41 and 42) with strong
internal consistency (Cronbach’s alpha=0.81) were
combined to form the variable ‘Worried about
HPV infection’, and the mean score of the two
statements was used for analysis. Similarly, two
other statements (Questions 46 and 47) with strong
internal consistency (Cronbach’s alpha=0.91) were
merged into the variable ‘Worried that HPV vaccine
might negatively impact child’s sexual activity’.
Descriptive statistics were used to characterise
the participants and study variables. The first analysis
compared the knowledge, attitudes, and acceptance
of the HPV vaccine between boys’ parents and girls’
parents. Significant differences between groups were
identified using the Chi squared test for nominal
variables, the t test for continuous variables, and
the Mann-Whitney U test for ordinal variables (age-group,
household income, and education level).
In the second analysis, we investigated factors
associated with the acceptance of HPV vaccination
for children. Participants whose children had
already received HPV vaccination were excluded
from the analysis due to missing values in some
variables (Questions 49 to 51). Univariate logistic
regression was used to estimate the crude odds ratio
(OR) and 95% confidence interval (CI). The study
variables were included as independent predictors;
the acceptance of HPV vaccination for children was
regarded as a binary dependent variable (‘Yes’ or
‘No’). Variables with P values <0.1 were entered into
multivariate logistic regression. P values <0.05 were
considered statistically significant.
Because free HPV vaccination was only
provided for primary school girls in Hong Kong,
we assumed that factors affecting the acceptance of
HPV vaccination for their child varied between boys’
parents and girls’ parents. Consequently, the second
analysis was conducted separately for each parent
group.
All analyses were conducted using R software (version 4.1.1).
Results
In total, 844 participants completed the survey.
Of these, 43.8% were parents of boys and 56.2%
were parents of girls. The socio-demographic
characteristics of the parents are presented in Table 1.
Vaccine uptake rate
The HPV vaccine uptake rate is low with boys’ parents reported 6.8% and girls’ parents reported
4.9%. Among children who have received HPV
vaccine, >90% of parents in both groups reported
that their children received the HPV vaccine through
the HKCIP (Table 1).
Awareness and knowledge of human papillomavirus and the vaccine among parents
Awareness of HPV was similar between boys’
parents and girls’ parents (81.4% vs 78.5%; P=0.346).
Knowledge scores regarding HPV and the HPV
vaccine were low in both parent groups; parents of
boys had higher mean scores compared with parents
of girls (6.48 vs 6.03; P=0.012). More boys’ parents
discussed sexually transmitted disease (STDs) with
their children, relative to girls’ parents (33.0% vs
15.2%; P<0.001) [Table 2].
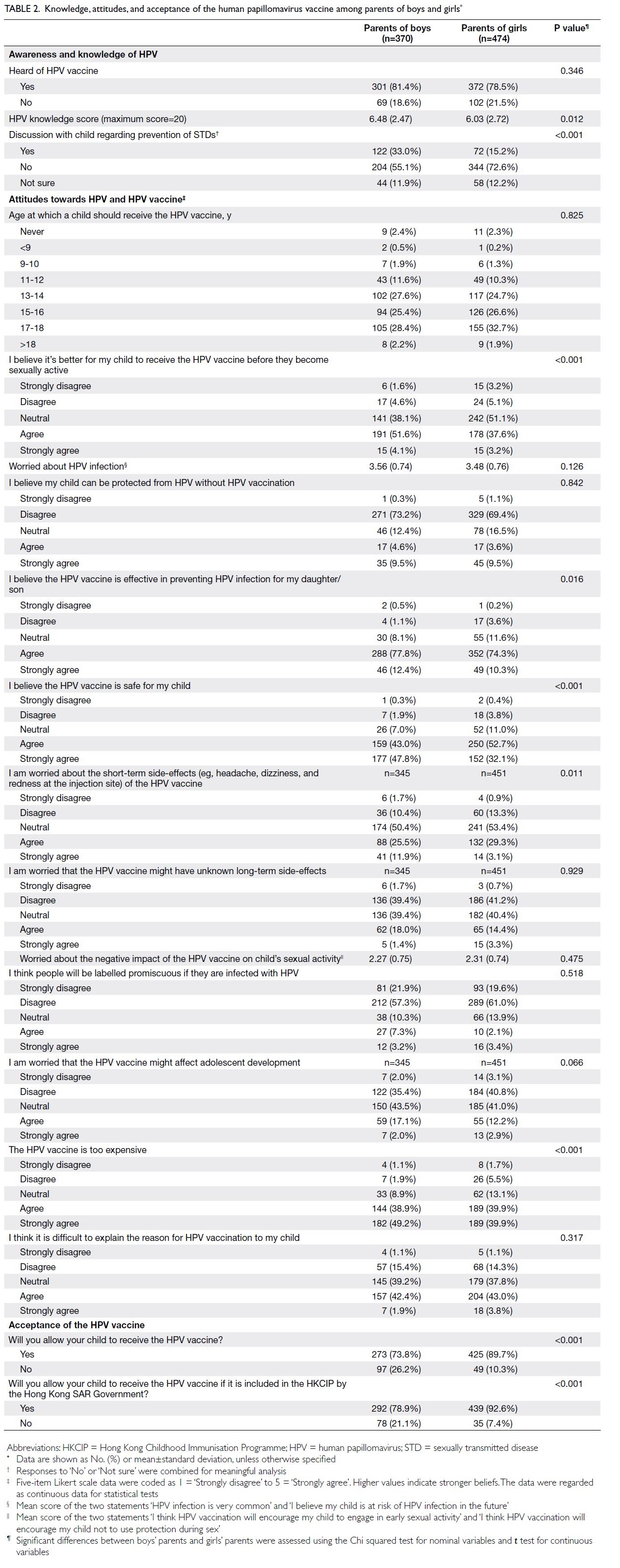
Table 2. Knowledge, attitudes, and acceptance of the human papillomavirus vaccine among parents of boys and girls
Attitudes towards the vaccine in parents
Two questions addressed the timing of vaccination,
namely: ‘At what age should a child receive the
HPV vaccine?’, and the yes/no statement ‘I believe
it’s better for my child to receive the HPV vaccine
before they become sexually active’. A majority of
parents, both of boys (83.6%) and of girls (85.9%),
believed that their children should receive the HPV
vaccine at age ≥13 years. Additionally, more parents
of boys (55.7%) believed that their children should
receive the HPV vaccine before becoming sexually
active; more parents of girls (51.1%) reported a
neutral perspective on this statement. Regarding
HPV infection and HPV vaccine effectiveness,
parents in both groups were worried about HPV
infection (mean±standard deviation [SD] out of
5: 3.56±0.74 in boys’ parents; 3.48±0.76 in girls’
parents). Over 70% in parents of both groups believe
that their children cannot be protected from HPV
without HPV vaccination, furthermore a majority of
parents in both groups also believe in the vaccine’s
effectiveness (90.2% in boys’ parents and 84.6% in
girls’ parents) [Table 2].
Concerning vaccine safety, impacts, and cost,
most parents of boys (90.8%) and parents of girls
(84.8%) agreed that the HPV vaccine is safe. They
had a neutral perspective or were less worried
about the vaccine’s short-term (62.5% and 67.6%, respectively) and long-term side-effects (80.5% and 82.3%, respectively) [Table 2].
Additionally, parents had a neutral
perspective or were less worried about the vaccine’s
negative impacts or influence on adolescent
development. However, most parents agreed that
the HPV vaccine is too expensive (88.1% and 79.8%,
respectively) [Table 2].
Vaccine acceptance in parents of boys and girls
We observed high acceptance of the HPV vaccine
for their children in boys’ parents (73.8%) and girls’
parents (89.7%). If the HPV vaccine were subsidised
under the HKCIP, acceptance in parents would
slightly increase because the government would cover
the cost (78.9% and 92.6%, respectively) [Table 2].
The reasons for accepting the HPV vaccine
for their children were similar between parent
groups (Fig), with a majority citing concerns about HPV infection (91.0% in boys’ parents and 78.6% in
girls’ parents). Acceptance was least influenced by
religions and culture (<3%) or advertisements (<5%)
in parents of both sexes. The reasons for declining
the HPV vaccine for their children were somewhat
different between boys’ parents and girls’ parents.
‘The HPV vaccine is too expensive’ was the top
reason chosen by both boys’ parents (46.4%) and
girls’ parents (42.9%). The other two reasons most
often selected by boys’ parents were ‘Not enough
information about the HPV vaccine provided to
me’ (32.0%) and ‘My child doesn’t like vaccinations’
(22.7%). For girls’ parents, the other two reasons
were ‘My child doesn’t like vaccinations’ (38.8%) and
‘The HPV vaccine can cause adverse effects/is not
safe’ (36.2%) [online supplementary Fig].
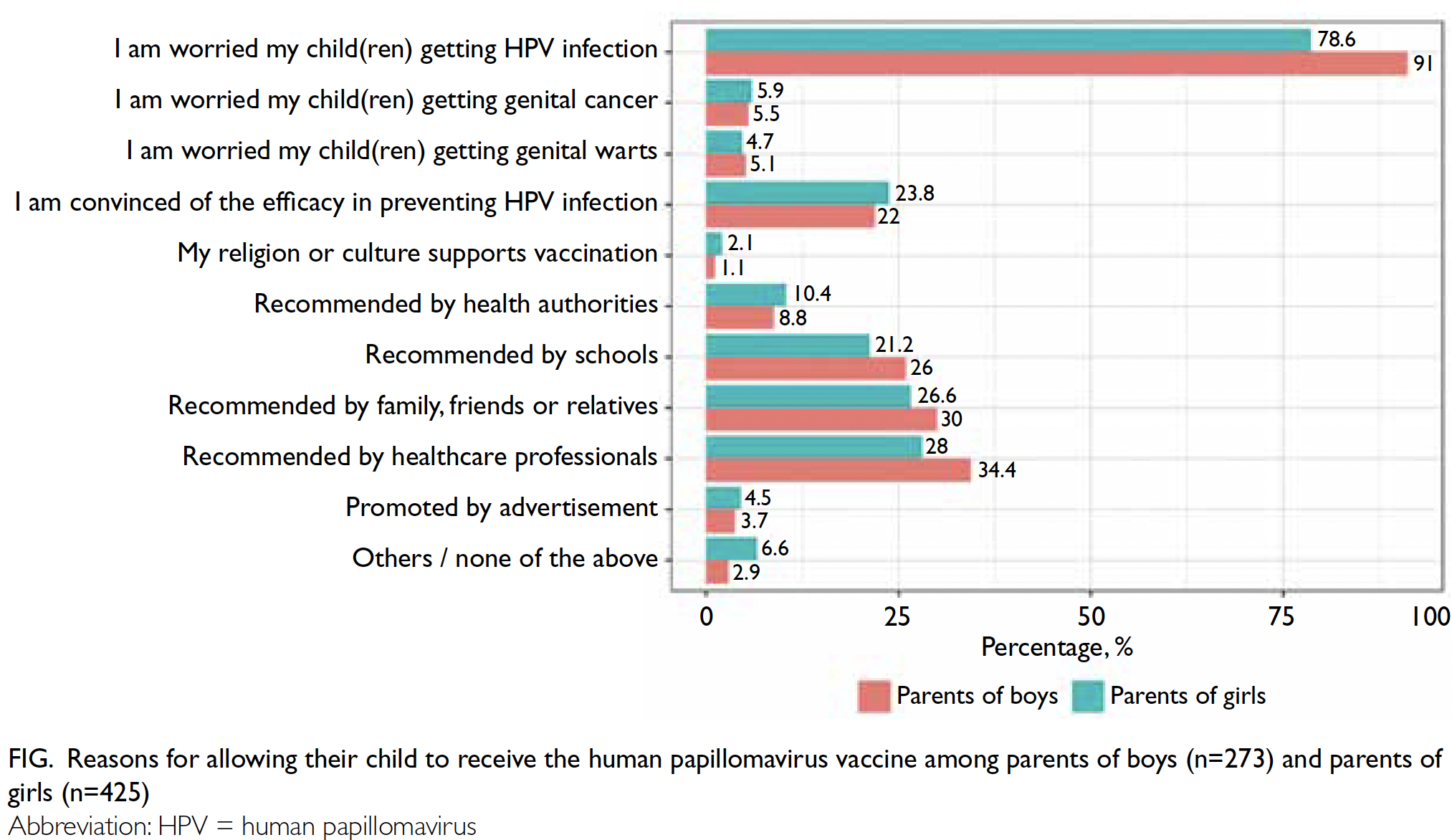
Figure. Reasons for allowing their child to receive the human papillomavirus vaccine among parents of boys (n=273) and parents of girls (n=425)
Factors associated with vaccine acceptance
for children
The association analysis excluded 25 parents of boys
and 23 parents of girls whose children had already
received the HPV vaccine. The acceptance rates
of the HPV vaccine for children of boys’ parents
and girls’ parents, stratified according to the study
variables, are listed in online supplementary Tables 1 and 2, respectively.
Regarding boys’ parents, 24 study variables with
P values <0.1 in univariate logistic regression were
entered into multivariate logistic regression (Table 3). Factors associated with higher acceptance of the HPV
vaccine for children included parental receipt of the
HPV vaccine (OR=9.36, 95% CI=1.5-63.82; P=0.018),
knowledge of the HPV vaccine (OR=10.16, 95%
CI=3.02-39.07; P<0.001), and stronger beliefs that
‘it’s better for my child to receive the HPV vaccine
before they become sexually active’ (OR=3.27, 95%
CI=1.66-7.09; P=0.001) and ‘I am worried that the
HPV vaccine might affect adolescent development’
(OR=2.56, 95% CI=1.39-5.03; P=0.004). Conversely,
factors associated with lower acceptance of the
HPV vaccine were the presence (in the respondents’
families) of more children in Primary 4 to Primary
6 (OR=0.28, 95% CI=0.12-0.63; P=0.002), a history
of discussing STD prevention with their children
(OR=0.23, 95% CI=0.08-0.64; P=0.005), receipt of
regular seasonal influenza vaccines (OR=0.15, 95%
CI=0.04-0.48; P=0.002), child’s receipt of regular
seasonal influenza vaccines (OR=0.25, 95% CI=0.08-0.80; P=0.021), and stronger beliefs that ‘my child can
be protected from HPV without HPV vaccination’
(OR=0.28, 95% CI=0.11-0.66; P=0.005) [Table 3].
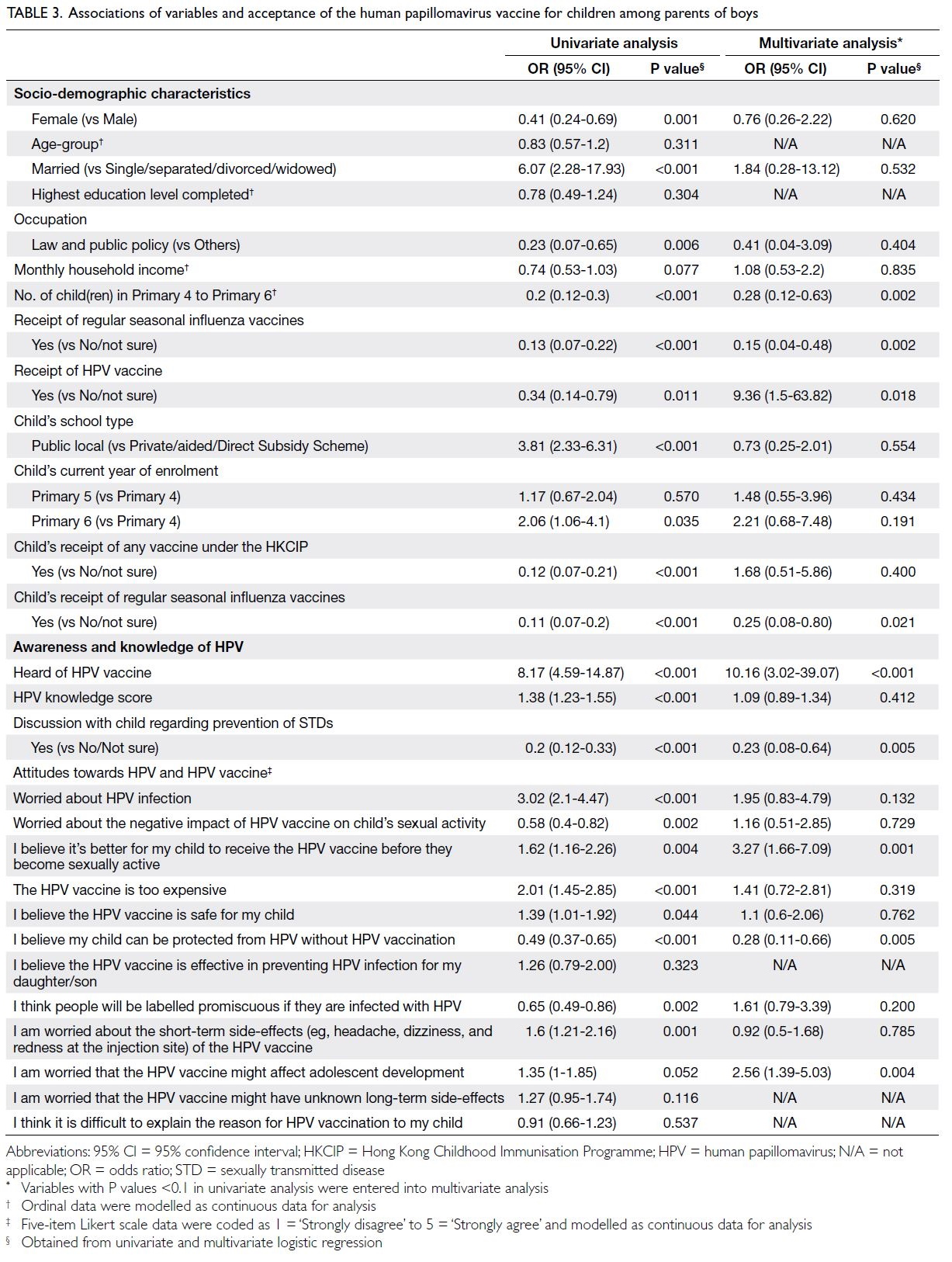
Table 3. Associations of variables and acceptance of the human papillomavirus vaccine for children among parents of boys
Regarding girls’ parents, 19 study variables were
entered into multivariate logistic regression. Higher
acceptance of the HPV vaccine for their children was
associated with higher monthly household income
(OR=4.3, 95% CI=1.95-10.47; P=0.001) and the
combined variable ‘worried about HPV infection’
(OR=2.39, 95% CI=1.08-5.73; P=0.038). Older age-group
(OR=0.38, 95% CI=0.17-0.82; P=0.018) was
the only variable associated with lower acceptance
of the HPV vaccine (Table 4).
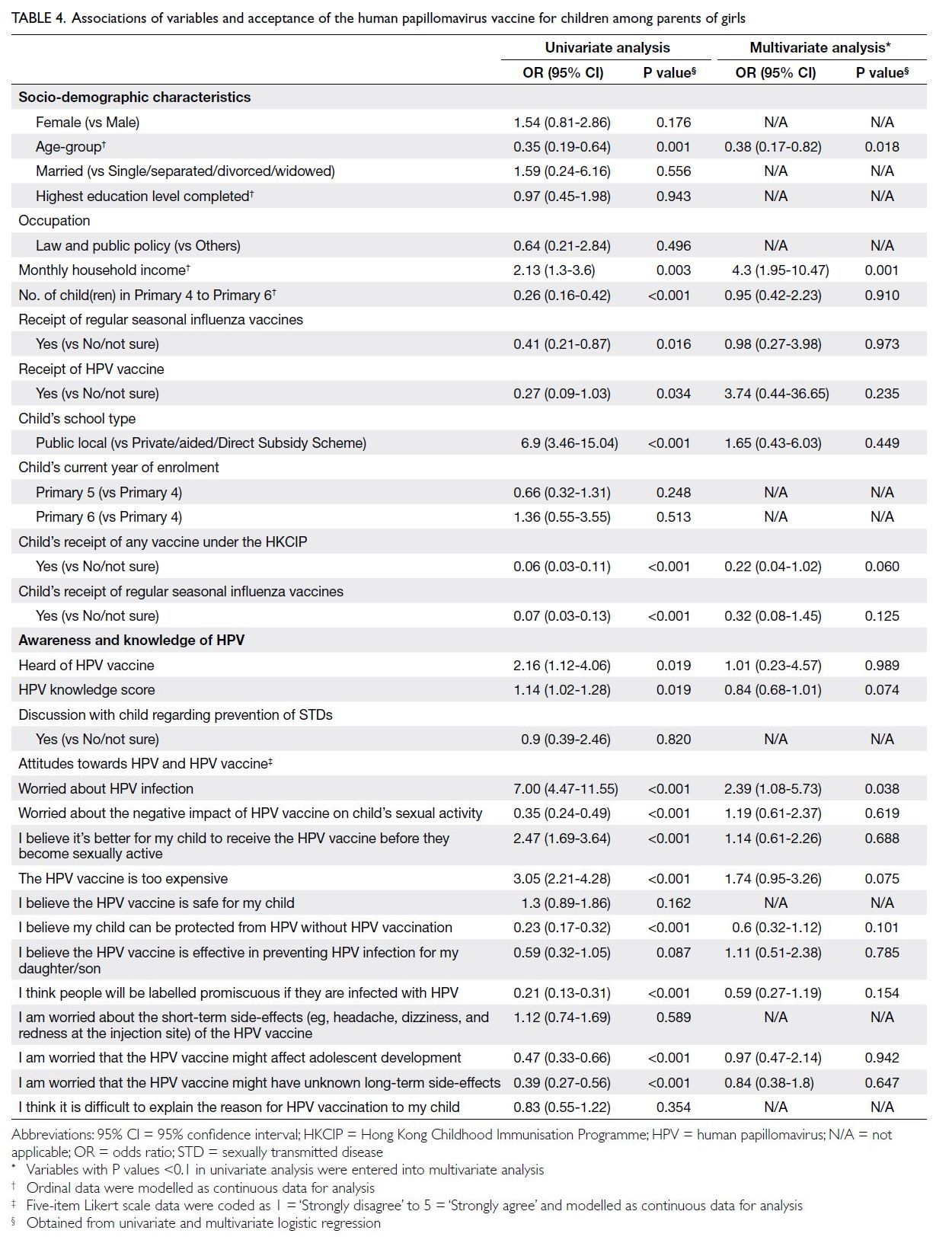
Table 4. Associations of variables and acceptance of the human papillomavirus vaccine for children among parents of girls
Discussion
This survey of 844 Hong Kong parents (370 boys’
parents and 474 girls’ parents) revealed high HPV
vaccine awareness but relatively low knowledge of
HPV and the HPV vaccine. Parents believed the
vaccine was safe and effective in preventing HPV
infection. Acceptance of the HPV vaccine was lower
among boys’ parents than among girls’ parents,
and factors associated with acceptance differed
between the two parent groups. Differences in socio-demographic
characteristics were observed, such
that more boys’ parents discussed STDs with their
children and had experience with regular seasonal
influenza vaccines, the HPV vaccine, and Pap smears.
Understanding of human papillomavirus and the vaccine
Although a majority of parents of both sexes had
knowledge of the HPV vaccine, their average scores
indicated a low overall understanding of HPV and
HPV vaccination. This finding is consistent with
the results of previous studies, which showed that
general knowledge and awareness of HPV among
parents in Hong Kong remain low despite some
improvement over time.14 15 16 18 19 20 Considering the
substantial healthcare burden associated with HPV-related
diseases in Hong Kong, there is an urgent
need for educational or promotional programmes to
enhance vaccine acceptance and uptake.
In our study, parents expressed concern
about HPV infection and strongly favoured HPV
vaccination for their children before the children
became sexually active. These beliefs support
educational and promotional campaigns targeting
the early adolescent age-group.
The reported HPV vaccine uptake rate is low in
both groups (6.8% in boys and 4.9% in girls). The low
vaccine uptake rate reported in girls is particularly
alarming considering the recent inclusion of the
HPV vaccine in the HKCIP and the high vaccination
rate of 85% reported in the 2019/2020 school year.17
Among those parents who reported their children of
receiving the HPV vaccine, >90% of them, including
boys’ parents, indicated that their children received
the vaccine through the HKCIP. This finding
provides evidence suggesting insufficient public
health campaigns, resulting in a lack of knowledge
among parents on the HPV vaccination programme
and the HKCIP, subsequently leading to potential
confusion among parents.
Notably, girls’ parents in our study reported a
belief that the HPV vaccine is too expensive, despite
the availability of free HPV vaccination through the
HKCIP. This finding again reinforces a potential lack
of awareness regarding the Programme, possibly
due to inadequate dissemination of information
during the coronavirus disease 2019 pandemic. Similar trends have been observed in other
Western countries, where routine vaccinations
(including HPV vaccination) were disrupted by the
pandemic.21 22 Catch-up vaccination services for
affected children should be implemented promptly
to prevent future healthcare burdens.23 24 25 26
Concern for cost and vaccine safety
This study examined the factors influencing parental
acceptance of HPV vaccination for boys and girls.
Parents who had more children in Primary 4 to 6
were less likely to accept the vaccine, possibly due
to cost concerns. Discussions with children about
STD prevention and previous receipt of seasonal
flu vaccines did not lead to higher acceptance
rates. These findings imply that vaccination is not
a common topic in STD prevention campaigns, a
point that warrants attention in future educational
efforts focused on STD prevention. Intriguingly,
parents with greater concern that the HPV vaccine
affects adolescent development were more likely
to accept it; they also had higher knowledge and
awareness of HPV (online supplementary Table 3).
This result highlights the need to increase parental
understanding of HPV and the HPV vaccine,
including efforts to clarify potential misconceptions
and mitigate safety concerns.
Our data indicate that parental concerns
about HPV infection strongly influence vaccine
acceptance, whereas concerns about genital warts
and HPV-related cancers are less impactful. This
discrepancy may be attributed to an optimistic bias,
where parents associate HPV complications with
promiscuity and believe that their children have low
STD risk.18
Notably, parents ranked HPV vaccine
recommendations from healthcare professionals,
relatives and friends, and schools as more important
reasons to accept the vaccine, compared with
recommendations by health authorities. This result
may suggest that government initiatives provide
suboptimal education concerning HPV and the HPV
vaccine.
Barriers to HPV vaccine acceptance include
costs and children’s preferences, which may explain
the discrepancies between uptake and acceptance.
Cost is a well-established barrier to vaccination
uptake. However, we note that the vaccine is free
for girls in our study population, which highlights
the importance of awareness. Health messages to
boys’ parents should emphasise the value of HPV
vaccination as a long-term investment in their
sons’ health.14 Concerns about vaccine safety and
adverse effects, as well as a lack of recommendations
from healthcare professionals or a lack of general
knowledge, may also hinder vaccine acceptance.
We found that parental knowledge of HPV and
the HPV vaccine significantly influenced decision-making in boys’ parents, indicating that educational
campaigns targeting HPV acceptance may be more
effective for these parents than for girls’ parents. This
difference might be partly related to the feminisation
of HPV, especially in Hong Kong. This phenomenon
has been observed in a regional qualitative study
focusing on men’s perceptions of HPV and HPV
vaccination.27 Because the Chinese translation of the
HPV vaccine is ‘cervical cancer vaccine’, many boys
and men in Hong Kong perceive a low risk of HPV
infection.27 28 29 In this context, campaigns or strategies
using a fear-based approach to increase the perceived
risk of HPV infection may be more effective for boys’
parents.
Limitations
This study had several limitations. First, it was a
cross-sectional study and thus provided less robust
evidence than would be obtained in a longitudinal
study. Vaccine acceptance is merely an indicator
of potential uptake, and it is unclear whether this
acceptance will be translated into action. Second, this
study relied on parents to self-report their outcomes,
and it lacked the ability to verify information
provided by participants. Third, the results may have
been influenced by volunteer bias or other selection
biases. Because the survey was self-administered,
random sampling of the general study population
could not be achieved due to intrinsic differences
between those who did and did not choose to
participate. Volunteer bias may explain the variation
in baseline characteristics between boys’ parents and
girls’ parents. This bias limits the generalisability of
the study results to the broader population. Fourth,
the use of previously validated scales or items was
limited. Previous studies were used as a reference to
construct the survey questionnaire, but questions
were not directly adapted. Although such validated
measures exist, due to the lack of research regarding
HPV and HPV vaccination, no measures have been
validated in Hong Kong.30 31
One possible future research direction
involves conducting longitudinal studies to examine
the factors affecting vaccine uptake. These studies
can produce stronger evidence and more effectively
inform strategies for improved vaccine uptake.
Furthermore, because this study only screened for
variables involved in parental decision-making, a
more thorough investigation could be done to better
understand this process. Qualitative studies (eg,
involving focus groups or interviews) can provide a
more in-depth understanding of parents’ attitudes,
perceptions, and decision-making processes
regarding HPV vaccination acceptance.
Conclusion
This study represents the most extensive local
investigation into factors affecting parental acceptance of HPV vaccination in Hong Kong after
the implementation of a school-based outreach
programme. We found that high awareness of
HPV and the HPV vaccine is predictive of vaccine
acceptance. To increase vaccination rates among
adolescents, we recommend targeted interventions
based on the identified factors, including public
education for parents and children to raise awareness
of HPV risks, the benefits of vaccination for boys,
and STD prevention. We also suggest including HPV
vaccination for boys in the HKCIP and implementing
catch-up vaccination for affected children. Extension
of the catch-up programme to school children
beyond Primary 6 should be considered to maintain
high vaccination rates.
Author contributions
All authors (except for PH Wong and EYT So) contributed to
the concept or design of the study, acquisition of the data,
analysis or interpretation of the data, drafting of the manuscript,
and critical revision of the manuscript for important
intellectual content. PH Wong and EYT So contributed to the
concept and design of the study questionnaire. All authors
had full access to the data, contributed to the study, approved
the final version for publication, and take responsibility for its
accuracy and integrity.
Conflicts of interest
PH Wong and EYT So are employees of Merck Sharp and
Dohme (Asia) Ltd. Other authors have disclosed no conflicts
of interest.
Acknowledgement
The authors thank Dr Ka-yu Tse from the Division of
Gynaecology Oncology of the Department of Obstetrics and
Gynaecology of The University of Hong Kong for review of
survey questions.
Funding/support
This research was sponsored by Merck Sharp & Dohme LLC,
a subsidiary of Merck & Co, Inc (Rahway [NJ], United States)
[Ref No.: NIS009837]. The sponsor had no role in collection,
analysis, or interpretation of the data, nor did it participate in
manuscript preparation.
Ethics approval
This study was approved by the Institutional Review Board of
The University of Hong Kong/Hospital Authority Hong Kong
West Cluster, Hong Kong (Ref No.: UW21-574). Participants
provided informed consent via the online survey platform
before survey completion.
Supplementary material
The supplementary material was provided by the authors and
some information may not have been peer reviewed. Accepted
supplementary material will be published as submitted by the
authors, without any editing or formatting. Any opinions
or recommendations discussed are solely those of the
author(s) and are not endorsed by the Hong Kong Academy
of Medicine and the Hong Kong Medical Association. The Hong Kong Academy of Medicine and the Hong Kong
Medical Association disclaim all liability and responsibility
arising from any reliance placed on the content.
References
1. de Martel C, Plummer M, Vignat J, Franceschi S. Worldwide
burden of cancer attributable to HPV by site, country and
HPV type. Int J Cancer 2017;141:664-70. Crossref
2. Hong Kong Cancer Registry, Hospital Authority, Hong
Kong SAR Government. Cervical Cancer in 2017. October
2019. Available from: https://www3.ha.org.hk/cancereg/pdf/factsheet/2017/cx_2017.pdf. Accessed 10 Feb 2022.
3. Centre for Health Protection, Department of Health, Hong
Kong SAR Government. Cervical Cancer. 2024 January 12.
Available from: https://www.chp.gov.hk/en/healthtopics/content/25/56.html. Accessed 9 Sep 2024.
4. Lin C, Lau JT, Ho KM, Lau MC, Tsui HY, Lo KK. Incidence
of genital warts among the Hong Kong general adult
population. BMC Infect Dis 2010;10,272. Crossref
5. Garland SM, Kjaer SK, Muñoz N, et al. Impact and
effectiveness of the quadrivalent human papillomavirus
vaccine: a systematic review of 10 years of real-world
experience. Clin Infect Dis 2016;63:519-27. Crossref
6. World Health Organization. Human papillomavirus
vaccines: WHO position paper, May
2017-Recommendations. Vaccine 2017;35:5753-5. Crossref
7. Markowitz LE, Hariri S, Lin C, et al. Reduction in human
papillomavirus (HPV) prevalence among young women
following HPV vaccine introduction in the United States,
National Health and Nutrition Examination Surveys, 2003-2010. J Infect Dis 2013;208:385-93. Crossref
8. Elfström KM, Lazzarato F, Franceschi S, Dillner J, Baussano I.
Human papillomavirus vaccination of boys and extended
catch-up vaccination: effects on the resilience of programs.
J Infect Dis 2016;213:199-205. Crossref
9. Lehtinen M, Gray P, Louvanto K, Vänskä S. In 30 years,
gender-neutral vaccination eradicates oncogenic human
papillomavirus (HPV) types while screening eliminates
HPV-associated cancers. Expert Rev Vaccines 2022;21:735-8.Crossref
10. Division of Cancer Epidemiology & Genetics, National
Cancer Institute. HPV vaccine may provide men with herd
immunity against oral HPV infections. 2019 October 10.
Available from:
https://dceg.cancer.gov/news-events/news/2019/hpv-vaccine-herd-immunity. Accessed 10 Feb 2022.
11. Kahn JA, Brown DR, Ding L, et al. Vaccine-type human
papillomavirus and evidence of herd protection after
vaccine introduction. Pediatrics 2012;130:e249-56. Crossref
12. Merriel SW, Nadarzynski T, Kesten JM, Flannagan C,
Prue G. ‘Jabs for the boys’: time to deliver on HPV
vaccination recommendations. Br J Gen Pract 2018;68:406-7. Crossref
13. Brisson M, Bénard É, Drolet M, et al. Population-level
impact, herd immunity, and elimination after human
papillomavirus vaccination: a systematic review and
meta-analysis of predictions from transmission-dynamic
models. Lancet Public Health 2016;1:e8-17. Crossref
14. Wang Z, Wang J, Fang Y, et al. Parental acceptability of HPV
vaccination for boys and girls aged 9-13 years in China—a
population-based study. Vaccine 2018;36:2657-65. Crossref
15. Li SL, Lau YL, Lam TH, Yip PS, Fan SY, Ip P. HPV
vaccination in Hong Kong: uptake and reasons for non-vaccination
amongst Chinese adolescent girls. Vaccine
2013;31:5785-8. Crossref
16. Choi HC, Leung GM, Woo PP, Jit M, Wu JT. Acceptability
and uptake of female adolescent HPV vaccination in
Hong Kong: a survey of mothers and adolescents. Vaccine
2013;32:78-84. Crossref
17. Hong Kong SAR Government. LCQ10: human
papillomavirus vaccination programme. 2021 January
20. Available from: https://www.info.gov.hk/gia/general/202101/20/P2021012000507.htm. Accessed 13 Feb 2022.
18. Wang LD, Lam WW, Fielding R. Determinants of human
papillomavirus vaccination uptake among adolescent girls:
a theory-based longitudinal study among Hong Kong
Chinese parents. Prev Med 2017;102:24-30. Crossref
19. Jones CL, Jensen JD, Scherr CL, Brown NR, Christy K,
Weaver J. The Health Belief Model as an explanatory
framework in communication research: exploring
parallel, serial, and moderated mediation. Health Comm
2015;30:566-76. Crossref
20. Chen JM, Leung DY. Factors associated with human
papillomavirus vaccination among Chinese female
university students in Hong Kong. Am Int J Soc Sci
2014;3:56-62.
21. Silva TM, Nogueira de Sá AC, Beinner MA, et al. Impact
of the COVID-19 pandemic on human papillomavirus
vaccination in Brazil. Int J Public Health 2022;67:1604224. Crossref
22. Damgacioglu H, Sonawane K, Chhatwal J, et al. Long-term
impact of HPV vaccination and COVID-19 pandemic on
oropharyngeal cancer incidence and burden among men
in the USA: a modeling study. Lancet Reg Health Am
2022;8:100143. Crossref
23. Shet A, Carr K, Danovaro-Holliday MC, et al. Impact of the
SARS-CoV-2 pandemic on routine immunisation services:
evidence of disruption and recovery from 170 countries
and territories. Lancet Glob Health 2022;10:e186-94. Crossref
24. Ryan G, Gilbert PA, Ashida S, Charlton ME, Scherer A,
Askelson NM. Challenges to adolescent HPV vaccination
and implementation of evidence-based interventions to
promote vaccine uptake during the COVID-19 pandemic:
“HPV is probably not at the top of our list”. Prev Chronic
Dis 2022;19:E15. Crossref
25. Ogilvie GS, Remple VP, Marra F, et al. Intention of
parents to have male children vaccinated with the human
papillomavirus vaccine. Sex Transm Infect 2008;84:318-23. Crossref
26. Karafillakis E, Simas C, Jarrett C, et al. HPV vaccination in
a context of public mistrust and uncertainty: a systematic
literature review of determinants of HPV vaccine hesitancy
in Europe. Hum Vaccin Immunother 2019;15:1615-27. Crossref
27. Siu JY, Fung TK, Leung LH. Barriers to receiving HPV
vaccination among men in a Chinese community: a
qualitative study in Hong Kong. Am J Mens Health
2019;13:1557988319831912. Crossref
28. Holman DM, Benard V, Roland KB, Watson M, Liddon N,
Stokley S. Barriers to human papillomavirus vaccination
among US adolescents: a systematic review of the literature.
JAMA Pediatr 2014;168:76-82. Crossref
29. Trim K, Nagji N, Elit L, Roy K. Parental knowledge,
attitudes, and behaviours towards human papillomavirus
vaccination for their children: a systematic review from
2001 to 2011. Obstet Gynecol Int 2012;2012:921236. Crossref
30. Waller J, Ostini R, Marlow LA, McCaffery K, Zimet G.
Validation of a measure of knowledge about human
papillomavirus (HPV) using item response theory and
classical test theory. Prev Med 2013;56:35-40. Crossref
31. Perez S, Tatar O, Ostini R, et al. Extending and validating
a human papillomavirus (HPV) knowledge measure in a
national sample of Canadian parents of boys. Prev Med
2016;91:43-9. Crossref


