Hong Kong Med J 2024 Aug;30(4):332–6 | Epub 5 Aug 2024
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
COMMENTARY
The Hong Kong Renal Registry: a recent update
John YH Chan, MB, ChB, FHKAM (Medicine)1; YL Cheng, MB, ChB, FHKAM (Medicine)2; SK Yuen, MB, ChB, FHKAM (Medicine)3; PN Wong, MB, ChB, FHKAM (Medicine)4; HM Cheng, MB, BS, FHKAM (Medicine)5; KL Mo, MB, BS, FHAKM (Medicine)6; CY Yung, MB, BS, FHKAM (Medicine)7; KM Chow, MB, ChB, FHKAM (Medicine)8; Samuel KS Fung, MB, BS, FHKAM (Medicine)9; WL Chak, MB, BS, FHKAM (Medicine)1; Maggie KM Ma, MB, BS, FHKAM (Medicine)10; TL Ho, MB, ChB, FHKAM (Medicine)11; Achilles Lee, MB, ChB, FHKAM (Medicine)12; Sunny Wong, MB, BS, FHKAM (Medicine)13; SF Cheung, MB, BS, FHKAM (Medicine)14; Alison LT Ma, MB, BS, FHKAM (Medicine)15 CC Szeto, MD, FHKAM (Medicine)16; Sydney CW Tang, MD, FHKAM (Medicine)17; SL Lui, MD, FHKAM (Medicine)18
1 Department of Medicine, Queen Elizabeth Hospital, Hong Kong SAR, China
2 Department of Medicine, Alice Ho Miu Ling Nethersole Hospital, Hong Kong SAR, China
3 Department of Medicine and Geriatrics, Caritas Medical Centre, Hong Kong SAR, China
4 Department of Medicine and Geriatrics, Kwong Wah Hospital, Hong Kong SAR, China
5 Department of Medicine, North District Hospital, Hong Kong SAR, China
6 Department of Medicine, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, China
7 Department of Medicine and Geriatrics, Pok Oi Hospital, Hong Kong SAR, China
8 Department of Medicine and Therapeutics, Prince of Wales Hospital, Hong Kong SAR, China
9 Department of Medicine and Geriatrics, Princess Margaret Hospital, Hong Kong SAR, China
10 Department of Medicine, Queen Mary Hospital, Hong Kong SAR, China
11 Department of Medicine, Tseung Kwan O Hospital, Hong Kong SAR, China
12 Department of Medicine and Geriatrics, Tuen Mun Hospital, Hong Kong SAR, China
13 Department of Medicine and Geriatrics, United Christian Hospital, Hong Kong SAR, China
14 Department of Medicine, Yan Chai Hospital, Hong Kong SAR, China
15 Department of Paediatrics and Adolescent Medicine, Hong Kong Children’s Hospital, Hong Kong SAR, China
16 Department of Medicine and Therapeutics, The Chinese University of Hong Kong, Hong Kong SAR, China
17 Department of Medicine, School of Clinical Medicine, The University of Hong Kong, Hong Kong SAR, China
18 Department of Medicine, Tung Wah Hospital, Hong Kong SAR, China
Corresponding author: Dr John YH Chan (chanyhj@ha.org.hk)
Introduction
The Hong Kong Hospital Authority (HA) provides
>90% of renal replacement services for kidney failure
with replacement therapy (KFRT) [previously termed
end-stage renal failure] patients in Hong Kong.1 The
HA Renal Registry, established in April 1995,1 is
an online computerised registry system developed
by the HA Central Renal Committee to capture
data regarding all KFRT patients with treatment
provided by the HA. Reports of the Renal Registry
were published in 1999,2 2013,3 and 2015.1 This
report constitutes an update on the epidemiology of
chronic kidney disease in Hong Kong based on data
from the Renal Registry up to 31 December 2022.
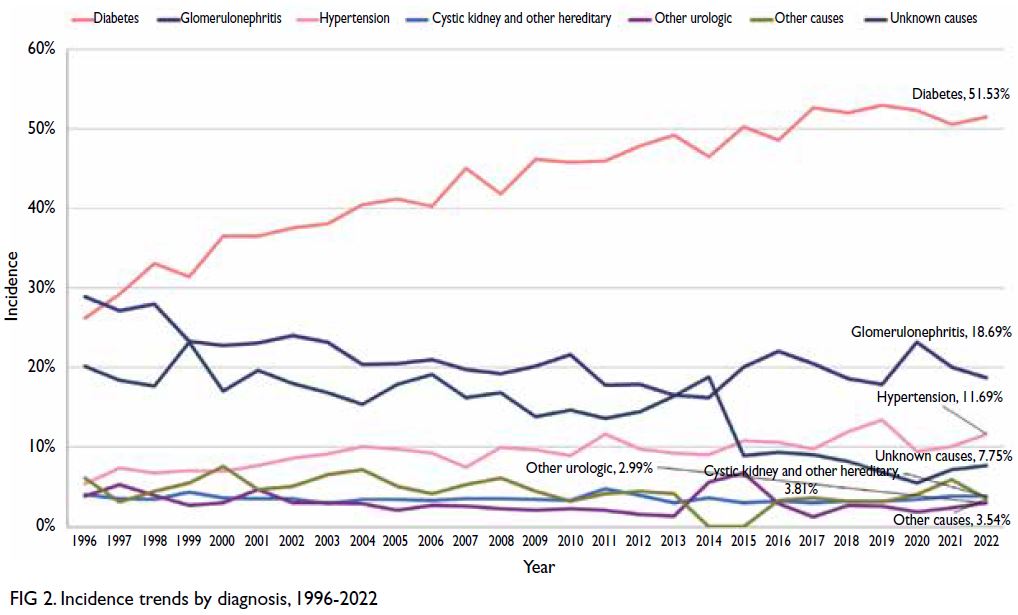
Incidence of kidney failure with replacement therapy
During 2022, 1471 new patients entered the KFRT
programme at an incidence of 197.5 per million
population (pmp), an 0.34% increase compared with
2021. Since the establishment of the Renal Registry
in 1995, the number of new patients increased by
139%, from 615 per year (95.1 pmp) in 1996 to a
peak of 1471 per year (197.5 pmp) in 2022 (Fig 1). As HA has had peritoneal dialysis (PD)–first policy,4
82.3% (n=1211) of new patients received PD, 17.0%
(n=250) received haemodialysis (HD), and 0.7%
(n=10) underwent kidney transplantation in 2022.
The male-to-female ratio among new patients was
1.8:1. For new patients in the HD and PD groups, the
greatest increase was observed among those aged 45
to 64 years, followed by those aged 65 to 74 years.
The median age of new KFRT patients in 2022 was
63.4 years, a substantial increase compared with the
median age of 51.4 years in 2013.1 Among new PD patients in 2022, 15.4% were aged >70 years.
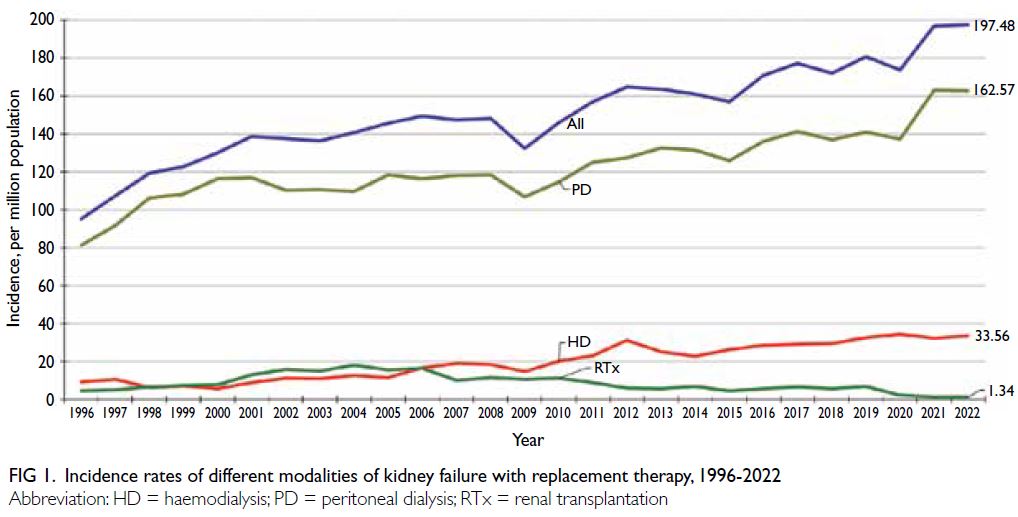
Fig 1. Incidence rates of different modalities of kidney failure with replacement therapy, 1996-2022
Since 1997, diabetes mellitus (DM) has been the
most common aetiology leading to kidney failure in
Hong Kong (Fig 2). In 2022, the percentage of KFRT
cases attributable to DM was 51.5% and among
the highest percentages worldwide,5 followed by
glomerulonephritis (18.7%) and hypertension (11.7%).
Over the 26 years from 1996 to 2022, the percentage of
KFRT cases attributable to DM increased from 26.2%
in 1996 to >50% beginning in 2017. The percentage
of KFRT cases attributable to glomerulonephritis
steadily decreased from 28.9% in 1996 to 18.7%
in 2022. The percentage of other causes remained
relatively stable between 2012 and 2022 (Fig 2).
Point prevalence of kidney failure
with replacement therapy
As of 31 December 2022, there were 11 115 patients
registered in the Renal Registry, representing a
prevalence of 1492 pmp. Among these patients,
5148 (46.3%) were receiving PD, 2452 (22.1%) were
receiving HD, and 3515 (31.6%) had a functioning
graft kidney. From 1996 to 2022, the number of KFRT patients in Hong Kong increased by 236%,
despite 49 fewer patients in 2022 causing a decrease
in the prevalence by 0.4%. This was likely due to
the substantial decrease (4.3%) in the prevalence
of patients with a functioning graft kidney, from
493.4 pmp in 2021 to 471.1 pmp in 2022 (online supplementary Fig 1). Between 1996 and 2022, the median patient age increased from 49.1 years to 61.0 years; in 2022, 12.4% of patients were aged >75
years and the male-to-female ratio among all KFRT
patients was 1.38:1.
Modes of renal replacement therapy
Peritoneal dialysis
Hong Kong has had a PD-first policy since 1985.4 All
new patients requiring dialysis therapy receive PD
unless they have medical contraindications to such
treatment. As of 31 December 2022, there were 5148
patients receiving PD in Hong Kong, representing a
prevalence of 691 pmp. These patients constituted
48.2% of all patients receiving renal replacement
therapy and 73.2% of all patients receiving dialysis
therapy. The number of patients receiving PD
was 1.2% higher in 2022 than in 2021. Since
establishment of the Renal Registry, the number of
patients receiving PD has increased by 176%, from
1865 in 1995 to 5148 in December 2022. Beginning
in 2020, the number of patients receiving automated
PD therapy also substantially increased. In 2022,
1330 patients received automated PD, constituting
25.8% of all PD patients. The overall peritonitis rate
among patients receiving continuous ambulatory
PD has greatly improved, from 0.55 episode per
patient-year in 1999 to 0.27 episode per patient-year
in 2022. Moreover, patients receiving automated PD
had a peritonitis rate of 0.23 episode per patient-year,
which was better than the rate among patients
receiving continuous ambulatory PD.
Haemodialysis
As of 31 December 2022, there were 2452 patients
receiving HD in the Renal Registry, representing a
prevalence of 329 pmp; this rate constituted a 2.0%
increase compared with 2021. Although PD remains
the main treatment for KFRT patients in Hong
Kong, there has been an increase in the provision of
HD services by the HA for patients with PD failure
or not suitable to receive PD. As of 31 December
2022, 1866 patients received HD services provided
by HA, including 1294 who were receiving in-centre
HD in HA facilities; this represented a 249% increase
compared with 371 patients in 1996. The proportion
of HD among all KFRT treatment modalities also
increased from 11% in 1996 to 17.6% in 2022,
resulting in the HD-to-PD ratio of 0.37:1. Since
the introduction of the nocturnal home dialysis
programme in 2006 and New Generation Home
HD in 2020, HA home HD services have expanded.
In 2022, 220 patients participated in home HD
programmes, representing 12% of all HD services
provided by the HA.
Kidney transplantation
In 2022, the number of patients with a functioning graft kidney continued to decline for the fourth
consecutive year since 2019. As of 31 December 2022,
there were 3515 patients with a functioning graft
kidney (3058 deceased donor transplants and 457
living donor transplants), representing a prevalence
of 472 pmp; this rate constituted a 4.3% decrease
compared with 2021. Among the 3515 transplant
recipients, 1198 patients underwent transplantation
in Hong Kong; these patients comprised 34.1% of the
overall kidney transplant population. The number of
patients with a functioning graft kidney increased
during 1995 (956 patients) and 2019 (3779 patients);
since then, the number has continuously decreased.
The overall increase during the analysis period was
due to the 364% increase in the number of deceased
donor transplant recipients (from 659 in 1996 to
3058 in 2022), whereas the increase in the number
of living donor transplant recipients was relatively
modest (ranging from 297 in 1996 to 457 in 2022).
In 2022, there were 45 deceased donor
(6.2 pmp) and 11 living donor (1.5 pmp) kidney
transplant surgeries performed in Hong Kong,
among the lowest rates worldwide.5 In terms of
transplant outcomes, the death-censored graft
survival rates for living donor kidney transplant
surgeries performed in Hong Kong during 2010 and
2019 were 0.97 at 1 year and 0.94 at 5 years, while
that for deceased donor kidney transplant surgeries
were 0.97 at 1 year and 0.89 at 5 years.
Mortality
The crude mortality rate among KFRT patients in Hong Kong remained stable at approximately 100
deaths per 1000 patient-years from 2012 to 2021
(online supplementary Fig 2). In 2022, possibly due to
the coronavirus disease 2019 pandemic, there was an
increase in the crude annual mortality rate to 147.9
deaths per 1000 patient-years. The annual mortality
rate increased with increasing age for all KFRT
treatment modalities. The highest rate was observed
among patients aged ≥75 years: >300 deaths per 1000
patient-years for both PD and HD patients. Overall,
transplant recipients had better survival than PD or
HD patients. Even among patients aged ≥75 years,
those receiving PD had a relative mortality risk 2.7-fold higher than the risk for transplant recipients.
Infection remained the most common cause
of death among KFRT patients (46.0% in 2022),
followed by cardiovascular disease (26.2%) and
cerebrovascular disease (4.1%) [online supplementary Fig 3]. Malignancy caused 12.4% of all deaths in
transplant recipients. Because of improved hepatitis
treatment for transplant recipients, liver failure has
caused <1% of deaths in recent years.
Discussion
The incidence and prevalence of KFRT have substantially increased since the establishment of the Renal Registry. Considering these trends,
the kidney disease epidemic constitutes a serious
burden on the healthcare system in Hong Kong.
Diabetes mellitus continues to be a leading cause
of KFRT in Hong Kong; this rate is among the top
quartile worldwide.5 There may be multiple reasons,
including the increasing prevalence of young-onset
DM6 7 and improved survival of DM patients with
cardiovascular disease.7 In 2020, the Asian Pacific
Society of Nephrology published a clinical practice
guideline that focused on the management of
diabetic kidney disease (DKD) in the Asia-Pacific
region.8 The Kidney Disease: Improving Global
Outcomes group also updated its Guideline for
Diabetes Management in Chronic Kidney Disease in
2022.9 Based on the collaborative efforts to provide
better care for patients with DKD, we hope to see
fewer new cases of KFRT attributable to DKD and a
decrease in the growth of KFRT incidence in Hong
Kong in the coming years.
By the end of 2022, >70% of prevalent
KFRT patients received PD. When considered in
combination with home HD, around 75% of the
dialysis population in Hong Kong is receiving
home-based dialysis therapy; this is the highest rate
worldwide.5 The benefits of this therapy were evident
during the coronavirus disease 2019 era.10 However,
home HD patients constituted approximately 3%
of all dialysis patients. It may be time to explore
the feasibility of modifying the PD-first policy to a
home-dialysis–first policy with further expansion
of home HD services for suitable patients, allowing
patients to maintain greater autonomy and freedom
when selecting their dialysis modality; this approach
could also serve as a transitional treatment method
for patients with PD failure before they begin in-centre
HD therapy.
Kidney transplant recipients continue to
display the lowest annual mortality rates. However,
the number of transplant surgeries in Hong Kong
remains low. In 2022, the transplant rate (including
both living and deceased donor surgeries) was 7.2 pmp, which ranked in the lowest quartile worldwide.5
Furthermore, only around 34% of patients with
a functioning graft kidney underwent surgery in
Hong Kong; many of the remaining patients chose
to undergo surgery elsewhere. Currently, there
are >2000 patients on the waiting list for a kidney
transplant in Hong Kong. It appears that there
are further opportunities for improvement in
transplantation services, particularly concerning the
promotion of living organ donation activities, the
willingness of relatives of potential brain-dead donors
to permit organ donation, and further expansion of
the donor pool. Considering the implementation of
the paired kidney donation programme and ABO-incompatible
transplantation programme, we look
forward to seeing increases in organ transplantation activities within Hong Kong that will benefit KFRT
patients in the future.
Author contributions
Concept or design: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: JYH Chan.
Critical revision of the manuscript for important intellectual content: KM Chow, CC Szeto, SCW Tang, SL Lui.
Acquisition of data: All authors.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: JYH Chan.
Critical revision of the manuscript for important intellectual content: KM Chow, CC Szeto, SCW Tang, SL Lui.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
The authors thank all medical and nursing staff members
of Alice Ho Miu Ling Nethersole Hospital, Caritas Medical
Centre, Hong Kong Children’s Hospital, Kwong Wah Hospital,
North District Hospital, Pamela Youde Nethersole Eastern
Hospital, Pok Oi Hospital, Prince of Wales Hospital, Princess
Margaret Hospital, Queen Elizabeth Hospital, Queen Mary
Hospital, Tin Shui Wai Hospital, Tseung Kwan O Hospital,
Tuen Mun Hospital, Tung Wah Hospital, United Christian
Hospital, and Yan Chai Hospital for contributions to the entry
of renal registry data. The authors also appreciate the support
of all transplant coordinators and staff members of the
Division of Transplantation and Immunogenetics of Queen
Mary Hospital, and thank members of the Renal Registry
Steering Group of the Central Renal Committee, Hospital
Authority and members of the Renal Registry Implementation
Team for their support and implementation of the Hong Kong
Renal Registry.
Funding/support
This commentary received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Supplementary material
The supplementary material was provided by the authors and
some information may not have been peer reviewed. Accepted
supplementary material will be published as submitted by the
authors, without any editing or formatting. Any opinions
or recommendations discussed are solely those of the
author(s) and are not endorsed by the Hong Kong Academy
of Medicine and the Hong Kong Medical Association.
The Hong Kong Academy of Medicine and the Hong Kong
Medical Association disclaim all liability and responsibility
arising from any reliance placed on the content.
References
1. Leung CB, Cheung WL, Li PK. Renal registry of Hong Kong—the first 20 years. Kidney Int Suppl (2011) 2015;5:33-8. Crossref
2. Lui SF, Ho YW, Chau KF, Leung CB, Choy BY. Hong Kong Renal Registry 1995-1999. Hong Kong J Nephrol 1999;1:53-60. Crossref
3. Ho YW, Chau KF, Choy BY, et al. Hong Kong Renal Registry
Report 2012. Hong Kong J Nephrol 2013;15:28-43. Crossref
4. Li PK, Lu W, Mak SK, et al. Peritoneal dialysis first policy
in Hong Kong for 35 years: global impact. Nephrology
(Carlton) 2022;27:787-94. Crossref
5. United States Renal Data System. 2023 USRDS Annual
Data Report: Epidemiology of kidney disease in the United
States. Bethesda (MD): National Institutes of Health,
National Institute of Diabetes and Digestive and Kidney
Diseases; 2023.
6. Luk AO, Ke C, Lau ES, et al. Secular trends in incidence of
type 1 and type 2 diabetes in Hong Kong: a retrospective
cohort study. PLoS Med 2020;17:e1003052. Crossref
7. Wu H, Lau ES, Yang A, et al. Trends in kidney failure
and kidney replacement therapy in people with diabetes
in Hong Kong, 2002-2015: a retrospective cohort study.
Lancet Reg Health West Pac 2021;11:100165. Crossref
8. Liew A, Bavanandan S, Prasad N, et al. Asian Pacific Society
of Nephrology Clinical Practice Guideline on Diabetic
Kidney Disease—an executive summary. Nephrology
(Carlton) 2020;25:809-17. Crossref
9. Kidney Disease: Improving Global Outcomes (KDIGO)
Diabetes Work Group. KDIGO 2022 Clinical Practice
Guideline for Diabetes Management in Chronic Kidney
Disease. Kidney Int 2022;102(5S):S1-127. Crossref
10. Wilkie M. Home dialysis—an international perspective.
NDT Plus 2011;4(Suppl 3):iii4-6. Crossref