Hong Kong Med J 2024 Aug;30(4):325–7 | Epub 6 Jun 2024
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Atypical metatarsal fracture in a Chinese postmenopausal woman with osteoporosis on long-term denosumab: a case report
Eunice KH Leung, MB, BS1 #; Andy KC Kan, MB, BS1 #; Jerome Lau, MB, BS2; CH Wong, MB, BS1; Connie HN Loong, MNurs1; Stephen CW Cheung, FRCR3; YC Woo, MD1; David TW Lui, MB, BS1
1 Department of Medicine, Queen Mary Hospital, The University of Hong Kong, Hong Kong SAR, China
2 Department of Surgery, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, China
3 Department of Radiology, Queen Mary Hospital, Hong Kong SAR, China
# Equal contribution
Corresponding author: Dr David TW Lui (dtwlui@hku.hk)
Case presentation
We report the first case of atypical fifth metatarsal
fracture in a 69-year-old Chinese woman
following long-term treatment for osteoporosis
with denosumab. She had been diagnosed with
hypertension in 2007 and was managed with
amlodipine and losartan. One year previously in
2006, she had been diagnosed with postmenopausal
osteoporosis based on low bone mineral density
(BMD) revealed at a health screening. Her height
and weight were 150 cm and 54 kg, respectively,
with a body mass index of 24.0 kg/m2. She had no
previous history of fracture or parental history of hip
fracture.
The patient was initially prescribed raloxifene
for 2 years but due to a suboptimal BMD response,
she was treated with alendronate for 4 years. Given
the prolonged use of alendronate, she was switched to strontium ranelate but this was discontinued a few
months later due to intolerance. Dual-energy X-ray
absorptiometry at that juncture in 2014 showed the
BMD of the L1-L4 level, the left femoral neck, and
the left total hip were 0.928 g/cm2 (T-score=-2.1), 0.646 g/cm2 (T-score=-2.9), and 0.725 g/cm2
(T-score=-2.4), respectively. She was started on
subcutaneous denosumab 60 mg every 6 months
that was continued until October 2021. Her most
recent dual-energy X-ray absorptiometry in
December 2020 revealed the BMD of the left femoral
neck and left total hip were 0.544 g/cm2 (T-score=-2.3) and 0.715 g/cm2 (T-score=-1.4), respectively,
indicating significant improvement. The BMD of
the lumbar spine was not reported due to significant
degenerative changes.
The patient presented to the primary care
physician in November 2021 with a 2-week history
of mechanical right lateral foot pain. She reported
no preceding injury but physical examination
revealed mild tenderness over the base of the right
fifth metatarsal. There was no joint effusion or signs
of infection and distal neurovascular status was
intact. X-ray of the right foot was performed (Fig a) and she was prescribed analgesics for right foot
tendinitis. One month later in December 2021, she
complained of persistent right foot pain during her
scheduled follow-up at the Osteoporosis Centre of
The University of Hong Kong. Physical examination
revealed intense tenderness over the lateral side of
her right foot, near the base of the fifth metatarsal.
Review of the X-ray taken in November 2021
identified beaking over the lateral aspect at the base
of the right fifth metatarsal, indicating a periosteal
reaction, associated with a transverse radiolucency
across the cortex. Repeat X-ray of the right foot
(Fig b) revealed a more prominent transverse
radiolucency across the same site. A diagnosis of
denosumab-related atypical metatarsal fracture was
reached given the long duration of antiresorptive
treatment (likely related to denosumab since fracture occurred after 7 years of denosumab),
prodromal symptoms and absence of high-energy
trauma, along with characteristic radiological
findings. Blood tests showed serum calcium level of
2.44 mmol/L (reference range, 2.24-2.63), phosphate
level of 0.98 mmol/L (reference range, 0.88-1.45),
creatinine level of 60 μmol/L (reference range,
49-82), parathyroid hormone level of 1.7 pmol/L
(reference range, 1.3-6.8), and 25-hydroxyvitamin
level of 70 nmol/L (sufficient level: 50-220). Although
bone turnover markers were not measured, serum
alkaline phosphatase level was on the low side at
48 U/L (reference range, 47-124) that could suggest
suppressed bone turnover. An X-ray of the left foot
was not available, but the patient had no history
of left foot pain. For her atypical right metatarsal
fracture, she was given a short leg plaster and
completed a course of physiotherapy. The fracture
healed completely in 6 months. She was started on
teriparatide as anti-osteoporosis treatment, and this
was tolerated well.
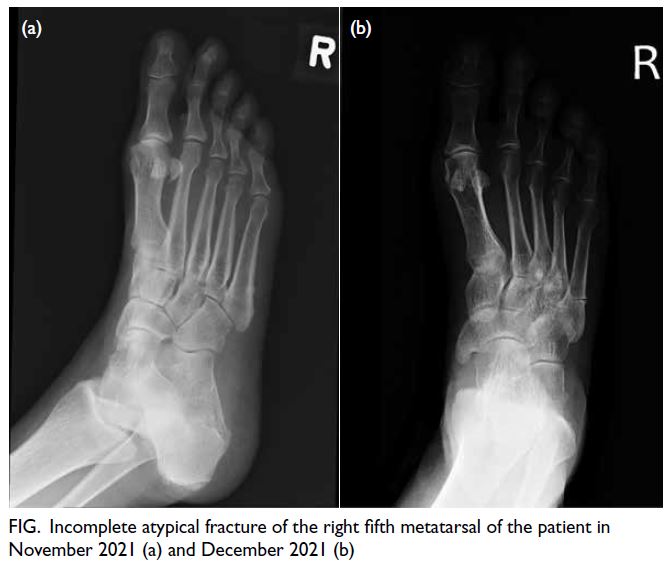
Figure. Incomplete atypical fracture of the right fifth metatarsal of the patient in November 2021 (a) and December 2021 (b)
Discussion
The American Society for Bone and Mineral Research Task Force published a report in 2014 on the case
definition of atypical femoral fracture (AFF),1 which
refers to fracture located along the femoral diaphysis
just distal to lesser trochanter to just proximal to
the supracondylar flare. Major and minor diagnostic
criteria were proposed. The pathophysiology is
postulated to be related to oversuppression of
bone turnover impairing normal bone remodelling
in response to physiological stress. Prolonged
bisphosphonate use has been associated with rare
adverse events of atypical fractures (3.2-50 cases per
100 000 person-years).1 Atypical femoral fractures
related to denosumab use have been reported, but
they are even rarer (0.8 per 10000 person-years).2
Our patient had been taking alendronate for 4 years
and denosumab for 7 years. It was very likely that
bone turnover had been severely suppressed. In line
with this, her serum alkaline phosphatase level was
at the lower end of the reference range.
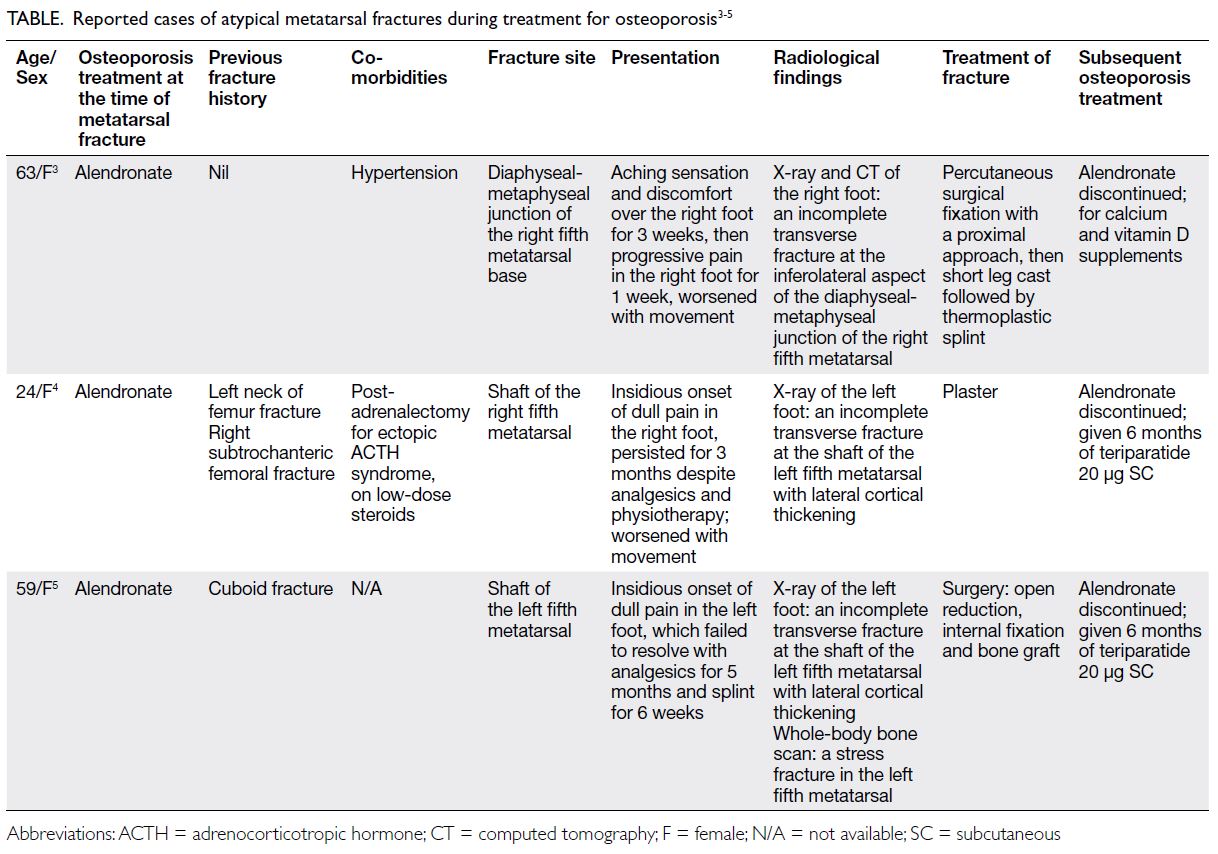
Less commonly, atypical fractures involving
long bones other than the femur have also been
reported among patients prescribed bisphosphonate
or denosumab, including the tibia and ulnar.3 Notably, atypical metatarsal fractures associated
with bisphosphonate use for osteoporosis have been reported in only three cases.3 4 5 Our case is
the first of atypical metatarsal fracture associated
with denosumab. Atypical metatarsal fractures
associated with antiresorptive agents, as illustrated
in our patient and other case reports (Table), share
several characteristics and are distinct from typical
fifth metatarsal fractures. They were all associated
with prodromal pain with no history of high-energy
impact. More importantly, the radiological features
fulfil some of the criteria of AFF proposed in the
American Society for Bone and Mineral Research
2013 consensus,1 including a fracture line originating
in the lateral cortex and periosteal reaction.
Although the atypical metatarsal fracture in our
patient was temporally related to the long duration
of denosumab, the possibility that alendronate had
caused abnormal microarchitecture that persisted
and was perpetuated by denosumab therapy could
not be excluded since she had also been prescribed
alendronate for 4 years.
When AFF is diagnosed, antiresorptive
agents should be stopped. The risk of AFF of the
contralateral femur declines after discontinuation
of bisphosphonate. Adequate vitamin D, calcium
supplementation and teriparatide can promote
healing and reunion of atypical femoral fracture.
Surgery promotes healing and relieves pain for AFF.
Incomplete AFF has been successfully treated with
prophylactic intramedullary nailing. Unlike AFF, the
treatment for atypical metatarsal fractures is less
well defined. The decision about treatment involves a
patient-physician discussion, although the presence
of a longer transverse radiolucent line across the
shaft favours surgical management.
Although bisphosphonate and denosumab
are safe and efficacious, rare side-effects of atypical
fractures have been reported. Our case highlights
the importance of clinician vigilance for atypical
fractures when patients on long-term antiresorptive
agents complain of pain over the long bones (not
limited to the femur) to enable timely management
to reduce morbidities and re-evaluate the anti-osteoporosis
strategy.
Author contributions
Concept or design: All authors.
Acquisition of data: EKH Leung, AKC Kan, YC Woo, DTW Lui.
Analysis or interpretation of data: EKH Leung, AKC Kan, SCW Cheung, YC Woo, DTW Lui.
Drafting of the manuscript: EKH Leung, AKC Kan, YC Woo, DTW Lui.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: EKH Leung, AKC Kan, YC Woo, DTW Lui.
Analysis or interpretation of data: EKH Leung, AKC Kan, SCW Cheung, YC Woo, DTW Lui.
Drafting of the manuscript: EKH Leung, AKC Kan, YC Woo, DTW Lui.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patient was treated in accordance with the Declaration of Helsinki. Informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
1. Shane E, Burr D, Abrahamsen B, et al. Atypical
subtrochanteric and diaphyseal femoral fractures: second
report of a task force of the American Society for Bone and
Mineral Research. J Bone Miner Res 2014;29:1-23. Crossref
2. Paparodis R, Buehring B, Pelley EM, Binkley N. A case of
an unusual subtrochanteric fracture in a patient receiving
denosumab. Endocr Pract 2013;19:e64-8. Crossref
3. Min BC, Chung CY, Park MS, Sung KH, Lee KM. A suspicious atypical fracture of 5th metatarsal bone: a case report. J Orthop Sci 2022;27:281-3. Crossref
4. Pradhan P, Saxena V, Yadav A, Mehrotra V. Atypical metatarsal fracture in a patient on long term bisphosphonate therapy. Indian J Orthop 2012;46:589-92. Crossref
5. Valiollahi B, Salehpour M, Bashari H, Majdi Sh, Mohammadpour M. Atypical metatarsal fracture in a patient on long-term bisphosphonate therapy (case report). J Res Orthopedic Sci 2019;6:25-30. Crossref