Hong Kong Med J 2024 Oct;30(5):362–70 | Epub 3 Oct 2024
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Mental health among parents and their children
with eczema in Hong Kong
PH Lam, MSSc, GMBPsS1; KL Hon, MB, BS, MD1,2; Steven Loo, MB, ChB, FRCP2; CK Li, MB, BS, MD1,3; Patrick Ip, MB, BS, FRCPCH4; Mark J Koh, MB, BS, MRCPCH5; Celia HY Chan, PhD, RSW6
1 Department of Paediatrics, The Chinese University of Hong Kong, Hong Kong SAR, China
2 Hong Kong Institute of Integrative Medicine, The Chinese University of Hong Kong, Hong Kong SAR, China
3 Hong Kong Hub of Paediatric Excellence, The Chinese University of Hong Kong, Hong Kong SAR, China
4 Department of Paediatrics and Adolescent Medicine, The University of Hong Kong, Hong Kong SAR, China
5 Dermatology Service, KK Women’s and Children’s Hospital, SingHealth Group, Singapore
6 Department of Social Work, Melbourne School of Health Sciences, Faculty of Medicine, Dentistry and Health Sciences, The University of Melbourne, Australia
Corresponding author: Dr KL Hon (ehon@hotmail.com)
Abstract
Introduction: This cross-sectional survey research
investigated mental health symptoms and quality of
life among Chinese parents and their children with
eczema at a paediatric dermatology clinic in Hong
Kong from November 2018 to October 2020.
Methods: Health-related quality of life, eczema
severity, and mental health among children with
eczema, as well as their parents’ mental health,
were studied using the Children’s Dermatology Life
Quality Index (CDLQI), Infants’ Dermatitis Quality
of Life Index (IDQOL), Nottingham Eczema Severity
Score (NESS), Patient-Oriented Eczema Measure
(POEM), and the Chinese version of the 21-item
Depression, Anxiety, and Stress Scales (DASS-21).
Results: In total, 432 children and 380 parents
were recruited. Eczema severity (NESS and POEM)
and health-related quality of life (CDLQI) were
significantly positively associated with parental and
child depression, anxiety, and stress levels according
to the DASS-21, regardless of sex (children: r=0.28-
0.72, P<0.001 to 0.007; parents: r=0.20-0.52, P<0.001
to 0.034). Maternal depression was marginally
positively associated with increased anxiety in boys
with eczema (r=0.311; P=0.045). Younger parents
had higher risk of developing more anxiety and
stress compared with the older parents (adjusted
odds ratio [aOR]=-0.342, P=0.014 and aOR=-0.395,
P=0.019, respectively). Depression level of parents
with primary to secondary education was 58%
higher than their counterparts with post-secondary
education or above (aOR=-1.579; P=0.007).
Conclusion: Depression, anxiety, and stress among
children with eczema and their parents were
associated with eczema severity and impaired quality
of life in those children. These findings regarding
impaired mental health in children with eczema and
their parents highlight the need to include mental
well-being and psychosocial outcomes in future
studies and clinical practice.
New knowledge added by this study
- Depression, anxiety, and stress among children with eczema and their parents were associated with eczema severity and impaired quality of life in those children.
- Higher parental education level and advanced parental age could be the protective factors in dealing with emotional distress among parents whose children had eczema.
- The findings regarding impaired mental health in children with eczema and their parents highlight the need to include mental well-being and psychosocial outcomes in future studies and clinical practice.
Introduction
Atopic eczema (AE) is a common childhood
skin disease associated with pruritus and sleep
disturbance.1 2 3 4 5 Childhood AE can substantially
influence quality of life (QOL) among affected
children and their parents. The extent of QOL
impairment is often correlated with eczema severity, skin dehydration, and staphylococcal
infection.6 Additionally, many affected children
and their parents develop depression, anxiety, and
stress symptoms.1 These mental health issues are
correlated with disease severity, impaired QOL,
and therapeutic non-compliance.1 7 8 A study using
the 42-item Depression, Anxiety, and Stress Scales (DASS-42) found that depression, anxiety, and stress
symptoms were present in 21%, 33%, and 23% of Hong
Kong adolescent patients with AE, respectively.1
These psychological symptoms were significantly
correlated with poor QOL.1 A study of Japanese
children showed eczema severity was associated
with mental health.9 Furthermore, a retrospective,
cross-sectional population-based survey of
childhood eczema in the United States revealed
that increased eczema severity was associated with
a higher risk of mental disorders.10 School-aged
children with moderate and severe AE have a higher
risk of psychosocial problems that can influence
their quality of sleep and cognitive development.11
Emotion, attention, interpersonal relationships, and
conduct can also be affected by AE.10 12 Moreover,
parents are often unaware of potential psychosocial
health issues in their children with eczema.13 Most
affected children and their parents do not receive
appropriate psychological help and support; they
also exhibit low symptom recognition. The impacts
of childhood eczema on the parent-child dyad have not been extensively studied in terms of healthrelated
quality of life (HRQOL), eczema severity, or
mental health status.14
This study was performed to examine
associations between mental health issues and
disease severity in children or adolescents with AE
and their parents using the concise validated 21-item
Chinese version of DASS-42 (DASS-21).1 15 16 17
Methods
Study design and participant recruitment
This 2-year cross-sectional survey was conducted
between November 2018 and October 2020.
Participants with a diagnosis of AE and their parents
were recruited at the paediatric dermatology clinic
of a university-affiliated hospital in Hong Kong.
Eczema was clinically diagnosed in accordance with
the United Kingdom Working Party’s Diagnostic
Criteria for Atopic Dermatitis.18 Participants
and their parents received information about the
study including objectives, procedures, voluntary
participation, and right of withdrawal. Non-Chinese
participants and individuals aged <11 years who were
not accompanied by a parent during recruitment
were excluded from the study.
The questionnaires were self-administered
and supervised by research staff. Parents would help
complete the Children’s Dermatology Life Quality
Index (CDLQI), Infants’ Dermatitis Quality of Life
Index (IDQOL), Nottingham Eczema Severity Score
(NESS), and Patient-Oriented Eczema Measure
(POEM) for their younger children. The DASS-21
was individually administered to all parents and to
children aged >11 years.
Clinical assessment of eczema
The validated Chinese version of the three-item NESS,
completed by children aged >11 years or the parents
of children aged ≤11 years, was used to determine
eczema severity in participating children.19 20 The
presence of eczema and number of nights affected by
skin itchiness each week in the past 12 months were
rated from 1 to 5. A higher score indicated greater
eczema severity. Additionally, areas of skin with
eczematous lesions (eg, rash, lichenified skin, and/or
bleeding) were recorded. Scores on the NESS were
categorised as mild (3 to 8), moderate (9 to 11), and
severe (12 to 15) eczema. Subjective measurements
were determined using the validated seven-item
Chinese translation of the POEM, which was also
completed by children aged >11 years or the parents
of children aged ≤11 years.21 22 Each item was scored
from 0 to 4, with a maximum aggregate score of 28.
A higher score indicated greater eczema severity in
the past week (ranges of 0-2, 3-7, 8-16, 17-24, and
25-28 correspond to clear, mild, moderate, severe,
and very severe levels of eczema, respectively).
Assessment of health-related quality of life
Health-related QOL was evaluated using the
Chinese version of the 10-item CDLQI23 and the
10-item IDQOL.24 The CDLQI was completed by
children aged ≥4 years with guidance from parents,
whereas the IDQOL was completed by parents of
children aged <4 years. Each item on the two scales
was scored from 0 to 3, with a maximum aggregate
score of 30. A higher score indicated greater eczema-related
HRQOL impairment in the past week
(CDLQI ranges of 0-1, 2-6, 7-12, 13-18, and 19-30
correspond to no, small, moderate, very large, and
extremely large effects on HRQOL, respectively;
these ranges for IDQOL are 0-1, 2-5, 6-10, 11-20,
and 21-30, respectively).
Assessment of mental health
Mental health was assessed by measuring depression,
anxiety, and stress in children with eczema and
their parents using the validated Chinese version of
the DASS-21. This scale has been used to examine
symptoms of depression, anxiety, and stress
among individuals with dermatitis or eczema.1 17
The DASS-21 was individually administered to
all parents and to children aged >11 years. The
DASS-21 composite score can be divided into the
DASS Depression, DASS Anxiety, and DASS Stress
domains. The total score for each domain ranges from
0 to 42.25 A higher score indicates greater emotional distress in that domain (DASS Depression ranges of 0-9, 10-13, 14-20, 21-27, and ≥28 correspond
to normal, mild, moderate, severe, and extremely
severe levels, respectively; these ranges for DASS
Anxiety are 0-7, 8-9, 10-14, 15-19, and ≥20, whereas
they are 0-14, 15-18, 19-25, 26-33, and ≥34 for DASS
Stress).
Statistical analysis
Clinical data were de-identified and analysed using
SPSS (Windows version 25.0; IBM Corp, Armonk
[NY], United States). Frequency distributions were
used to describe the demographic and clinical
characteristics of participants. Continuous variables
with normal distributions were expressed as means±standard deviations (corrected to 1 decimal place).
Nominal and ordinal variables were expressed in
numbers with percentage (corrected to 1 decimal
place). Independent samples t tests were used to
explore sex differences regarding age, education
level, disease severity, QOL, and emotional distress
in parents and children. Pearson correlation analysis
was utilised to examine associations among mental
health, eczema severity, and HRQOL in parents and
children of both sexes. Multiple linear regression
was performed to adjust for variations in parental
and child DASS scores and HRQOL according to
demographic and clinical variables. P values <0.05
were considered statistically significant.
Results
Demographic information, disease state, and mental well-being among children and parents
Among 380 parents (mean age=41.13±6.52 years), 49 were fathers (mean age=42.50±7.49 years) and 331 were mothers (mean age=40.95±6.36 years).
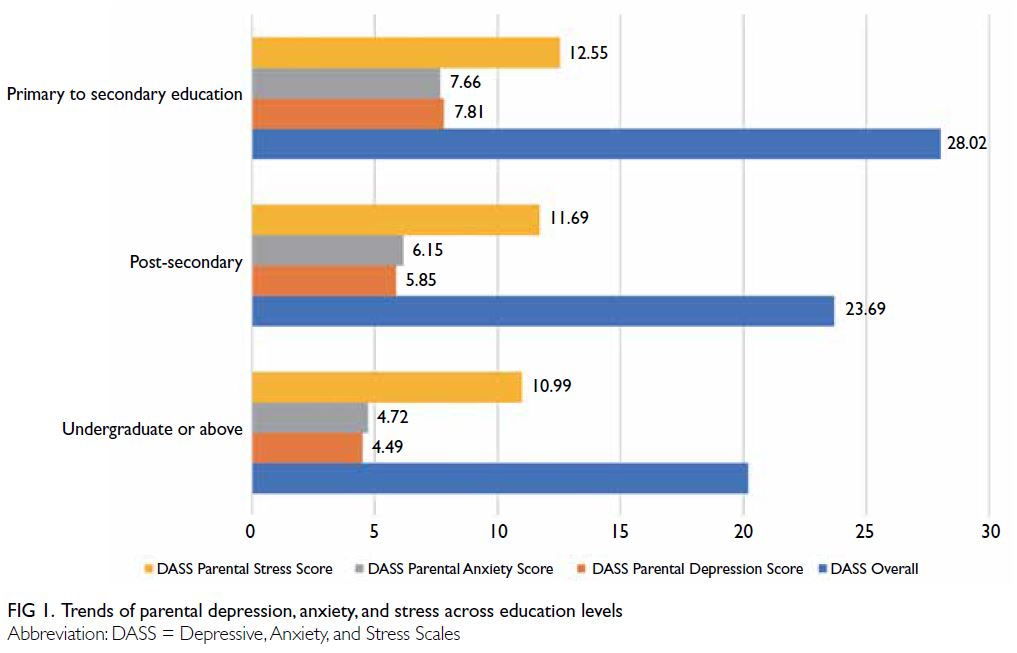
Parents’ education levels were primary to secondary
(n=124, 13 males), post-secondary (n=26, 1 male),
and undergraduate or above (n=81, 14 males) [Table 1]. Parents reported moderate to extremely severe
depression (n=58, 2 males), moderate to extremely
severe anxiety (n=101, 5 males), and moderate to
extremely severe stress (n=90, 6 males). Parents
with a higher education level had lower levels of
depression, anxiety, and stress (Fig 1). Compared
with fathers, mothers generally had higher overall
DASS-21 depression, anxiety, and stress scores
(P<0.001-0.005) [Table 1].
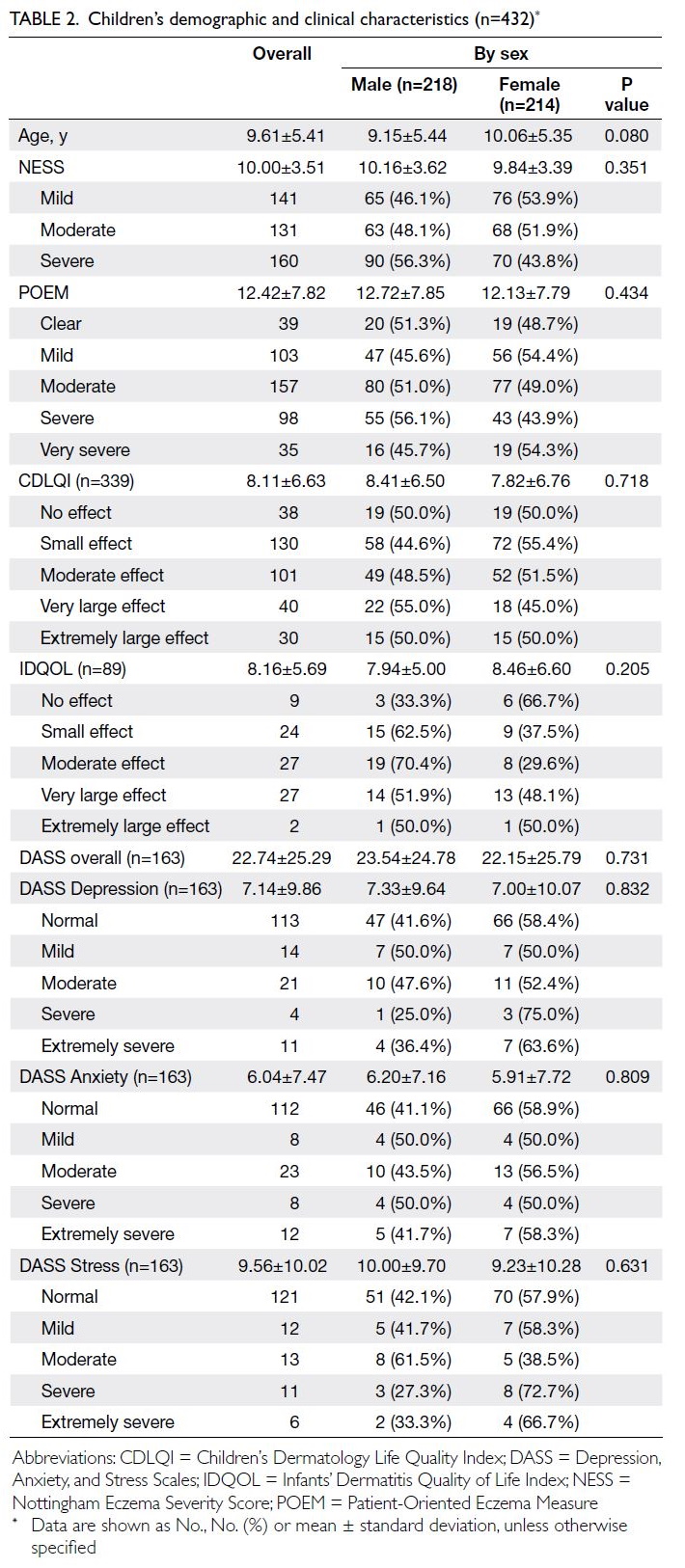
Among 432 children (mean age=9.61±5.41
years), 218 were boys (mean age=9.15±5.44 years)
and 214 were girls (mean age=10.06±5.35 years).
Most children had moderate to severe/very severe
disease according to the POEM (n=290) and NESS
(n=291). Over half of the children displayed a
moderate to extremely large impact on QOL in the
CDLQI (n=171, 50.4%) and IDQOL (n=56, 62.9%).
Small numbers of children had moderate to extremely
severe depression (n=36), anxiety (n=43), and stress
(n=30). There were no significant sex differences in
disease severity, HRQOL, or emotional distress in
the DASS (Table 2).
Eczema severity, health-related quality of life, and mental health among children
Disease severity in terms of NESS, POEM, and HRQOL (ie, CDLQI and IDQOL) was generally
worse among infants than among older children
(Fig 2). Thus, eczema severity and QOL generally
appeared to improve with age. Correlation analysis
demonstrated that depression, anxiety, and stress
levels were significantly associated with NESS,
POEM, and CDLQI, regardless of sex (Table 3).
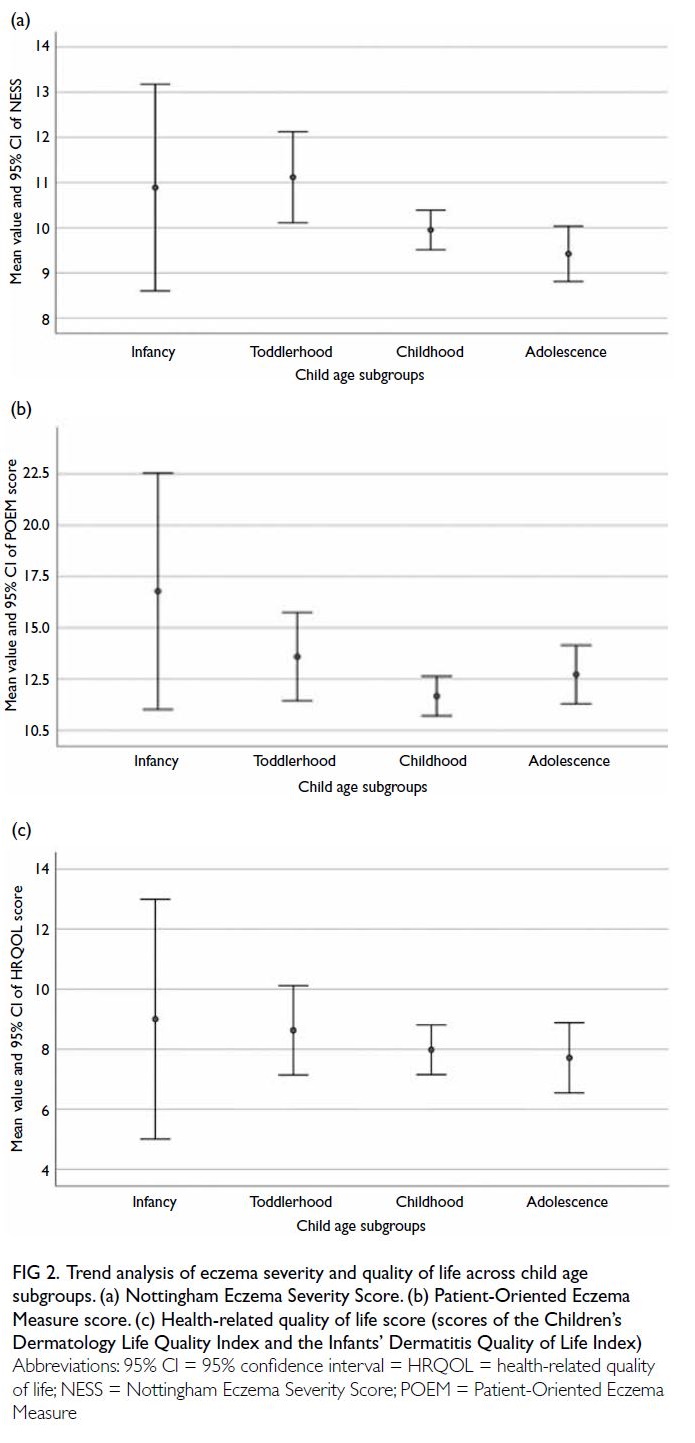
Figure 2. Trend analysis of eczema severity and quality of life across child age subgroups. (a) Nottingham Eczema Severity Score. (b) Patient-Oriented Eczema Measure score. (c) Health-related quality of life score (scores of the Children’s Dermatology Life Quality Index and the Infants’ Dermatitis Quality of Life Index)
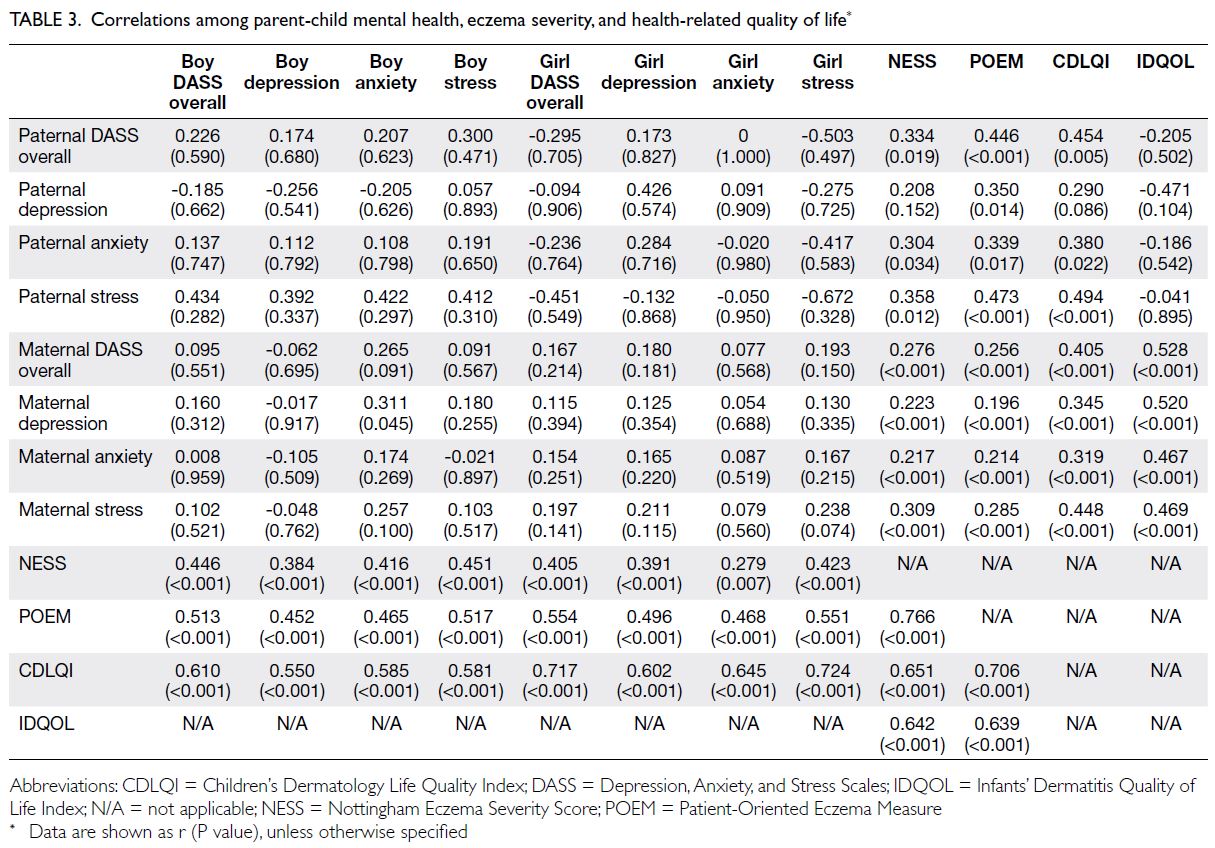
Table 3. Correlations among parent-child mental health, eczema severity, and health-related quality of life
Eczema severity, health-related quality of
life, and mental health among parents
Correlation analysis revealed that eczema severity
(NESS and POEM) and HRQOL (CDLQI) were
associated with depression, anxiety, and stress levels
(DASS-21) among children and parents, regardless
of sex (Table 3 and Fig 3). Moreover, depression,
anxiety, and stress levels in mothers were significantly
correlated with NESS, POEM, IDQOL, and CDLQI.
Paternal anxiety and stress levels were correlated
with NESS, POEM, and CDLQI (P<0.001 to 0.034).
However, paternal depression was only correlated
with POEM (P=0.014) [Table 3].
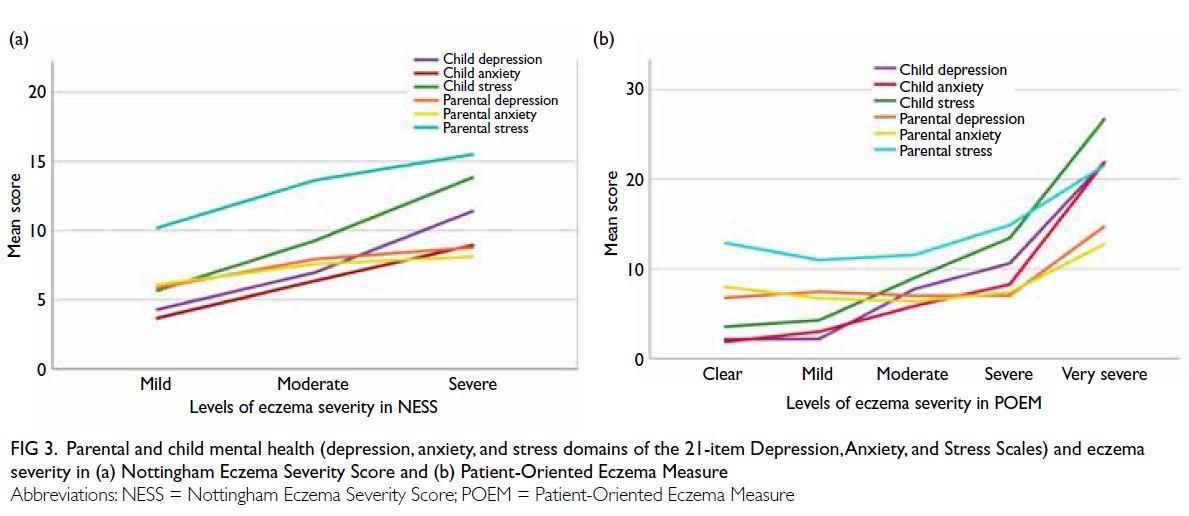
Figure 3. Parental and child mental health (depression, anxiety, and stress domains of the 21-item Depression, Anxiety, and Stress Scales) and eczema severity in (a) Nottingham Eczema Severity Score and (b) Patient-Oriented Eczema Measure
Mental health among children and parents
Maternal depression showed a marginal association
with higher anxiety levels in boys with eczema (n=42,
r=0.311; P=0.045) [Table 3]. However, considering
the small number of pairs, no clinical or statistical inferences should be made regarding sex differences
in mental health among children and parents.
Additionally, there were no statistically significant
associations between the mental health of children
and parents concerning depression, anxiety, and
stress levels in the DASS-21 (Table 3). Regression
analysis showed that the child’s HRQOL and
parental age mostly explained variation in parental
anxiety and stress, whereas parental education level
explained variation in parental depression (Table 4). Younger parents had higher risk of developing
more anxiety and stress compared with the older
parents. Depression level of parents with primary
to secondary education was 58% higher than their
counterparts with post-secondary education or
above. Conversely, the child’s eczema severity and
HRQOL mostly explained the child’s emotional
distress. Eczema severity and parental emotional
distress significantly affected HRQOL in children of
all ages (Table 4).
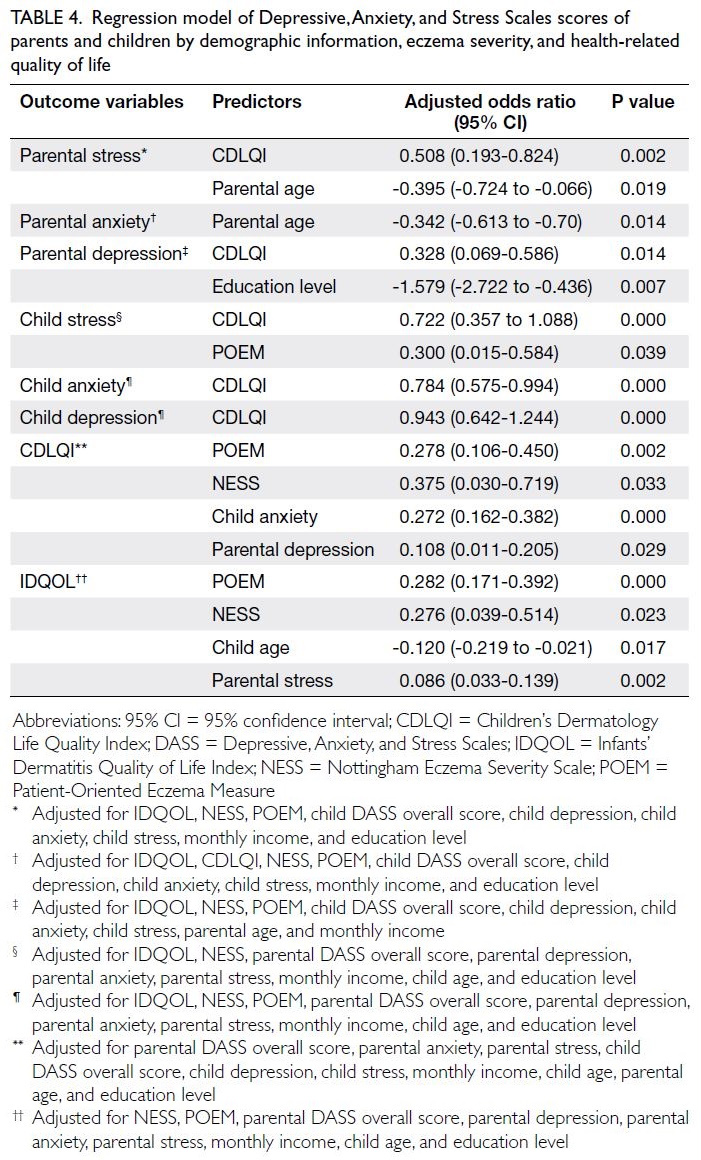
Table 4. Regression model of Depressive, Anxiety, and Stress Scales scores of parents and children by demographic information, eczema severity, and health-related quality of life
There was no psychological or physiological discomfort resulted from administration of the surveys.
Discussion
Psychological symptoms of depression, anxiety, and
stress were prevalent among children with AE and
their parents. Our findings indicate associations
between the mental health of children and parents
and the eczema severity in those children. Increased
eczema severity in children and adolescents led to
greater emotional distress in parents and children,
regardless of sex. Similarly, psychological symptoms in
children and their parents were negatively correlated
with the child’s eczema severity (NESS and POEM)
and HRQOL impairment (CDLQI or IDQOL),
regardless of sex. These strong correlations suggest
that psychological symptoms, eczema severity, and
impact on QOL have mutually detrimental effects.
The DASS depression, anxiety, and stress scores were
generally higher among mothers than among fathers,
suggesting that mothers (the primary caregivers for
children with eczema) were more strongly affected.
The present study showed that eczema severity can
adversely affect emotions and QOL among parents
and children, highlighting the need for further
exploration of biopsychosocial interactions among
children and adolescents with eczema. Children with
severe disease reportedly have more problems with
depression and internalising behaviour.26 Behavioural
issues can lead to adverse social interactions with
peers, further reducing self-esteem and HRQOL.
Therefore, interactions among parental perception
of the child’s disease severity, the child’s treatment
adherence, the child’s social influence by peers, and
the child’s school environment should be considered
when clinicians make comprehensive decisions
about holistic treatments.
Our results using the DASS-21 are consistent
with findings in previous studies1 27 that used the more comprehensive DASS-42. As in previous
studies,1 27 we found that caregivers were especially
likely to experience anxiety related to care provision
in the home.28 29 In the present study, maternal
depression was associated with a higher anxiety
level, particularly in relation to boys with eczema.
Accordingly, the Harmonising Outcome Measures
for Eczema initiative recommends documentation
of disease severity and QOL impairment in
eczema cases.25 30 However, there have been few
international initiatives and clinical trials regarding
the psychological symptoms of caregivers and
patients, particularly in the context of childhood
eczema. Therefore, we suggest that clinicians should
consider these important measurable domains in
terms of therapeutic interventions and psychological
support. Childhood eczema treatments mainly focus
on pharmacological control of physical symptoms,
but they often completely neglect the psychological
symptoms of affected children and their parents.
A more holistic treatment approach is needed for
this potentially devastating common childhood
disorder. Given the increasing numbers of proposed
assessment tools, we advocate a holistic and
comprehensive approach for eczema management
that considers children and their families. This
treatment tool should use a composite score to
continuously evaluate disease severity (in objective
and subjective manners), QOL impairment,
psychological symptoms, and miscellaneous
disease surrogates in affected children and their
parents.1 16 21 26
Strengths and limitations
A strength of this study was that compared with
the DASS-42, the DASS-21 demonstrated better
performance with 50% fewer questions and a shorter
completion time. Findings from the DASS-21, but
not the DASS-42, were correlated with disease
severity as measured by the NESS and POEM.1
These discrepancies could have arisen because the
sample size in the present study (using the DASS-21) was threefold greater than the sample size in
the previous DASS-42 study.1 In the present study,
the DASS-21, especially in child and mother, was
moderately to strongly correlated with the CDLQI,
IDQOL, NESS, and POEM. Thus, the DASS-21 can
effectively represent the degree of emotional distress
among parents and children or adolescents with
eczema. This questionnaire is available in different
languages, potentially allowing it to be used for
assessment of patients with other ethnicities. To our
knowledge, this is the first study to use the DASS-21
to assess the mental health of parents and children
with eczema in a paediatric setting. This study revealed the presence of childhood eczema-related
depression, anxiety, and stress in affected children
and their parents.
This study had a few limitations including its
relatively small sample size, especially concerning
father-child pairs. A greater proportion of mothers
participated in this study, which is expected because
mothers are the main caregivers for children with
eczema; they typically accompany their children
during medical consultations. Considering that
paediatric dermatological clinics also cater adolescent patients aged ≥16 years, a few participants
aged 16 to 19 years completed the CDLQI on their
HRQOL; although these participants exceeded the
suggested age range of ≤16 years, the overall results
were not affected.
Another limitation is that the number of
recruited mothers, who are normally regarded
as the main child caregiver, much outweighs that
of recruited fathers. In addition, compared with
fathers, mothers may know their child’s health
more and get anxious or depressed as the eczema
severity of their child escalates over time. Thus, the
difference of the role in childbearing, sample size
and the understanding of child’s health may affect
the findings in parental-child correlations. It should
be cautious when the results regarding parental-child
correlations are studied and presented. The
CDLQI (n=339) is a questionnaire for children,
and the IDQOL (n=89) is for infants. The different
numbers of participants who completed each of
these questionnaires is consistent with the CDLQI
coverage of a broader age range, whereas the IDQOL
is only suitable for children aged <4 years. Although
maternal depression was correlated with boys
with anxiety, it is important to note that statistical
significance should not be used to infer that there
is a sex difference between parent and child groups
in terms of mental health; such an inference would
constitute overgeneralisation.
Conclusion
Children with eczema and their parents demonstrated
mental health impairment, which was correlated
with disease severity. Eczema-induced anxiety,
stress, and other mental health issues in affected
children and their parents should be considered
by healthcare professionals during comprehensive
assessments for the treatment of eczema. In addition
to primary eczema, possible secondary psychiatric
symptoms should be monitored in children with
moderate to severe eczema and their parents.
Childhood eczema severity and the mental health
of affected children and their parents should be
simultaneously evaluated to prevent and manage
secondary psychological problems.
Author contributions
Concept or design: KL Hon.
Acquisition of data: PH Lam.
Analysis or interpretation of data: PH Lam, P Ip.
Drafting of the manuscript: PH Lam, KL Hon.
Critical revision of the manuscript for important intellectual content: KL Hon, S Loo, MJ Koh, CHY Chan, CK Li, P Ip.
Acquisition of data: PH Lam.
Analysis or interpretation of data: PH Lam, P Ip.
Drafting of the manuscript: PH Lam, KL Hon.
Critical revision of the manuscript for important intellectual content: KL Hon, S Loo, MJ Koh, CHY Chan, CK Li, P Ip.
Conflicts of interest
As an editor of the journal, KL Hon was not involved in the peer review process. Other authors have disclosed no conflicts of interest.
Acknowledgement
The authors thank all children and parents who participated in this research.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This research was approved by the Joint Chinese University of Hong Kong–New Territories East Cluster Clinical Research Ethics Committee, Hong Kong (Ref No.: CRE.2018.401).
Written informed consent was obtained from participants
and parents prior to the research.
References
1. Hon KL, Pong NH, Poon TC, et al. Quality of life and
psychosocial issues are important outcome measures in
eczema treatment. J Dermatolog Treat 2015;26:83-9. Crossref
2. Leung AK, Hon KL, Robson WL. Atopic dermatitis. Adv Pediatr 2007;54:241-73. Crossref
3. Leung TN, Hon KL. Eczema therapeutics in children: what do the clinical trials say? Hong Kong Med J 2015;21:251-60. Crossref
4. Hon KL, Lam PH, Ng WG, et al. Age, sex, and disease status
as determinants of skin hydration and transepidermal
water loss among children with and without eczema. Hong
Kong Med J 2020;26:19-26. Crossref
5. Hon KL, Wong KY, Leung TF, Chow CM, Ng PC.
Comparison of skin hydration evaluation sites and
correlations among skin hydration, transepidermal water
loss, SCORAD index, Nottingham Eczema Severity Score,
and quality of life in patients with atopic dermatitis. Am J
Clin Dermatol 2008;9:45-50. Crossref
6. Holm EA, Wulf HC, Stegmann H, Jemec GB. Life quality
assessment among patients with atopic eczema. Br J
Dermatol 2006;154:719-25. Crossref
7. Slattery MJ, Essex MJ, Paletz EM, et al. Depression, anxiety,
and dermatologic quality of life in adolescents with atopic
dermatitis. J Allergy Clin Immunol 2011;128:668-71. Crossref
8. Magin PJ, Pond CD, Smith WT, Watson AB, Goode SM.
Correlation and agreement of self-assessed and objective
skin disease severity in a cross-sectional study of patients
with acne, psoriasis, and atopic eczema. Int J Dermatol
2011;50:1486-90. Crossref
9. Kuniyoshi Y, Kikuya M, Miyashita M, et al. Severity
of eczema and mental health problems in Japanese
schoolchildren: the ToMMo Child Health Study. Allergol
Int 2018;67:481-6. Crossref
10. Wan J, Takeshita J, Shin DB, Gelfand JM. Mental health
impairment among children with atopic dermatitis: a
United States population-based cross-sectional study of
the 2013-2017 National Health Interview Survey. J Am
Acad Dermatol 2020;82:1368-75. Crossref
11. Fishbein AB, Cheng BT, Tilley CC, et al. Sleep disturbance
in school-aged children with atopic dermatitis: prevalence
and severity in a cross-sectional sample. J Allergy Clin
Immunol Pract 2021;9:3120-9.e3. Crossref
12. Schmitt J, Apfelbacher C, Chen CM, et al. Infant-onset
eczema in relation to mental health problems at age
10 years: results from a prospective birth cohort study
(German Infant Nutrition Intervention plus). J Allergy Clin
Immunol 2010;125:404-10. Crossref
13. Walker C, Papadopoulos L, Hussein M. Paediatric eczema
and psychosocial morbidity: how does eczema interact
with parents’ illness beliefs? J Eur Acad Dermatol Venereol
2007;21:63-7. Crossref
14. Ali F, Vyas J, Finlay AY. Counting the burden: atopic
dermatitis and health-related quality of life. Acta Derm
Venereol 2020;100:adv00161. Crossref
15. Wong KC. Psychometric investigation into the construct
of neurasthenia and its related conditions: a comparative
study on Chinese in Hong Kong and Mainland China
[dissertation]. Hong Kong: The Chinese University of Hong
Kong; 2009.
16. Lam PH, Hon KL, Leung KK, Leong KF, Li CK, Leung TF.
Self-perceived disease control in childhood eczema. J
Dermatolog Treat 2022;33:1459-64. Crossref
17. Gong X, Xie XY, Xu R, Luo YJ. Psychometric properties
of the Chinese versions of DASS-21 in Chinese college
students [in Chinese]. Chinese J Clin Psychol 2010;18:443-6.
18. Williams HC, Burney PG, Pembroke AC, Hay RJ. The U.K.
Working Party’s Diagnostic Criteria for Atopic Dermatitis.
III. Independent hospital validation. Br J Dermatol
1994;131:406-16. Crossref
19. Emerson RM, Charman CR, Williams HC. The Nottingham
Eczema Severity Score: preliminary refinement of the Rajka
and Langeland grading. Br J Dermatol 2000;142:288-97. Crossref
20. Hon KL, Ma KC, Wong E, Leung TF, Wong Y, Fok TF.
Validation of a self-administered questionnaire in Chinese
in the assessment of eczema severity. Pediatr Dermatol
2003;20:465-9. Crossref
21. Hon KL, Kung JS, Tsang KY, Yu JW, Cheng NS, Leung TF.
Do we need another symptom score for childhood eczema?
J Dermatolog Treat 2018;29:510-4. Crossref
22. Gaunt DM, Metcalfe C, Ridd M. The Patient-Oriented
Eczema Measure in young children: responsiveness
and minimal clinically important difference. Allergy
2016;71:1620-5. Crossref
23. Salek MS, Jung S, Brincat-Ruffini LA, et al. Clinical
experience and psychometric properties of the Children’s
Dermatology Life Quality Index (CDLQI), 1995-2012. Br J
Dermatol 2013;169:734-59. Crossref
24. Lewis-Jones MS, Finlay AY, Dykes PJ. The Infants’
Dermatitis Quality of Life Index. Br J Dermatol
2001;144:104-10. Crossref
25. Gerbens LA, Prinsen CA, Chalmers JR, et al. Evaluation
of the measurement properties of symptom measurement
instruments for atopic eczema: a systematic review. Allergy
2017;72:146-63. Crossref
26. Hon KL, Kam WY, Lam MC, Leung TF, Ng PC. CDLQI,
SCORAD and NESS: are they correlated? Qual Life Res
2006;15:1551-8. Crossref
27. Duran S, Atar E. Determination of depression, anxiety and
stress (DAS) levels in patients with atopic dermatitis: a
case-control study. Psychol Health Med 2020;25:1153-63. Crossref
28. Shelley AJ, McDonald KA, McEvoy A, et al. Usability,
satisfaction, and usefulness of an illustrated eczema action
plan. J Cutan Med Surg 2018;22:577-82. Crossref
29. Rork JF, Sheehan WJ, Gaffin JM, et al. Parental response to
written eczema action plans in children with eczema. Arch
Dermatol 2012;148:391-2. Crossref
30. Spuls PI, Gerbens LA, Simpson E, et al. Patient-Oriented
Eczema Measure (POEM), a core instrument to measure
symptoms in clinical trials: a Harmonising Outcome
Measures for Eczema (HOME) statement. Br J Dermatol
2017;176:979-84. Crossref