Hong Kong Med J 2024 Aug;30(4):300–9 | Epub 15 Aug 2024
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
End-of-life practices in Hong Kong intensive care
units: results from the Ethicus-2 study
Gavin Matthew Joynt, MBBCh, FHKAM (Anaesthesiology)1; Steven KH Ling, MB, ChB, FHKAM (Anaesthesiology)2; LL Chang, MB, ChB, FHKAM (Medicine)3; Polly NW Tsai, MB, BS, FHKAM (Medicine)4; Gary KF Au, MB, ChB, FHKAM (Medicine)5; Dominic HK So, MB, BS, FHKAM (Anaesthesiology)6; FL Chow, MB, BS, FHKAM (Medicine)7; Philip KN Lam, MB, BS, FHKAM (Medicine)8; Alexander Avidan, MD9; Charles L Sprung, MD9; Anna Lee, MPH, PhD1; Hong Kong Ethicus-2 study Group
for the Hong Kong Ethicus-2 study group (group members are listed at the end of the article)
1 Department of Anaesthesia and Intensive Care, The Chinese University of Hong Kong, Prince of Wales Hospital, Hong Kong SAR, China
2 Department of Intensive Care, Tuen Mun Hospital, Hong Kong SAR, China
3 Department of Intensive Care, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, China
4 Adult Intensive Care Unit, Queen Mary Hospital, Hong Kong SAR, China
5 Department of Intensive Care, Kwong Wah Hospital, Hong Kong SAR, China
6 Department of Intensive Care Unit, Princess Margaret Hospital/Yan Chai Hospital, Hong Kong SAR, China
7 Department of Intensive Care, Caritas Medical Centre, Hong Kong SAR, China
8 Department of Intensive Care, North District Hospital, Hong Kong SAR, China
9 Department of Anesthesiology, Critical Care and Pain Medicine, Hadassah Medical Organization and Faculty of Medicine, Hebrew University of Jerusalem, Jerusalem, Israel
Corresponding author: Prof Gavin Matthew Joynt (gavinmjoynt@cuhk.edu.hk)
Abstract
Introduction: The need for end-of-life care is
common in intensive care units (ICUs). Although
guidelines exist, little is known about actual end-of-life care practices in Hong Kong ICUs. The study
aim was to provide a detailed description of these
practices.
Methods: This prospective, multicentre
observational sub-analysis of the Ethicus-2 study
explored end-of-life practices in eight participating
Hong Kong ICUs. Consecutive adult ICU patients
admitted during a 6-month period with life-sustaining
treatment (LST) limitation or death were
included. Follow-up continued until death or 2
months from the initial decision to limit LST.
Results: Of 4922 screened patients, 548 (11.1%) had
LST limitation (withholding or withdrawal) or died
(failed cardiopulmonary resuscitation/brain death).
Life-sustaining treatment limitation occurred in
455 (83.0%) patients: 353 (77.6%) had decisions
to withhold LST and 102 (22.4%) had decisions to
withdraw LST. Of those who died without LST
limitation, 80 (86.0%) had failed cardiopulmonary
resuscitation and 13 (14.0%) were declared brain
dead. Discussions of LST limitation were initiated
by ICU physicians in most (86.2%) cases. Shared
decision-making between ICU physicians and
families was the predominant model; only 6.0%
of patients retained decision-making capacity.
Primary medical reasons for LST limitation were
unresponsiveness to maximal therapy (49.2%) and
multiorgan failure (17.1%). The most important
consideration for decision-making was the patient’s
best interest (81.5%).
Conclusion: Life-sustaining treatment limitations
are common in Hong Kong ICUs; shared decision-making between physicians and families in the
patient’s best interest is the predominant model. Loss
of decision-making capacity is common at the end of
life. Patients should be encouraged to communicate
end-of-life treatment preferences to family members/surrogates, or through advance directives.
New knowledge added by this study
- Life-sustaining treatment (LST) limitation at the end of life is common in Hong Kong intensive care units (ICUs).
- Compared with international practices, the time from admission to LST limitation is relatively long in Hong Kong.
- Shared decision-making between healthcare providers and patients, family members, or patient surrogates is the predominant decision-making model.
- Most patients lack the mental capacity for decision-making at the end of life.
- Patient preferences regarding the use of life-sustaining therapies at the end of life are usually unknown, and the use of advance directives is rare.
- End-of-life care practices in Hong Kong ICUs generally align with local guidelines and the international consensus.
- Local factors possibly preventing earlier implementation of LST limitation in appropriate patients should be explored.
- The public should be educated to communicate their preferences regarding the use of life-sustaining therapies in ICUs to surrogates/family members, or through advance directives.
Introduction
Despite high-quality care, many patients admitted
to the intensive care unit (ICU) do not survive;
therefore, management of the dying process
is a required skill among modern healthcare
professionals.1 Life-sustaining technology has
advanced sufficiently that it is possible to maintain
vital organ function despite the knowledge that the
patient’s return to health and an acceptable quality
of life is no longer feasible. In these situations, a
decision to limit life-sustaining treatment (LST) has
become a common clinical practice in most countries
worldwide.2 3 4 5 6 In recent decades, attempts to define desirable principles for end-of-life care according
to a global professional consensus have achieved
considerable success.3 Nevertheless, decision-making
processes for death and dying are likely to
be heavily influenced by regional and cultural norms
and expectations; thus, it is reasonable to expect
different medical practices related to end-of-life
decisions. Several local and international surveys
of healthcare professionals have revealed regional
differences in attitudes towards end-of-life ethical
concerns, as well as substantial differences in clinical
practices.7 8 9 10 11 Limited prospective observational data from international studies support the existence of
regional variability in end-of-life practices.5 12 13
Hong Kong is a special administrative region of
China with an overwhelmingly Chinese population;
nevertheless, it maintains an independent fiscal
budget and healthcare system. The Hong Kong
Hospital Authority, funded by the Hong Kong SAR
Government, provides >90% of hospital-based
services available for the local population; although
nearly all healthcare workers in the public health
services exhibit Chinese ethnicity, health services
are based on Western medical conventions.14
Hong Kong is considered a high-income region,
and recently published patient outcomes data
indicate that the Hong Kong Hospital Authority
provides high-quality intensive care services.15 The
juxtaposition of a Western medical system and a
culturally Chinese population creates a situation
where Western medical practices (driven by Western
cultural and ethical values) may conflict with
Chinese cultural values, particularly at the end of
life when deep-rooted cultural beliefs may become
more relevant. A small number of studies have
explored end-of-life care practices in Hong Kong
ICUs; these include a survey of ICU physicians’
ethical attitudes concerning end-of-life care8 and a
prospective observational study regarding end-of-life
practices at a single tertiary university hospital.16
No observational territory-wide data have been
published thus far. Additionally, end-of-life practices
in Europe have substantially changed in recent
decades17; similar changes may have occurred in
Hong Kong, although previous comparative data
are sparse.16 Multiple Hong Kong ICUs participated
in the recent worldwide Ethicus-2 study,13 18 with
the understanding that the Hong Kong data would
be accessible for secondary analysis. The aim of
this study was to provide a detailed description of
current end-of-life care practices in Hong Kong.
Methods
This study constituted a secondary analysis of the
Ethicus-2 database, focusing on the Hong Kong data.
The Ethicus-2 study was a prospective, multicentre,
global observational study of end-of-life practices in
199 ICUs across 36 countries.13 17 All 15 adult ICUs in
publicly funded hospitals in Hong Kong were invited
to participate by the Hong Kong study coordinator,
representing the Hong Kong Society of Critical Care
Medicine. Eight ICUs in Hong Kong participated.
Consecutive adult patients admitted to the
ICU over an individual ICU-selected 6-month
period between 1 September 2015 and 30 September
2016 with LST limitation or death were included.
Follow-up continued until death or 2 months
from the initial decision to limit LST. End-of-life
categories included withholding LST, withdrawing
LST, active shortening of the dying process, failed cardiopulmonary resuscitation (CPR), and brain
death. These categories were mutually exclusive;
if more than one limitation was triggered in a
particular case, the most stringent limitation was
chosen (ie, active shortening of the dying process
was considered more stringent than LST withdrawal,
followed by LST withholding).
Data were collected by the senior physician, or
a representative, responsible for making end-of-life
decisions. De-identified patient data were entered
into a secure online database. Collected data included
age; sex; religion; end-of-life category; admission
date, time, and diagnoses; chronic disorders; use of
ventilation and vasopressors, sedatives, or analgesics;
date and time of hospital and ICU admission; and
date and time of death or discharge from the ICU or
hospital. End-of-life process data collected included
type, date, and time of LST; presence of information
about patient wishes; discussions with the patient
or their family; degree of concurrence between the
decision and patient/family wishes; and reasons for
treatment decisions.
Data quality was monitored by concurrent
audit and feedback, with a quality review involving
5% of all patients.17 Categorical variables were
reported as numbers and percentages within
end-of-life groups. After normality assessment
using the Shapiro–Wilk test, continuous variables
were reported as means (standard deviations)
or medians (interquartile ranges [IQRs]), as
appropriate. Differences among LST withholding,
LST withdrawal, and no LST limitation groups were
compared using analysis of variance, the Kruskal–Wallis H test, or the Chi squared test, as appropriate.
Subsequent pairwise group comparisons were
performed with Bonferroni correction for multiple
tests. All analyses were performed using SPSS
software (Windows version 27.0; IBM Corp, Armonk
[NY], United States).
This prospective observational study has been reported in accordance with the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) checklist for observational studies.
Results
The eight participating ICUs were distributed
across Hong Kong; at least two ICUs represented
each of the New Territories, Kowloon, and Hong
Kong Island. Two ICUs were located in academic
university hospitals (comprising 20 and 25 acute ICU
beds, respectively), and the remainder were located
in medium-to-large regional hospitals (ranging from
12 to 22 acute ICU beds per unit).
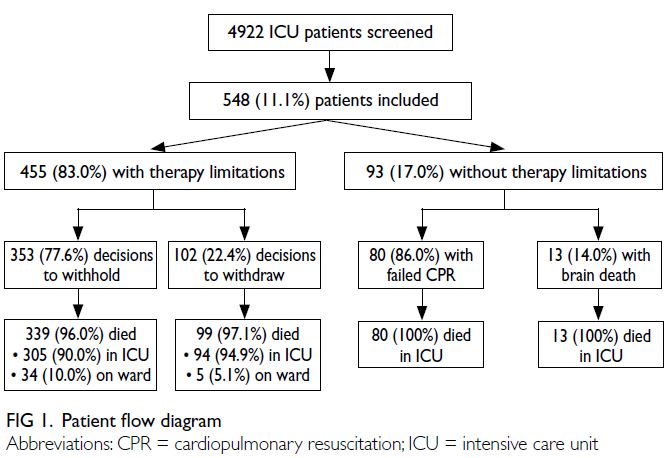
Among the 4922 consecutive patients screened
during the study period, 548 (11.1%) patients with
LST limitation (withholding or withdrawal) or death
(failed CPR or brain death) were included in the study. Life-sustaining treatment limitation occurred
in 455 (83.0%) patients, including 353 (77.6%) with
decisions to withhold LST and 102 (22.4%) with
decisions to withdraw LST. Of the 93 patients who
died without LST limitation, 80 (86.0%) had failed
CPR, and 13 (14.0%) experienced brain death (Fig 1). No patients underwent shortening of the dying process.
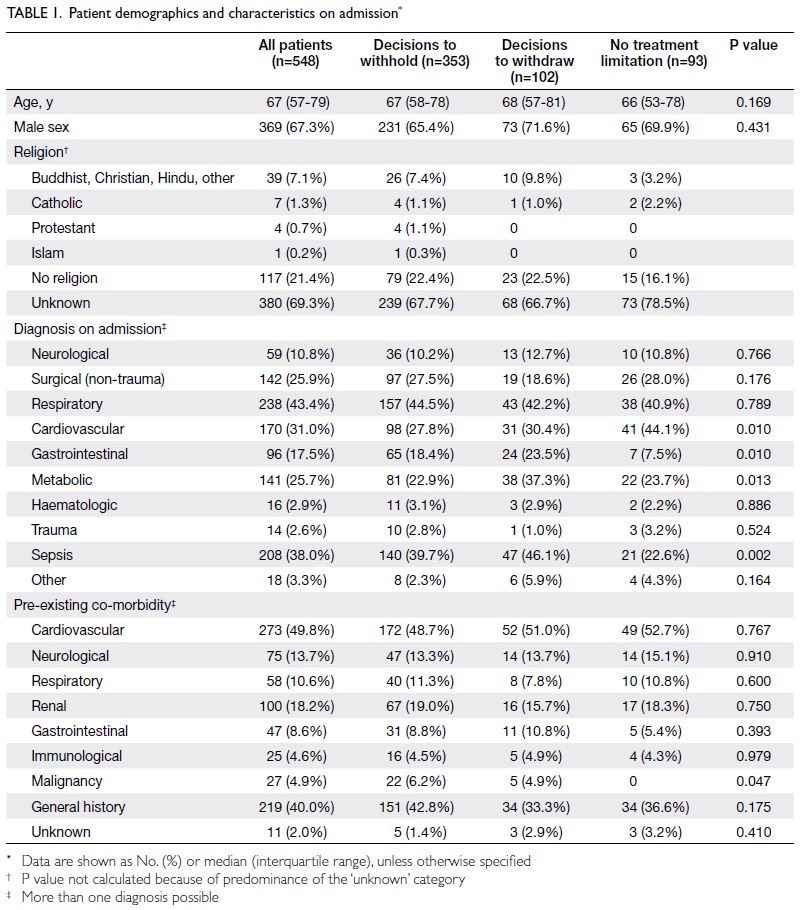
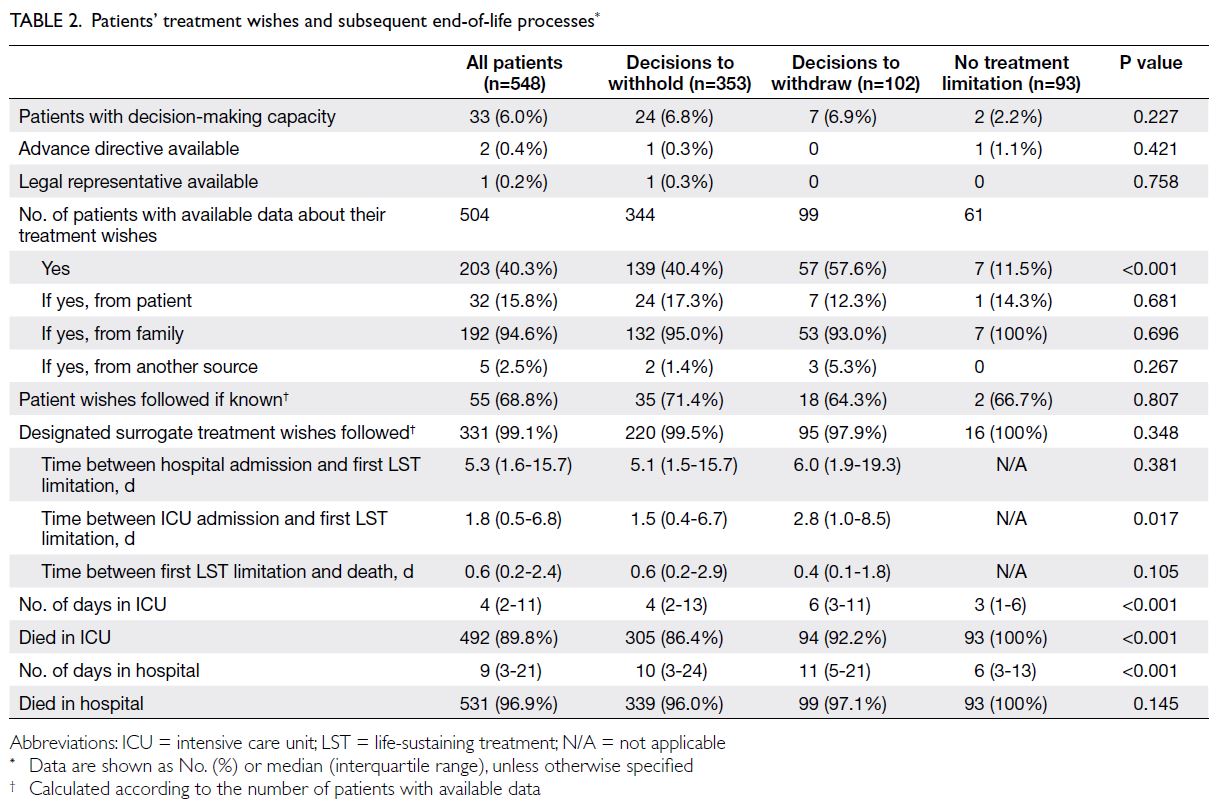
Patient characteristics are summarised in Table 1; knowledge of patient and family/surrogate wishes,
as well as the timing of end-of-life processes, are
described in Table 2. Patients without LST limitation
had a shorter duration of ICU stay (median: 3 days,
IQR=1-6) compared with patients who had decisions
to withhold (median: 4 days, IQR=2-13) or withdraw
(median: 6 days, IQR=3-11) [P<0.001].
The prevalences of treatments withheld or
withdrawn at the initial and final decisions to limit
LST are shown in Figure 2. Higher percentages of
patients had endotracheal tube (P=0.009), renal
replacement therapy (P<0.001), and sedation/analgesia (P=0.002) withheld at the final decision,
compared with the initial decision. Similarly, higher
percentages of patients had endotracheal tube,
mechanical ventilation, vasopressor, and renal
replacement therapy withdrawn at the final decision
(all P<0.001), compared with the initial decision.
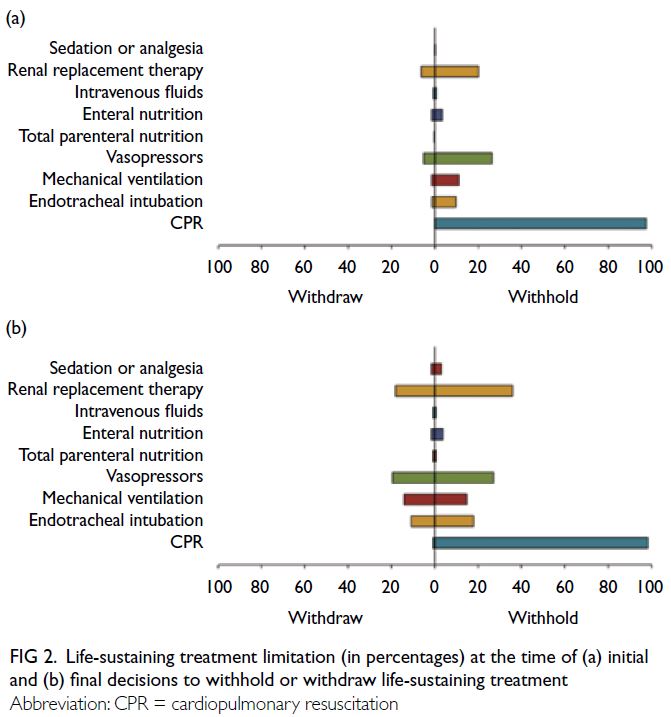
Figure 2. Life-sustaining treatment limitation (in percentages) at the time of (a) initial and (b) final decisions to withhold or withdraw life-sustaining treatment
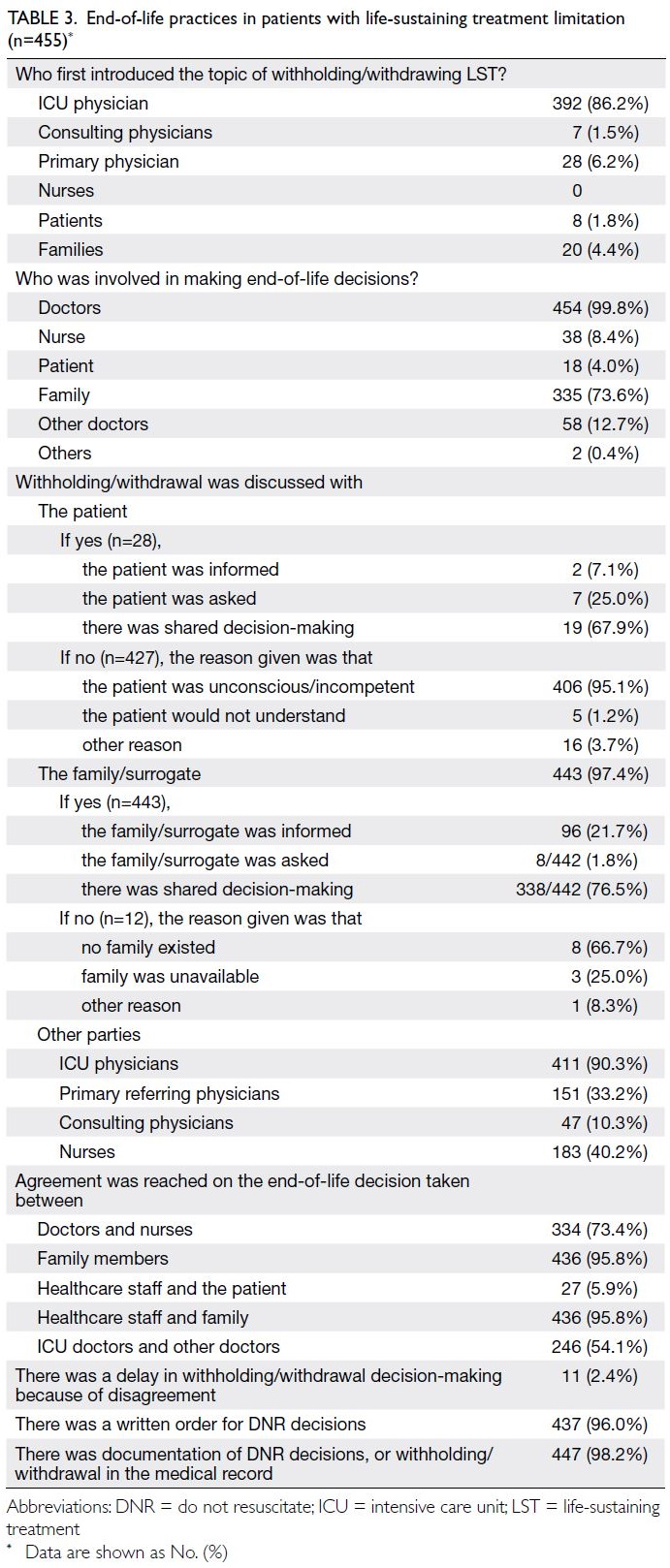
Information about decision-making practices
for patients with LST limitation is provided in Table 3. In the majority of cases, the ICU physician was
involved in key aspects of end-of-life decision-making
and implementation. The responsible
ICU physicians’ explanations of the reasons and
considerations for supporting end-of-life decisions
are provided in Table 4. The primary clinical reason
for limiting LST was unresponsiveness to maximal
therapy; the patient’s best interest, perceived good medical practice, and autonomy were key decision-making considerations.
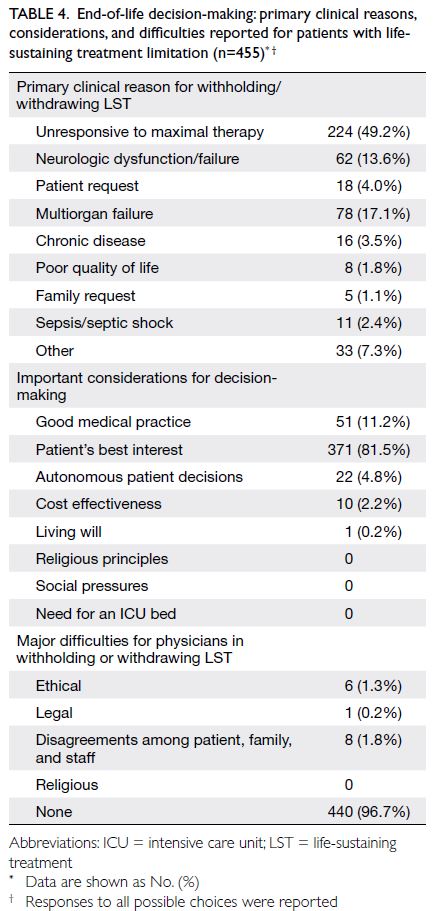
Table 4. End-of-life decision-making: primary clinical reasons, considerations, and difficulties reported for patients with lifesustaining treatment limitation (n=455)
Discussion
This is the first large, multicentre, prospective,
observational study of end-of-life care practices in
Hong Kong ICUs. Our main findings were that LST
limitation preceded >80% of patient deaths, and
that death occurred in the vast majority of patients
with LST limitation; only 4% of patients with LST
limitation were alive at 2 months. Only 15% of
ICU patients died after failed CPR (ie, without any LST limitations). Advance directives were rarely
available, and no cases of active shortening of the
dying process (euthanasia) were reported. Life-sustaining
treatment limitation occurred in the
majority (83.0%) of patients, predominantly via
withholding (77.6%); withdrawal was less common
(22.4%) [Fig 1]. High rates of LST limitation, such as
those observed in this study, are generally presumed
to reflect good end-of-life practices and have been
associated with the presence of written end-of-life
guidelines,19 such as those provided by the Hong Kong Hospital Authority.20
Withholding and withdrawing life-sustaining
treatment
Regarding treatments that were withdrawn or
withheld, the withholding of CPR universally
accompanied all limitation decisions. Nutrition,
hydration, and sedation were rarely withheld or
withdrawn at any time, consistent with guidance from
professional bodies in Hong Kong that additional
safeguards are necessary when considering these
actions.20 At the time of the initial limitation
decision, there was relatively frequent withholding
of vasopressors and renal replacement therapy;
withholding or withdrawal of endotracheal tubes
was less common. Although the patterns of LST
limitation were similar between the initial and final
decisions, such that withholding remained more
prevalent than withdrawal, a substantial increase
was observed in the prevalence of LST withdrawal
at the time of the final decision. This finding may
reflect the common Chinese cultural perspective
that LST withholding and withdrawal are not
ethically equivalent, with a documented preference
for withholding over withdrawal as an end-of-life
care strategy.8 11 The increase in withdrawal
prevalence at the time of the final decision across key
treatment categories (eg, vasopressors, mechanical ventilation, and renal replacement therapy) suggests
that, with increasing prognostic certainty and clear
progression towards death, LST withdrawal becomes
more acceptable. There also appeared to be a greater
reluctance to adopt withdrawal strategies early in the
ICU stay, evidenced by the longer interval between
ICU admission and initial limitation, if the initial
limitation was withdrawal. This tendency may also
reflect the need for greater prognostic certainty
prior to the implementation of a withdrawal strategy.
Comparisons with international data indicate that
although the high rate of LST limitation prior to
death is similar to practices in other countries, the
early and more frequent use of withholding (rather
than withdrawal) remains distinct from practices reported in North America, North and Central Europe, and Asia.13
Comparative historical data from Hong
Kong are limited. A single-centre observational
study conducted between 1997 and 1999 showed
that LST limitation occurred in 59% of patients,16
although its LST limitation categories are not fully
aligned with those of the current study. Notably,
the mean interval between ICU admission and LST
limitation in this previous study was nearly 8 days,16
whereas the median interval in the current study
was 1.8 days (IQR=0.5-7); this difference suggests
that recognition of the need for LST limitation is
occurring much earlier in Hong Kong, consistent
with a pattern observed in Europe during the
same period.17 21 When LST limitation is indicated,
earlier intervention leads to a shorter duration of
patient discomfort; the observed reduction in time
to limitation may represent a meaningful practice
improvement over time.
Despite similar rates of LST withholding/withdrawal, the low rate of survival after LST
limitation in Hong Kong (3%-4%)—comparable to
the findings in a previous pan-European study12—contrasts with current European ICU outcomes,
where the combined survival rate after LST
withdrawal or withholding was 20%.17 This difference
may possibly be attributed to implementing LST
in patients at the very end-of-life when prognostic
certainty is greater. The earlier implementation of
end-of-life interventions may represent an area
for further exploration to improve end-of-life ICU
practices and minimise suffering.
Practice components of end-of-life care
Key practices in end-of-life decision-making
included the initiation of discussions to limit LST by
ICU physicians in the vast majority of cases; when
such discussions began, ICU physicians were always
involved in end-of-life decision-making processes.
Notably, shared decision-making between ICU
physicians and families was the predominant
model reported. These findings align with the best
practices described in recent international expert
consensus documents.1 3 Despite frequent use
of the shared decision-making model, direct or
indirect knowledge of the patient’s wishes regarding
LST was available for fewer than half of patients
(40.3%); in the vast majority of cases (94.6%), this
information was transmitted by relatives rather than
by the patient themselves. Only 33 (6.0%) patients
had decision-making capacity during the decision-making
process, and only two (0.4%) patients had
advance directives (Table 2). These results highlight
the need to encourage patients to discuss their
wishes regarding future end-of-life care preferences
with relatives, or communicate such wishes through
the use of advance directives, ensuring that patients receive the preferred level of care at this critical
time. Nevertheless, levels of agreement among all
parties regarding end-of-life decisions were high,
and delays in decision-making due to disagreement
were uncommon.
Advance directives
Advance directives in Hong Kong ICUs were rarely
available, possibly due to selection bias; individuals
with advanced disease and a greater likelihood of
advance directives may have lower ICU admission
priority. However, the current rate of advance
directive use in North American ICUs at the end of
life is nearly 50%.18 A relatively recent population-based
study demonstrated very low public awareness
of advance directives in Hong Kong, such that 86% of
participants reported no previous knowledge of the
advance directive concept.22 However, once informed
of this concept, the majority of participants indicated
a willingness to consider using such directives. The
legislative process to formalise advance directive
use in Hong Kong has substantially progressed,
and there is a recognised need for public education
and healthcare professional–specific guidance to
promote the use of these directives.23 24
Patient characteristics and reasons for limitations of life-sustaining treatment
In the present study, the most common diagnostic
categories at ICU admission were respiratory
(43.4%) and sepsis-related (38.0%) [Table 1],
similar to reported findings in most other regions
worldwide.18 There were no substantial age or sex
differences regarding LST limitation, but there were
distinct differences in ICU admission diagnoses,
such that limitation was less likely in patients
with cardiovascular conditions and more likely
in patients with sepsis or gastrointestinal disease.
The vast majority of patients exhibited at least one
co-morbidity, again similar to recently reported
findings in other regions.18 Intriguingly, no patients
with cancer were among those who died without
LST limitation.
The primary clinical reasons for initiating LST
limitation included unresponsiveness to maximal
therapy, multiorgan failure, and neurologic failure;
in few cases, the limitation arose from a family
request or mainly in relation to quality of life (Table 4). Overwhelmingly, the primary consideration for
decision-making was the patient’s best interest,
followed by the principle of good medical practice,
defined as the recognition that continued maximal
therapy would not be beneficial for the patient (Table 4). These observations closely match the responses
recently provided by a group of international experts
who were asked to rank the triggers they would likely
use in clinical practice to initiate discussions about
LST limitation.1
Decision-making at end-of-life
Two questions related to decision-making and
patient treatment wishes revealed an interesting
observation. Across all end-of-life categories,
approximately 70% of physicians in charge of end-of-life decision-making reported that if the patient’s
wishes were known, they were followed. In contrast,
when a surrogate’s treatment wishes were known,
they were followed in nearly every case (Table 2).
These responses indicate that the family’s treatment
preferences are respected more frequently compared
with known patient preferences, in contrast to
guidelines from the Medical Council of Hong Kong25 and the Hospital Authority.20 Both guidelines clearly
state that treatment preferences should be sought
via communication with patients and family when
possible, and a consensus should be reached; however,
when conflicting views cannot be reconciled, the
patient’s treatment preferences should supersede the
family’s preferences.20 25 It is possible that physicians
prioritised the family’s preferences because few
patients were capable of direct communication;
there was low certainty regarding perceived
patient wishes when communicated through third
parties. Nevertheless, this finding warrants further
investigation and reflection among Hong Kong ICU
healthcare professionals.
Most communication related to end-of-life
decision-making occurred between ICU physicians
and family/surrogates; nurses, primary physicians,
and consulting physicians were involved in
fewer than half of the reported cases. It has been
suggested that this relatively low percentage of nurse
involvement is an underestimate because most data
were reported by physicians who may be unaware of
nurse involvement.26 Decision agreement between
healthcare staff and family members, as well as
among family members, was reportedly very high
(>95%) [Table 3]. Disagreements between family
and staff were rare, as were delays in implementing
end-of-life care because of disagreement, indicating
a high level of acceptance of the decision-making
process by the public and healthcare professionals in
Hong Kong.
Strengths and limitations
This study’s strengths included its involvement of
a large number of patients over a 6-month period,
provision of detailed follow-up data for up to 2
months, prospective design, and representation of
most public ICUs in Hong Kong. Moreover, the data
were provided by the physician in charge of end-of-life decision-making, with support from clear
definitions and uniform collection across ICUs;
they were also subjected to external quality control
measures, minimising measurement bias. The main
limitations were the lack of random ICU allocation and inclusion of consenting ICUs only, which may have introduced selection bias.
Conclusion
Data from the majority of Hong Kong ICUs,
spanning the entire territory and representing both
academic and non-academic ICUs, revealed that LST
limitation occurs in most patients prior to death in
ICU. Practices generally align with recommendations
from local professional bodies and key international
consensus documents. Although decision-making
is usually initiated by ICU physicians, shared
decision-making between medical staff and family/surrogates is the predominant model. Because a loss
of decision-making capacity is common in the ICU,
patients should be encouraged to communicate their
wishes regarding end-of-life care through dialogue
with relatives or more formal methods. Certain
practices and outcomes observed in Hong Kong are
more similar to those reported in North America
and Europe than to patterns in other parts of Asia.
Author contributions
Concept or design: CL Sprung, A Avidan, GM Joynt.
Acquisition of data: GM Joynt, SKH Ling, LL Chang, PNW Tsai, GKF Au, DHK So, FL Chow, PKN Lam.
Analysis or interpretation of data: A Lee, GM Joynt.
Drafting of the manuscript: GM Joynt.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: GM Joynt, SKH Ling, LL Chang, PNW Tsai, GKF Au, DHK So, FL Chow, PKN Lam.
Analysis or interpretation of data: A Lee, GM Joynt.
Drafting of the manuscript: GM Joynt.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
No funding was obtained to conduct this research from any
funding agency in the public, commercial, or not-for-profit
sectors. The Walter F and Alice Gorham Foundation funded
the international co-ordination of the Ethicus-2 study. The
Foundation had no part in the design and conduct of the
research; collection, management, analysis, and interpretation
of the data; preparation, review, or approval of the manuscript;
and decision to submit the manuscript for publication.
Ethics approval
This research was approved by the relevant Research Ethics Committee for each of the participating centres, including:
(1) Tuen Mun Hospital—The New Territories West Cluster Research Ethics Committee of Hospital Authority, Hong Kong (Ref No.: NTWC/CREC/15078);
(2) Prince of Wales Hospital and North District Hospital—The Joint Chinese University of Hong Kong—New Territories East Cluster Clinical Research Ethics Committee, Hong Kong (Ref No.: 2015.080);
(3) Caritas Medical Centre—The Kowloon West Cluster Research Ethics Committee of the Hospital Authority, Hong Kong [Ref No.: KW/EX-15-103(88-02)];
(4) Kwong Wah Hospital—The Kowloon West Cluster Research Ethics Committee of the Hospital Authority, Hong Kong [Ref No.: KW/EX-15-105(88-04)];
(5) Pamela Youde Nethersole Eastern Hospital—The Hong Kong East Cluster Research Ethics Committee of the Hospital Authority, Hong Kong (Ref No.: HKEC-2015-028);
(6) Princess Margaret Hospital—The Kowloon West Cluster Research Ethics Committee of the Hospital Authority, Hong Kong [Ref No.: KW/EX-15-104(88-03)]; and
(7) Queen Mary Hospital—Institutional Review Board of The University of Hong Kong / Hospital Authority Hong Kong West Cluster, Hong Kong (Ref No.: UW 15-361).
(1) Tuen Mun Hospital—The New Territories West Cluster Research Ethics Committee of Hospital Authority, Hong Kong (Ref No.: NTWC/CREC/15078);
(2) Prince of Wales Hospital and North District Hospital—The Joint Chinese University of Hong Kong—New Territories East Cluster Clinical Research Ethics Committee, Hong Kong (Ref No.: 2015.080);
(3) Caritas Medical Centre—The Kowloon West Cluster Research Ethics Committee of the Hospital Authority, Hong Kong [Ref No.: KW/EX-15-103(88-02)];
(4) Kwong Wah Hospital—The Kowloon West Cluster Research Ethics Committee of the Hospital Authority, Hong Kong [Ref No.: KW/EX-15-105(88-04)];
(5) Pamela Youde Nethersole Eastern Hospital—The Hong Kong East Cluster Research Ethics Committee of the Hospital Authority, Hong Kong (Ref No.: HKEC-2015-028);
(6) Princess Margaret Hospital—The Kowloon West Cluster Research Ethics Committee of the Hospital Authority, Hong Kong [Ref No.: KW/EX-15-104(88-03)]; and
(7) Queen Mary Hospital—Institutional Review Board of The University of Hong Kong / Hospital Authority Hong Kong West Cluster, Hong Kong (Ref No.: UW 15-361).
The requirement for informed patient consent was waived
by the relevant Clinical Research Ethics Committees as the
study was observational only, where all collected data were
anonymised at source and only de-identified data were
passed on to the co-ordinating centre for analysis, and risk to
participants was minimal.
Members of the Hong Kong Ethicus-2 study
group (in alphabetical order):
Gary KF Au, Department of Intensive Care, Kwong Wah Hospital, Hong Kong SAR, China
Alexander Avidan, Department of Anesthesiology, Critical Care and Pain Medicine, Hadassah Medical Organization and Faculty of Medicine, Hebrew University of Jerusalem, Jerusalem, Israel
KC Chan, Department of Intensive Care, Tuen Mun Hospital, Hong Kong SAR, China
WM Chan, Adult Intensive Care Unit, Queen Mary Hospital, Hong Kong SAR, China
LL Chang, Department of Intensive Care, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, China
FL Chow, Department of Intensive Care, Caritas Medical Centre, Hong Kong SAR, China
Gavin Matthew Joynt, Department of Anaesthesia and Intensive Care, The Chinese University of Hong Kong, Prince of Wales Hospital, Hong Kong SAR, China
Gladys WM Kwan, Department of Intensive Care, Tuen Mun Hospital, Hong Kong SAR, China
Philip KN Lam, Department of Intensive Care, North District Hospital, Hong Kong SAR, China
Anna Lee, Department of Anaesthesia and Intensive Care, The Chinese University of Hong Kong, Prince of Wales Hospital, Hong Kong SAR, China
E Leung, Adult Intensive Care Unit, Queen Mary Hospital, Hong Kong SAR, China
Steven KH Ling, Department of Intensive Care, Tuen Mun Hospital, Hong Kong SAR, China
CH Ng, Department of Intensive Care, Kwong Wah Hospital, Hong Kong SAR, China
HP Shum, Department of Intensive Care, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, China
Dominic HK So, Department of Intensive Care Unit, Princess Margaret Hospital/Yan Chai Hospital, Hong Kong SAR, China
Charles L Sprung, Department of Anesthesiology, Critical Care and Pain Medicine, Hadassah Medical Organization and Faculty of Medicine, Hebrew University of Jerusalem, Jerusalem, Israel
L Sy, Department of Intensive Care, North District Hospital, Hong Kong SAR, China
Polly NW Tsai, Adult Intensive Care Unit, Queen Mary Hospital, Hong Kong SAR, China
HH Tsang, Department of Intensive Care, Kwong Wah Hospital, Hong Kong SAR, China
WT Wong, Department of Anaesthesia and Intensive Care, The Chinese University of Hong Kong, Prince of Wales Hospital, Hong Kong SAR, China
Alexander Avidan, Department of Anesthesiology, Critical Care and Pain Medicine, Hadassah Medical Organization and Faculty of Medicine, Hebrew University of Jerusalem, Jerusalem, Israel
KC Chan, Department of Intensive Care, Tuen Mun Hospital, Hong Kong SAR, China
WM Chan, Adult Intensive Care Unit, Queen Mary Hospital, Hong Kong SAR, China
LL Chang, Department of Intensive Care, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, China
FL Chow, Department of Intensive Care, Caritas Medical Centre, Hong Kong SAR, China
Gavin Matthew Joynt, Department of Anaesthesia and Intensive Care, The Chinese University of Hong Kong, Prince of Wales Hospital, Hong Kong SAR, China
Gladys WM Kwan, Department of Intensive Care, Tuen Mun Hospital, Hong Kong SAR, China
Philip KN Lam, Department of Intensive Care, North District Hospital, Hong Kong SAR, China
Anna Lee, Department of Anaesthesia and Intensive Care, The Chinese University of Hong Kong, Prince of Wales Hospital, Hong Kong SAR, China
E Leung, Adult Intensive Care Unit, Queen Mary Hospital, Hong Kong SAR, China
Steven KH Ling, Department of Intensive Care, Tuen Mun Hospital, Hong Kong SAR, China
CH Ng, Department of Intensive Care, Kwong Wah Hospital, Hong Kong SAR, China
HP Shum, Department of Intensive Care, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, China
Dominic HK So, Department of Intensive Care Unit, Princess Margaret Hospital/Yan Chai Hospital, Hong Kong SAR, China
Charles L Sprung, Department of Anesthesiology, Critical Care and Pain Medicine, Hadassah Medical Organization and Faculty of Medicine, Hebrew University of Jerusalem, Jerusalem, Israel
L Sy, Department of Intensive Care, North District Hospital, Hong Kong SAR, China
Polly NW Tsai, Adult Intensive Care Unit, Queen Mary Hospital, Hong Kong SAR, China
HH Tsang, Department of Intensive Care, Kwong Wah Hospital, Hong Kong SAR, China
WT Wong, Department of Anaesthesia and Intensive Care, The Chinese University of Hong Kong, Prince of Wales Hospital, Hong Kong SAR, China
References
1. Joynt GM, Lipman J, Hartog C, et al. The Durban World
Congress Ethics Round Table IV: health care professional
end-of-life decision making. J Crit Care 2015;30:224-30. Crossref
2. Vincent JL. Forgoing life support in western European
intensive care units: the results of an ethical questionnaire.
Crit Care Med 1999;27:1626-33. Crossref
3. Sprung CL, Truog RD, Curtis JR, et al. Seeking worldwide
professional consensus on the principles of end-of-life
care for the critically ill. The Consensus for Worldwide
End-of-Life Practice for Patients in Intensive Care
Units (WELPICUS) study. Am J Respir Crit Care Med
2014;190:855-66. Crossref
4. Phua J, Joynt GM, Nishimura M, et al. Withholding and
withdrawal of life-sustaining treatments in low-middle-income
versus high-income Asian countries and regions.
Intensive Care Med 2016;42:1118-27. Crossref
5. Lobo SM, De Simoni FH, Jakob SM, et al. Decision-making
on withholding or withdrawing life support in the ICU: a
worldwide perspective. Chest 2017;152:321-9. Crossref
6. Wong WT, Phua J, Joynt GM. Worldwide end-of-life
practice for patients in ICUs. Curr Opin Anaesthesiol
2018;31:172-8. Crossref
7. Attitudes of critical care medicine professionals concerning
forgoing life-sustaining treatments. The Society of Critical
Care Medicine Ethics Committee [editorial]. Crit Care
Med 1992;20:320-6. Crossref
8. Yap HY, Joynt GM, Gomersall CD. Ethical attitudes of
intensive care physicians in Hong Kong: questionnaire
survey. Hong Kong Med J 2004;10:244-50.
9. Yaguchi A, Truog RD, Curtis JR, et al. International differences in end-of-life attitudes in the intensive care unit: results of a survey. Arch Intern Med 2005;165:1970-5. Crossref
10. Bito S, Asai A. Attitudes and behaviors of Japanese
physicians concerning withholding and withdrawal of life-sustaining
treatment for end-of-life patients: results from
an Internet survey. BMC Med Ethics 2007;8:7. Crossref
11. Weng L, Joynt GM, Lee A, et al. Attitudes towards ethical
problems in critical care medicine: the Chinese perspective.
Intensive Care Med 2011;37:655-64. Crossref
12. Sprung CL, Cohen SL, Sjokvist P, et al. End-of-life practices
in European intensive care units: the Ethicus study. JAMA
2003;290:790-7. Crossref
13. Avidan A, Sprung CL, Schefold JC, et al. Variations in end-of-life practices in intensive care units worldwide (Ethicus-2): a prospective observational study. Lancet Respir Med 2021;9:1101-10. Crossref
14. Kong X, Yang Y, Gao J, et al. Overview of the health care
system in Hong Kong and its referential significance to
mainland China. J Chin Med Assoc 2015;78:569-73. Crossref
15. Ling L, Ho CM, Ng PY, et al. Characteristics and outcomes
of patients admitted to adult intensive care units in Hong
Kong: a population retrospective cohort study from 2008 to 2018. J Intensive Care 2021;9:2. Crossref
16. Buckley TA, Joynt GM, Tan PY, Cheng CA, Yap FH.
Limitation of life support: frequency and practice in a Hong
Kong intensive care unit. Crit Care Med 2004;32:415-20. Crossref
17. Sprung CL, Ricou B, Hartog CS, et al. Changes in end-of-life
practices in European intensive care units from 1999 to
2016. JAMA 2019;322:1692-704. Crossref
18. Feldman C, Sprung CL, Mentzelopoulos SD, et al. Global
comparison of communication of end-of-life decisions in
the ICU. Chest 2022;162:1074-85. Crossref
19. Mentzelopoulos SD, Chen S, Nates JL, et al. Derivation
and performance of an end-of-life practice score aimed at
interpreting worldwide treatment-limiting decisions in the
critically ill. Crit Care 2022;26:106. Crossref
20. Hospital Authority, Hong Kong SAR Government. Working
Group on review of Hospital Authority Clinical Ethics
Committee (HKCEC) guidelines related to EOL decisionmaking.
HA Guidelines on Life-Sustaining Treatment
in the Terminally Ill. 2020. Available from: https://www.ha.org.hk/haho/ho/psrm/LSTEng.pdf. Accessed 4 Jul 2023.
21. Lesieur O, Herbland A, Cabasson S, Hoppe MA, Guillaume F,
Leloup M. Changes in limitations of life-sustaining
treatments over time in a French intensive care unit: a
prospective observational study. J Crit Care 2018;47:21-9. Crossref
22. Chung RY, Wong EL, Kiang N, et al. Knowledge, attitudes,
and preferences of advance decisions, end-of-life care, and
place of care and death in Hong Kong. A population-based
telephone survey of 1067 adults. J Am Med Dir Assoc
2017;18:367.e19-27. Crossref
23. Food and Health Bureau, Hong Kong SAR Government.
End-of-Life Care: Legislative Proposals on Advance
Directives and Dying in Place Consultation Report. July
2020. Available from: https://www.healthbureau.gov.hk/download/press_and_publications/consultation/190900_eolcare/e_EOL_consultation_report.pdf . Accessed 4 Jul 2023.
24. Fong BY, Yee HH, Ng TK. Advance directives in Hong Kong: moving forward to legislation. Ann Palliat Med 2022;11:2622-30. Crossref
25. Medical Council of Hong Kong. Code of professional
conduct: for the guidance of registered medical
practitioners. Revised October 2022. Available from:
https://www.mchk.org.hk/english/code/files/Code_of_Professional_Conduct_(English_Version)_(Revised_in_October_2022).pdf . Accessed 4 Jul 2023.
26. Benbenishty J, Ganz FD, Anstey MH, et al. Changes in
intensive care unit nurse involvement in end of life decision
making between 1999 and 2016: descriptive comparative
study. Intensive Crit Care Nurs 2022;68:103138. Crossref