© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
REMINISCENCE: ARTEFACTS FROM THE HONG KONG MUSEUM OF MEDICAL SCIENCES
The use of external pelvimetry in 1948
Stephanie Adams, MD, MWomHMed1,2; CP Lee, FRCOG, FHKAM (Obstetrics and Gynaecology)1,3; Elce Au Yeung, MN, DN1,4; WC Leung, MD, FHKAM (Obstetrics and Gynaecology)1,2
1 Education and Research Committee, Hong Kong Museum of Medical Sciences
2 Department of Obstetrics and Gynaecology, Kwong Wah Hospital, Hong Kong SAR, China
3 Department of Obstetrics and Gynaecology, Tsan Yuk Hospital, Hong Kong SAR, China
4 School of Midwifery, Department of Obstetrics and Gynaecology, Prince of Wales Hospital, Hong Kong SAR, China
A sequel to our previous article which discusses
senior midwife Mrs Kai-ying Poon Yam’s casebook
detailing the 30 births she attended while on
placement at Tsan Yuk Hospital between 1947 and
1948,1 this article focuses on the Collin’s pelvimeter
generously donated to the Hong Kong Museum of
Medical Sciences by Dr Chiu-kwong Yu’s family
(Fig 1).
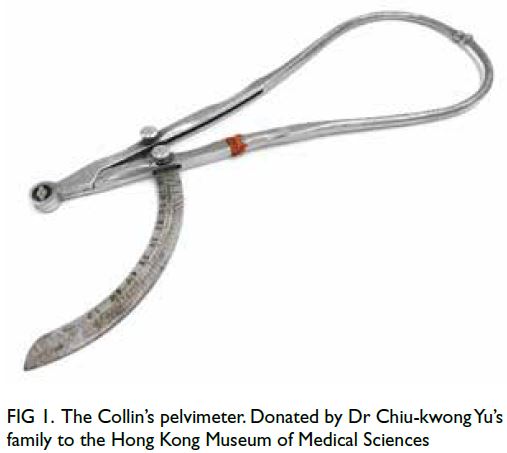
Figure 1. The Collin’s pelvimeter. Donated by Dr Chiu-kwong Yu’s family to the Hong Kong Museum of Medical Sciences
When a lady presented to the labour ward in
1948, key information—including her name, the
date of her last menstrual period and her estimated
due date—was recorded. In addition to the woman’s
vitals, routine assessment on admission involved
measuring the pelvis and the fundal height as well
as assessing the fetal presentation. Measuring the
pelvis, ie, pelvimetry, was developed by French
obstetrician Dr Jean-Louis Baudelocque in the late
1700s and requires an instrument called a pelvimeter,
of which there are different types.2
How pelvimetry was introduced to Hong Kong
in the 1940s is unclear. However, Prof Richard Edwin
Tottenham, the first Professor of Obstetrics and
Gynaecology at The University of Hong Kong, might
have played an important role in establishing its
routine practice; prior to his service in Hong Kong,
he published an article about his newly created
pelvimeter.3 External pelvimetry is no longer routine in obstetric care here.
The pelvimeter donated by Dr Yu’s family is
believed to be a Collin’s pelvimeter, possibly named
after the French manufacturing company Collin of
Paris.4 It is impossible to ascertain if the pelvimeter is
based on the original French model. The instrument
comprises two stainless steel curved probes hinged
together at one end (Fig 1). The pelvic measurement
in centimetres is read off a sliding scale attached
near the hinged end of the probes.
External pelvimetry in the 1940s was performed
by measuring the interspinous diameter, intercristal
diameter, external conjugate, and transverse outlet,
as shown in Figure 2.5 The interspinous diameter
measures the distance between the anterior superior
iliac spine, with normal values ranging from 23 to
26 cm.5 The intercristal diameter is the distance
between the iliac crests, with normal values ranging
from 25 to 28 cm.5 The external conjugate is the distance between the pubic symphysis and the
spinous process of the fifth lumbar vertebrae and
should range from 18 to 20 cm.5 Lastly, the transverse
outlet measures the distance between the ischial
tuberosities when the woman is supine, and normal
values range from 8.5 to 9.5 cm.5 Of note, whether
these normal value ranges truly reflect the standards
used in the 1940s is unconfirmed, given the lack of
relevant references from the time.
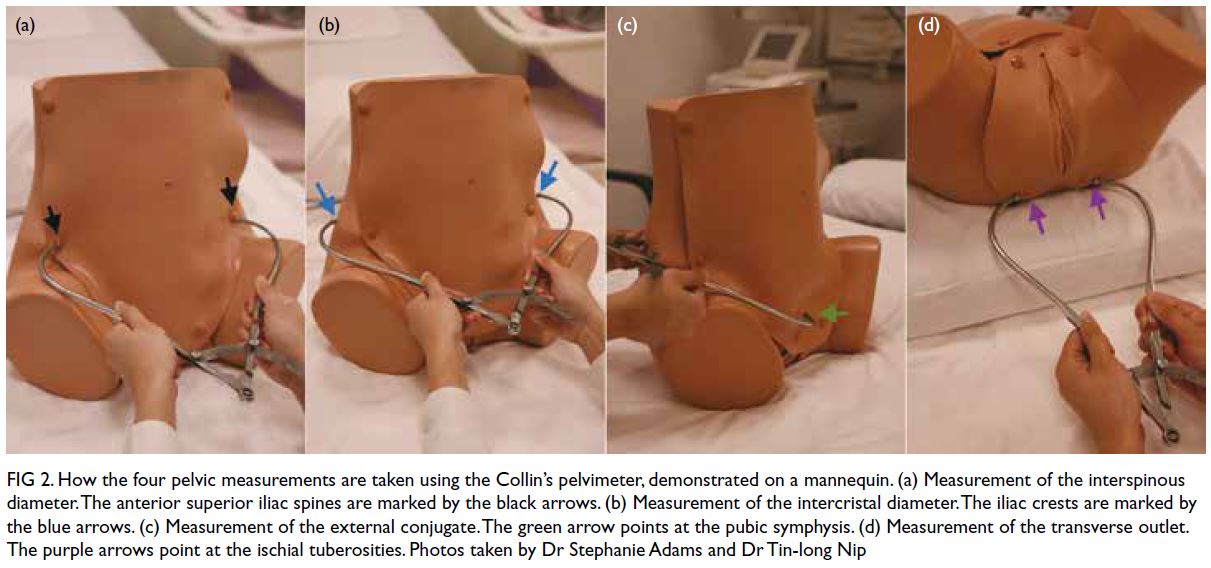
Figure 2. How the four pelvic measurements are taken using the Collin’s pelvimeter, demonstrated on a mannequin. (a) Measurement of the interspinous diameter. The anterior superior iliac spines are marked by the black arrows. (b) Measurement of the intercristal diameter. The iliac crests are marked by the blue arrows. (c) Measurement of the external conjugate. The green arrow points at the pubic symphysis. (d) Measurement of the transverse outlet. The purple arrows point at the ischial tuberosities. Photos taken by Dr Stephanie Adams and Dr Tin-long Nip
Of those 30 cases recorded in Mrs Poon’s
casebook, that of a 23-year-old multiparous lady
with a contracted pelvis exemplifies the importance
of external pelvimetry. The expectant mother had left
hip deformity secondary to tuberculosis and a history
of stillbirth requiring forceps delivery. She presented
at the hospital at 41 weeks and 3 days gestation. She
was found to have a floating fetal presentation. All
four pelvimetric measurements were shorter than
the lowest normal value. She eventually underwent a
lower segment caesarean section, performed by Prof
Gordon King and Dr B Moore. The operation was
successful and the woman delivered a healthy baby.
Over the past 80 years, obstetric practice has
witnessed many breakthroughs and improvements
in safety and the standard of care. One major change
was the introduction of evidence-based practices.
In 2018, the World Health Organization issued technical guidelines for intrapartum care to promote
a positive childbirth experience.6 Routine clinical
pelvimetry was no longer recommended for healthy
pregnant women due to insufficient supporting
evidence.6 Indeed, Prof Daphne Chun and Prof
Kin-hung Lee had recognised pelvimetry’s lack of
clinical significance a few decades before the World
Health Organization released their guidelines. As
written in their textbook Practical Obstetrics, Hong
Kong’s first bilingual obstetrics textbook, ‘External
pelvic measurements bear no constant relationship
to the actual pelvic measurements, hence external pelvimetry has now been abandoned…The best pelvimeter is the fetal head’.7
Grossly contracted pelvis was more common
in the 1940s than in modern times, because of the
higher prevalence of malnutrition and tuberculosis.
External pelvimetry helped screen for grossly
contracted pelvis, reducing the risk of obstructed
labour. Thus, the Collin’s pelvimeter improved
childbirth safety in the forties. This potentially life-saving
instrument and Mrs Poon’s casebook are great
testimonies to the development of obstetric practice
in Hong Kong.
References
1. Adams S, Lee CP, Au Yeung E, Leung WC. Travelling back to the 1940s: inspirations from a midwifery casebook written between 1947 and 1948. Hong Kong Med J 2024;30:82-4. Crossref
2. Dunn PM. Jean-Louis Baudelocque (1746–1810) of Paris and L’art des accouchemens. Arch Dis Child Fetal Neonstal Ed 2004;89:F370-2. Crossref
3. Tottenham RE. A new pelvimeter. Ir J Med Sci 1922;1:409-16. Crossref
4. Science Museum, London. Pelvimeter, Paris, France, 1860–1870. Wellcome Collection. Available from: https://www.jstor.org/stable/community.24786270. Accessed 23 Jun 2024.
5. Fan X, Zhou Z, Stewart M, et al. Comparing the pelvis of Tibetan and Chinese Han women in rural areas of China: two population-based studies using coarsened exact matching. J Obstet Gynaecol 2022;42:403-9. Crossref
6. World Health Organization. WHO recommendations: intrapartum care for a positive childbirth experience. Geneva: World Health Organization; 2018.
7. Chun WC, Lee KH. Practical Obstetrics: A Short Textbook in English and Chinese for Medical Students and Midwives. 3rd ed. Hong Kong: Hong Kong University Press; 1990: 261-2.

