MEDICAL PRACTICE
Recommendations for eligibility criteria concerning bariatric and metabolic surgical and endoscopic procedures for obese Hong Kong adults 2024: Hong Kong Society for Metabolic and Bariatric Surgery Position Statement
Shirley YW Liu, FRCS, FHKAM (Surgery)1; Carol MS Lai, FRCS, FHKAM (Surgery)1; Enders KW Ng, FRCS, FHKAM (Surgery)1; Fion SY Chan, FRCS, FHKAM (Surgery)2; SK Leung, FRCS, FHKAM (Surgery)3; Wilfred LM Mui, FRCS, FHKAM (Surgery)4; Daniel KH Tong, FRACS, FHKAM (Surgery)5; Dennis CT Wong, FRACS, FHKAM (Surgery)6; Patricia PC Yam, FRCS, FHKAM (Surgery)3; Simon KH Wong, FRCS, FHKAM (Surgery)1
1 Department of Surgery, Prince of Wales Hospital, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong SAR, China
2 Department of Surgery, Queen Mary Hospital, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong SAR, China
3 Department of Surgery, Tuen Mun Hospital, Hong Kong SAR, China
4 Hong Kong Bariatric and Metabolic Institute, Hong Kong SAR, China
5 Hong Kong Sanatorium & Hospital, Hong Kong SAR, China
6 St Teresa's Hospital, Hong Kong SAR, China
 Full paper in PDF
Full paper in PDF
Abstract
The surgical management of obesity in Hong
Kong has rapidly evolved over the past 20 years.
Despite increasing public awareness and demand
concerning bariatric and metabolic surgery, service
models generally are not standardised across
bariatric practitioners. Therefore, a working group
was commissioned by the Hong Kong Society for
Metabolic and Bariatric Surgery to review relevant
literature and provide recommendations concerning
eligibility criteria for bariatric and metabolic
interventions within the local population in Hong
Kong. The current position statement aims to provide
updated guidance regarding the indications and
contraindications for bariatric surgery, metabolic
surgery, and bariatric endoscopic procedures.
Obesity is a complex multifactorial disease caused
by diverse combinations of genetic, behavioural,
environmental, and endocrine aetiologies. In 2013,
obesity was recognised by the American Medical
Association as a disease state requiring treatment and
prevention efforts.
1 Obesity substantially increases
an individual’s risks of cardiovascular diseases,
metabolic illnesses, musculoskeletal problems, and
cancer. For healthcare policymakers, the financial
burden of treating and preventing obesity and its
related conditions is exponentially growing. At the
community level, reduced workforce productivity
from obesity-related adverse health outcomes can
lead to detrimental impacts on the broader economy.
According to the World Health Organization,
adults are considered overweight when their body
mass index (BMI) is ≥25 kg/m
2 and obese when their
BMI is ≥30 kg/m
2.
2 However, Asian populations have
a higher percentage of body fat and greater metabolic
risk at lower BMIs.
3 A World Health Organization
expert consultation identified potential public health
action points for Asians as 23.0 kg/m
2, 27.5 kg/m
2, 32.5 kg/m
2, and 37.5 kg/m
2; these values generally
were 2.5 kg/m
2 lower than the thresholds established
for Caucasians.
4 Because of differences in body frame
and visceral fat distribution, lower BMI thresholds
were used to define overweight (≥23 kg/m
2) and
obesity (≥25 kg/m
2) in Asians.
3
Similar to other regions of the world, obesity
is a substantial public health problem in Hong
Kong.
5 According to the latest Population Health Survey 2020/22 conducted by the Department of
Health, the prevalences of obesity and overweight in
people aged 15 to 84 years were 32.6% and 22.0%,
respectively.
6 These prevalences indicate that at least
half of the local Hong Kong population faces health
risks associated with overweight or obesity.
Bariatric and metabolic surgery
Bariatric surgery (ie, surgical treatment for obesity)
has been continuously evolving worldwide over the
past 50 years, with increasingly diverse procedural
options and indications.
7 In 1991, the National Institutes of Health published the first international
consensus endorsing the use of gastrointestinal
surgery as treatment for severe obesity.
8 9 Since then,
numerous studies have confirmed the effectiveness
of bariatric surgery in achieving sustainable weight
loss and substantial improvement in co-morbidities
among obese patients.
10 According to a systematic
review and meta-analysis of 22 094 morbidly
obese patients across 136 studies, bariatric surgery
resulted in 61.2% excess weight loss.
10 Resolution
of diabetes, hypertension, and obstructive sleep
apnoea were achieved in 76.8%, 61.7%, and 85.7% of
patients, respectively.
10 In a prospective randomised
trial of 150 morbidly obese diabetic patients,
bariatric surgery plus intensive medical therapy
was associated with significantly better glycaemic
and metabolic outcomes at 5 years compared with
intensive medical therapy alone.
11 Because bariatric
surgery has demonstrated efficacy in treating type
2 diabetes mellitus (T2DM), the term ‘metabolic
surgery’ was established to describe the role of
bariatric interventions in treating T2DM and
metabolic syndrome.
7 16 In 2016, metabolic surgery
was formally endorsed by 44 international diabetes
organisations as a treatment option for adults with
T2DM and obesity (defined as BMI >30 kg/m
2 for
Caucasians and >27.5 kg/m
2 for Asians), particularly
those with co-morbidities which cannot be
controlled by lifestyle changes and pharmacological
therapy.
17
Although operative safety is a concern for
morbidly obese individuals undergoing any type
of major surgery, current evidence suggests that
bariatric surgery has low perioperative mortality
rates, ranging from 0.03% to 0.2%.
12 In a systematic
review and meta-analysis of 161 756 patients
undergoing bariatric surgery, the 30-day mortality
rates ranged from 0.08% to 0.22%, whereas the
postoperative complication rates were between 9.8%
and 17.0%.
13 Currently, the most widely performed bariatric procedures are sleeve gastrectomy and
Roux-en-Y gastric bypass. Common operative
morbidities of sleeve gastrectomy include bleeding,
leakage, stricture, and symptoms of gastroesophageal
reflux.
14 Roux-en-Y gastric bypass is associated with
bleeding, leakage, stricture, stomal ulcer, small
bowel obstruction, internal herniation, and dumping
syndrome.
15 Data from randomised controlled trials
suggest that sleeve gastrectomy and Roux-en-Y
gastric bypass are comparable in terms of 30-day
mortality and morbidity rates.15
Primary bariatric endoscopic intervention
In recent decades, bariatric endoscopic procedures
have been developed for individuals who prefer
less invasive, non-surgical alternatives.
18 These
endoscopic therapies include intragastric space-occupying
devices (intragastric balloons [IGBs]),
gastric aspiration devices, endoluminal bypass
barrier sleeves, the POSE (primary obesity
surgery endoluminal) procedure, endoscopic
sleeve gastroplasty, and duodenal mucosal
resurfacing. All of these procedures can produce
clinically significant short-term weight loss and
improvements in obesity-related co-morbidities.
19
The first bariatric endoscopic intervention in Hong
Kong, IGB therapy, was introduced in 2004. An
early local report confirmed its efficacy in weight
reduction and co-morbidity improvement among
obese patients at 6 months after treatment.
20
Compared with weight-reduction medication, IGB
therapy was associated with better compliance and
superior weight reduction for up to 2 years after
treatment.
21 Because of its efficacy regarding short-term
weight loss and co-morbidity improvement,
IGB therapy can also serve as a bridging treatment
prior to bariatric or other operative interventions; it
facilitates preoperative weight loss that can reduce
anaesthetic risks. Thus, IGB therapy is a justifiable
non-surgical bariatric option for primary weight loss
and preoperative weight loss.
Overview of bariatric and metabolic surgery in Hong Kong
Hong Kong’s first bariatric surgery programme was
established in 2002 at Prince of Wales Hospital,
affiliated with The Chinese University of Hong
Kong.
22 Encouraged by the success and safety of
the early Prince of Wales Hospital obesity surgery
service,
23 increasing numbers of public and private
hospitals have begun to provide bariatric surgical
interventions to obese patients in Hong Kong (
Table).
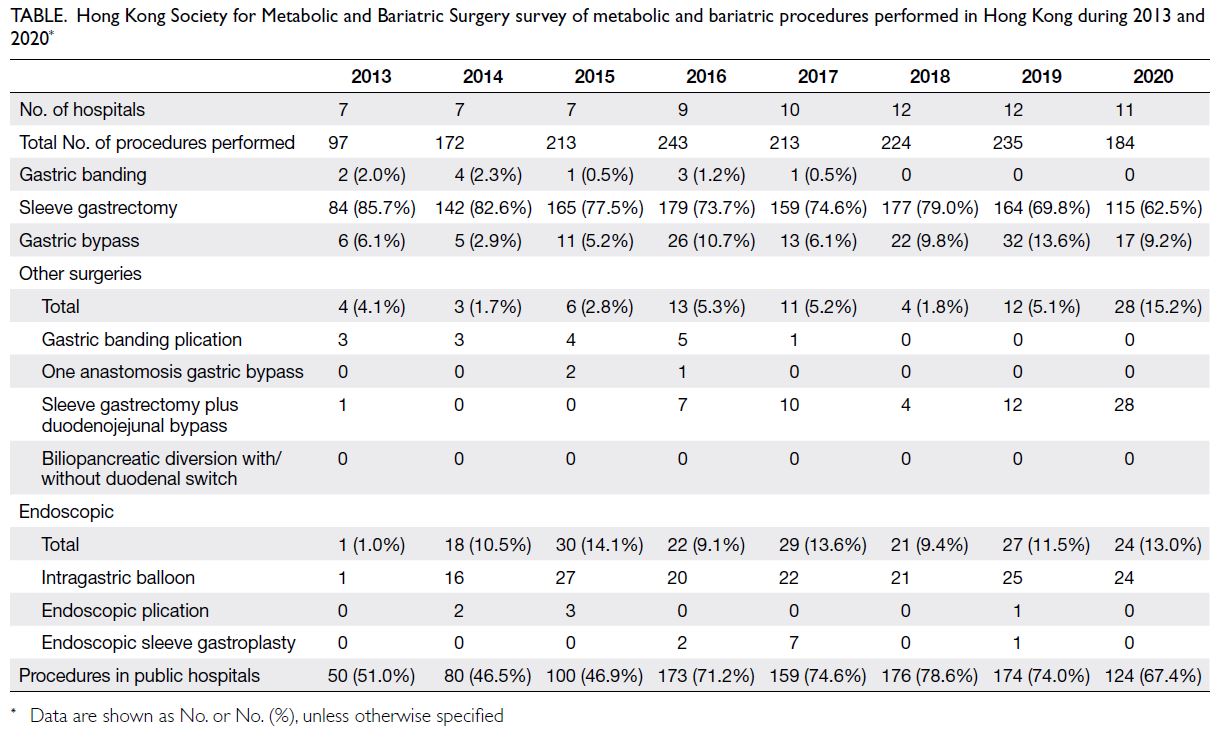
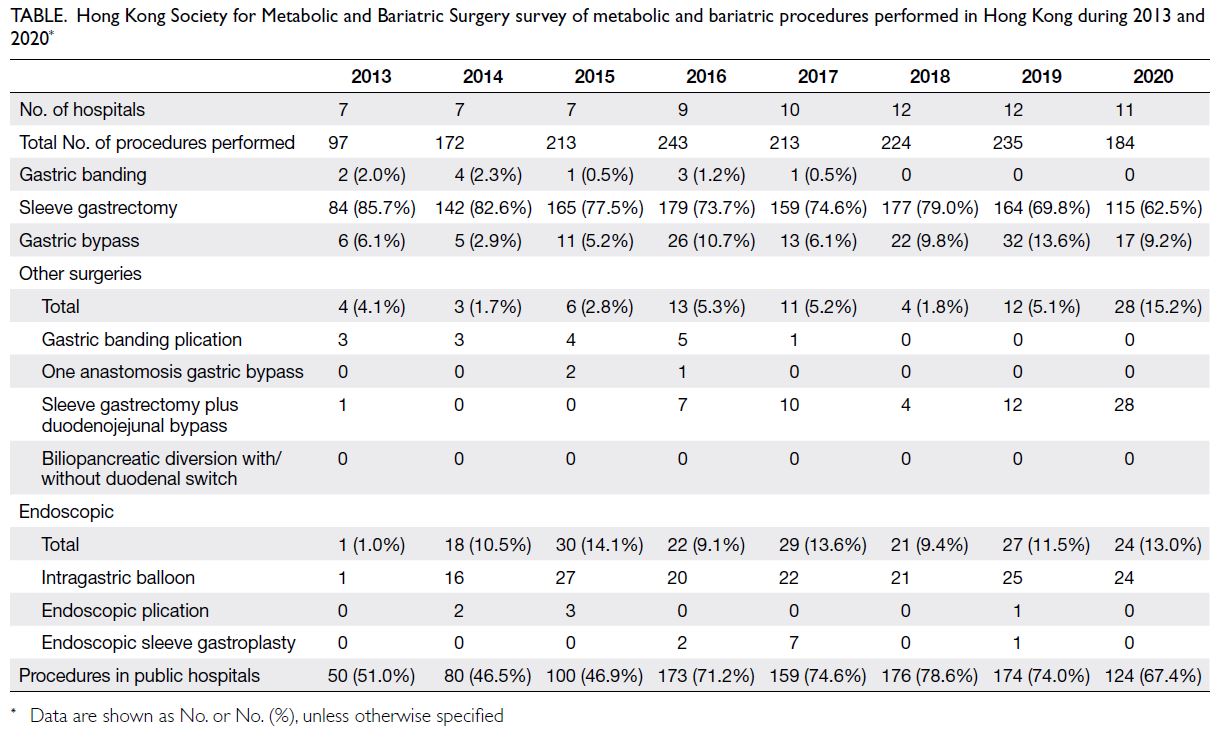 Table.
Table. Hong Kong Society for Metabolic and Bariatric Surgery survey of metabolic and bariatric procedures performed in Hong Kong during 2013 and 2020
With the goal of promoting public and
professional awareness about obesity treatment,
leading local bariatric practitioners formed the Metabolic and Bariatric Surgery Group under the
Hong Kong Association for the Study of Obesity in
2012. In 2017, the Hong Kong Society for Metabolic
and Bariatric Surgery (HKSMBS) was established
as an independent society. Surveys concerning
bariatric surgery types and case volumes are carried
out annually by the two bodies.
Metabolic and bariatric surgery options are
broadly classified as restrictive procedures and
malabsorptive procedures. In Hong Kong, common
restrictive procedures are gastric banding and sleeve
gastrectomy. The most common malabsorptive
procedure is Roux-en-Y gastric bypass. Other
less common malabsorptive procedures are one
anastomosis gastric bypass, sleeve gastrectomy
plus duodenojejunal bypass, and biliopancreatic
diversion with or without duodenal switch.
Between 2013 and 2020, 1582 bariatric surgical and
endoscopic procedures were performed in Hong
Kong (Table). Compared with 2002 when bariatric
surgery was first introduced, the number of bariatric
surgeries performed each year has exponentially
increased from <10 cases per year to >180 cases
per year in 2020. Current data indicate that more
than two-thirds of these surgeries are performed
in government hospitals. Sleeve gastrectomy is the most common bariatric procedure in Hong Kong
(~70%) and the second most common procedure is
Roux-en-Y gastric bypass. Gastric banding, popular
two decades ago, has not been favoured since 2013
(<2.5%). Biliopancreatic diversion with or without
duodenal switch has not been performed in Hong
Kong in the past ten years (
Table).
Development of the position statement
Although extensive international guidelines for
bariatric surgery have been established by various
bariatric authorities,
24 25 26 27 some of the existing
recommendations are not applicable to the Hong
Kong Chinese population because of ethnic and
practical differences. Nevertheless, there is a
lack of practical guidelines regarding bariatric
endoscopic interventions for Asian populations.
28
Among local bariatric practitioners, there has
been a lack of consensus regarding the indications,
contraindications, and procedural options for
bariatric surgery. This heterogeneity in clinical
practices surrounding bariatric surgery in Hong
Kong requires a position statement to address the
concerns of local bariatric practitioners.
In 1991, the National Institutes of Health
published a consensus statement regarding
indications for bariatric surgery; it utilised BMI
thresholds of ≥40 kg/m
2 or ≥35 kg/m
2 with co-morbidities
for Caucasians.
9 The American
Society for Metabolic and Bariatric Surgery and
International Federation for the Surgery of Obesity
and Metabolic Disorders recently updated the
indications for metabolic and bariatric surgery.
29
Their joint statement suggested a new threshold
of ≥35 kg/m
2 to receive a recommendation for
metabolic or bariatric surgery, regardless of the
presence, absence, or severity of co-morbidities.
Additionally, metabolic and bariatric surgery should
be considered for individuals with metabolic disease
and BMI ≥30 kg/m
2. For Asian populations, the joint
statement suggested that BMI thresholds should
be adjusted; specifically, individuals with BMI
>27.5 kg/m
2 should be offered metabolic and
bariatric surgery options.
29 In response to these
revised BMI thresholds for metabolic and bariatric
surgery, published in December 2022, extensive
discussions and debates have arisen in various
professional bodies focusing on metabolic and
bariatric surgery in Asia, including groups in
Hong Kong. Due to limited experience offering
metabolic and bariatric surgery to patients with BMI
<30 kg/m
2 in Hong Kong and other parts of Asia,
long-term surgical risks and benefits for such
patients have not been fully elucidated. Considering
that metabolic and bariatric surgery options are
associated with higher risks of perioperative
morbidity in patients with lower BMI, the HKSMBS
has reached a consensus to refrain from adopting
the newly updated BMI threshold of ≥27.5 kg/m
2
to receive a recommendation for metabolic and
bariatric surgery in this position statement.
The following position statement is issued
by the HKSMBS to define the indications and
contraindications for bariatric procedures and
endoscopic interventions which are suitable for the
Hong Kong population. The recommendations of
this position statement are based on current clinical
knowledge, expert opinion, and published peer-reviewed
scientific evidence.
25 26 27 28
General recommendations
The HKSMBS recommends that bariatric and
metabolic surgery be performed by surgeons
with specialised experience and training in these
procedures. Additionally, such procedures should be
conducted at facilities with multidisciplinary teams
of experts for appropriate perioperative assessment
and follow-up care. The multidisciplinary team may
include experienced surgeons, internal medicine
physicians, weight management coordinators,
nutritionists, exercise physiologists, and
psychologists or mental health professionals.
Eligibility for bariatric surgery
We define bariatric surgery as any surgical
procedure primarily intended for weight reduction
to improve physical and mental health in patients
with severe obesity. After careful review of available
data concerning the safety and efficacy of surgery
for obesity and weight-related diseases, as well as
the effectiveness of such surgery as treatment for
obesity and related co-morbidities, the position
statement committee reached a consensus on
the recommendation of bariatric surgery for the
following eligible candidates in the Hong Kong
adult population (aged ≥18 years) who are unable to
sustain weight loss through optimal lifestyle, dietary
or non-surgical interventions:
30
- appropriate surgical candidates who have a BMI
≥35 kg/m2 with or without obesity-related co-morbidities;
and
- appropriate surgical candidates who have a BMI
≥30 kg/m2 with clinically significant obesity-related
co-morbidities.
We define obesity-related co-morbidities as
conditions either directly caused by obesity or known
to contribute to the presence or severity of obesity.
These comorbid conditions are expected to improve
or resolve with effective and sustained weight loss.
The list of comorbid conditions includes, but is
not limited to, metabolic syndrome,31 T2DM, non-alcoholic
steatohepatitis, obstructive sleep apnoea
syndrome, degenerative arthritis, and polycystic
ovarian syndrome.
Eligibility for metabolic surgery
We define metabolic surgery as any surgical
procedure primarily intended to improve glycaemic
control in obese patients with T2DM. For adults (aged
≥18 years) with T2DM who are unable to sustain
weight loss through optimal lifestyle interventions,
metabolic surgery is recommended for the following
eligible candidates in treating T2DM with the
primary aim of glycaemic improvement:
17
- appropriate surgical candidates with BMI ≥37.5
kg/m2, regardless of the level of glycaemic control
or complexity of glucose-lowering regimens; and
- appropriate surgical candidates with BMI ranging
from 32.5 to 37.4 kg/m2 whose hyperglycaemia
is inadequately controlled by optimal medical,
lifestyle, dietary, and non-surgical interventions.
In addition, metabolic surgery can be regarded
as a treatment option for T2DM in appropriate
surgical candidates with BMI ranging from 27.5 to
32.4 kg/m2 whose hyperglycaemia is inadequately
controlled despite optimal medical control by either
oral or injectable medications (including insulin)
and lifestyle interventions.
We consider hyperglycaemia to be inadequately
controlled if the glycated haemoglobin level is >7.0% despite medical treatment involving two or
more oral hypoglycaemic agents or any injectable
medications (including insulin or glucagon-like
peptide-1 receptor agonist) for >6 months.
32 33
Fasting C-peptide levels should be checked if type 1
diabetes mellitus or latent autoimmune diabetes in
adults is suspected.
Eligibility for bariatric endoscopic
interventions
Intragastric balloon therapy
Intragastric balloon therapy is a minimally invasive
space-occupying system intended to provide
temporary weight loss by reducing gastric volume
and altering gastric motility.
34 35 The following
recommendations regarding IGB therapy are suggested:
1. As a bridging treatment for preoperative weight
loss, IGB therapy can be considered:
a. prior to metabolic or bariatric surgery for the optimisation of medical and/or anaesthetic status in severely obese individuals with very high BMI (eg, >50 kg/m2) who fail to respond to non-surgical optimisation; and
b. prior to non-bariatric surgery (eg, joint replacement surgery, ventral hernia repair, etc) for the optimisation of medical and/or anaesthetic status in obese individuals with BMI >30 kg/m2.
2. As a primary interventional treatment, IGB therapy can be considered:
a. in individuals with BMI ranging from 27.5 to 32.5 kg/m2 (30-35 kg/m2 for Caucasians) who fail to achieve weight loss through optimal lifestyle and dietary interventions; and
b. in obese individuals who meet the eligibility criteria for bariatric or metabolic surgery but are surgically unfit or reluctant to undergo bariatric or metabolic surgery.
3. Intragastric balloon therapy should be used for a
duration shorter than the maximum approved or
recommended duration (usually 4 to 12 months,
depending on IGB brand), or for a duration to be
decided on a case-by-case basis. Patients should
be informed about the intended duration of use.
Other endoscopic procedures
Currently, many restrictive and malabsorptive endoscopic procedures are available. These include,
but are not limited to, the following:
- space-occupying restrictive gastric devices (eg,
TransPyloric Shuttle, SatiSphere, Plenity, etc);
- gastric diversion devices (eg, AspireAssist
aspiration therapy);
- endoscopic gastric plication techniques (eg,
endoscopic sleeve gastroplasty, the POSE
procedure); and
- malabsorptive techniques (eg, duodenojejunal
bypass liner).
Some of these procedures have been approved
by the United States Food and Drug Administration,
whereas others remain investigational in most
countries. Except for endoscopic gastric plication,
AspireAssist aspiration therapy and endoscopic
sleeve gastroplasty, most of these endoscopic
procedures have not been explored in Hong Kong.
Due to the lack of scientific evidence and universal
consensus regarding their indications, efficacy, and
safety, these procedures should only be conducted
after careful evaluation and the acquisition of
informed patient consent and/or approval from
institutional review board.
Contraindications
Despite the beneficial effects of metabolic and
bariatric surgery with clinically significant
improvements in obesity-related co-morbidities,
these procedures are not without surgical and
anaesthetic risks. Moreover, most bariatric
procedures involve a gastric restrictive component;
an individual’s ability to maintain postoperative
dietary and lifestyle changes can substantially affect
surgical outcomes. Therefore, the position statement
committee reached a consensus on the following
suggestions.
Contraindications for bariatric and metabolic surgical and endoscopic interventions
Bariatric and metabolic surgical and endoscopic
procedures should not be performed in the following
situations or for the following individuals:
1. absence of multidisciplinary medical, dietary,
and behavioural guidance;
2. no fully informed consent from the patient or his/
her guardian regarding the risks, benefits, and
real expectations for weight loss, co-morbidity
management, and durability;
3. individuals with BMI <27.5 kg/m
2 (<30 kg/m
2
for Caucasians), unless the procedures are
performed under a research protocol approved
by a local institutional review board and/or
research ethics committee and informed patient
consent has been obtained;
4. individuals with medical conditions which
cannot be optimised before surgery, leading to
significantly increased anaesthetic and operative
risks. These conditions include, but are not
limited to, the following:
a. very high anaesthetic risk (defined as grade IV under the classification system of the American Society of Anesthesiologists) with organ failure that cannot be optimised and represents a constant threat to life;
b. uncontrolled endocrine disorders (eg, hypothyroidism, Cushing’s syndrome, drug-induced obesity, etc);
c. active infection (eg, tuberculosis, human immunodeficiency virus, etc);
d. uncorrected coagulopathy;
e. end-stage liver cirrhosis with or without portal venous hypertension;
f. uncontrolled enteropathy (eg, inflammatory bowel disease, protein-losing enteropathy, etc);
g. disseminated malignancy or advanced malignancy with <5 years of remission; and
h. uncontrolled major organ dysfunction (eg, cardiac, pulmonary, or renal disorders);
5. individuals with conditions that impair their
understanding of surgery and preclude them
from maintaining perioperative lifestyle changes.
These conditions include, but are not limited to,
the following:
a. inadequately controlled psychiatric illnesses (eg, untreated schizophrenia, major depression, bipolar affective disorder, eating disorders, etc);
b. major depression with suicidal ideation and/or attempt within the past year;
c. personality disorder involving poor compliance with instructions; and
d. active substance abuse/alcoholism;
6. individuals with potential non-compliance
problems regarding perioperative dietary and
lifestyle changes. These conditions include, but
are not limited to, the following:
a. intellectual/mental disability;
b. syndromic/genetic disease leading to obesity;
c. condition causing immobility (eg, paraplegia, stroke, etc); and
d. inability to attend regular follow-up.
Moreover, bariatric and metabolic surgical
and endoscopic procedures should not be offered to
pregnant women.
Contraindications specific to intragastric
balloon therapy
Generally, individuals with the above
contraindications for bariatric and metabolic
surgical interventions are also not recommended
to undergo IGB therapy. However, there are
additional contraindications for IGB therapy. These
contraindications include, but are not limited to, the
following, where IGB therapy is not recommended
for individuals:
- with contraindications for endoscopies, allergies
to proton-pump inhibitors, or allergies to balloon
materials (eg, silicone, polyurethane, etc);
- with active gastrointestinal pathology (eg, peptic
ulcers, gastroesophageal varices, inflammatory
bowel disease, etc), altered gastrointestinal
anatomy (eg, previous gastrointestinal surgery,
large hernia, suspect gastrointestinal malignancy, etc), gastrointestinal motility disorders, or a
history of idiopathic acute pancreatitis; and
- actively using anticoagulants or antiplatelet
medications, or individuals with a bleeding
tendency.
For patients who are intended to undergo
swallowable IGB therapy without prior endoscopy,
a preoperative endoscopic examination should be
considered if gastrointestinal pathology (eg, peptic
ulcer, large hiatus hernia, etc) is suspected based on
clinical assessment.
Conclusion
This position statement is not intended to provide
inflexible rules or requirements of practice, nor
to establish a local standard of care. Clinical
practitioners must use their own judgement in
selecting the best evidence-based treatment for
patients with informed consent. Physicians should
follow a reasonable course of action based on current
knowledge, available resources, and the needs of
the patient to deliver effective and safe medical
care. The sole purpose of this position statement is
to assist practitioners in achieving this objective.
This position statement was developed under the
auspices of HKSMBS position statement committee
and approved by the members of executive council.
These recommendations were considered valid at
the time of production based on the data available.
New developments in medical research and practice
will be reviewed, and the position statement will be
periodically updated.
Author contributions
Concept or design: All authors.
Acquisition of data: SKH Wong.
Analysis or interpretation of data: SYW Liu, SKH Wong.
Drafting of the manuscript: SYW Liu, CMS Lai, SKH Wong.
Critical revision of the manuscript for important intellectual
content: SYW Liu, CMS Lai, SKH Wong.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Declaration
This position statement has been endorsed by the Hong Kong
Association for the Study of Obesity. An abridged version of
the position statement has been published on the website of
the Hong Kong Society for Metabolic and Bariatric Surgery
(
http://www.hksmbs.org/).
Funding/support
This research received no specific grant from any funding
agency in the public, commercial, or not-for-profit sectors.
References
1. Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight
and obesity in adults: a report of the American College of
Cardiology/American Heart Association Task Force on
Practice Guidelines and The Obesity Society. Circulation
2014;129 (25 Suppl 2):S102-38.
Crossref2. World Health Organization. Obesity and overweight.
Available from:
https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight . Accessed 14 May 2024.
3. Ko GT, Tang J, Chan JC, et al. Lower BMI cut-off value to
define obesity in Hong Kong Chinese: an analysis based on
body fat assessment by bioelectrical impedance. Br J Nutr
2001;85:239-42.
Crossref4. WHO Expert Consultation. Appropriate body-mass index
for Asian populations and its implications for policy and
intervention strategies. Lancet 2004;363:157-63.
Crossref5. Obesity: preventing and managing the global epidemic.
Report of a WHO consultation [editorial]. World Health
Organ Tech Rep Ser 2000;894:i-xii, 1-253.
6. Non-Communicable Disease Branch, Centre for Health
Protection, Department of Health, Hong Kong SAR
Government. Report of Population Health Survey 2020-22
(Part II). 2023. Available from:
https://www.chp.gov.hk/files/pdf/dh_phs_2020-22_part_2_report_eng.pdf. Accessed 14 May 2024.
7. Buchwald H. The evolution of metabolic/bariatric surgery.
Obes Surg 2014;24:1126-35.
Crossref8. Gastrointestinal surgery for severe obesity: National
Institutes of Health Consensus Development Conference
Statement [editorial]. Am J Clin Nutr 1992;55(2
Suppl):615S-619S.
Crossref9. Consensus Development Conference Panel, NIH Conference. Gastrointestinal surgery for severe
obesity. Consensus Development Conference Panel
[editorial]. Ann Intern Med 1991;115:956-61.
Crossref10. Buchwald H, Avidor Y, Braunwald E, et al. Bariatric
surgery: a systematic review and meta-analysis. JAMA
2004;292:1724-37.
Crossref11. Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery
versus intensive medical therapy for diabetes—5-year
outcomes. N Engl J Med 2017;376:641-51.
Crossref12. Arterburn DE, Telem DA, Kushner RF, Courcoulas AP.
Benefits and risks of bariatric surgery in adults: a review.
JAMA 2020;324:879-87.
Crossref13. Chang SH, Stoll CR, Song J, Varela JE, Eagon CJ, Colditz GA.
The effectiveness and risks of bariatric surgery: an updated
systematic review and meta-analysis, 2003-2012. JAMA
Surg 2014;149:275-87.
Crossref14. Liu SY, Wong SK, Lam CC, Yung MY, Kong AP, Ng EK.
Long-term results on weight loss and diabetes remission
after laparoscopic sleeve gastrectomy for a morbidly obese
Chinese population. Obes Surg 2015;25:1901-8.
Crossref15. Lee Y, Doumouras AG, Yu J, et al. Laparoscopic sleeve
gastrectomy versus laparoscopic Roux-en-Y gastric
bypass: a systematic review and meta-analysis of weight
loss, comorbidities, and biochemical outcomes from
randomized controlled trials. Ann Surg 2021;273:66-74.
Crossref16. Buchwald H, Estok R, Fahrbach K, et al. Weight and type
2 diabetes after bariatric surgery: systematic review and
meta-analysis. Am J Med 2009;122:248-56.e5.
Crossref17. Rubino F, Nathan DM, Eckel RH, et al. Metabolic surgery
in the treatment algorithm for type 2 diabetes: a joint statement by International Diabetes Organizations.
Diabetes Care 2016;39:861-77.
Crossref18. Sullivan S, Edmundowicz SA, Thompson CC. Endoscopic
bariatric and metabolic therapies: new and emerging
technologies. Gastroenterology 2017;152:1791-801.
Crossref19. Winder JS, Rodriguez JH. Emerging endoscopic
interventions in bariatric surgery. Surg Clin North Am
2021;101:373-9.
Crossref20. Mui WL, So WY, Yau PY, et al. Intragastric balloon in ethnic
obese Chinese: initial experience. Obes Surg 2006;16:308-13.
Crossref21. Chan DL, Cruz JR, Mui WL, Wong SK, Ng EK. Outcomes
with intra-gastric balloon therapy in BMI <35 non-morbid
obesity: 10-year follow-up study of an RCT. Obes Surg
2021;31:781-6.
Crossref22. Wong SK, So WY, Yau PY, et al. Laparoscopic adjustable
gastric banding for the treatment of morbidly obese
patients: early outcome in a Chinese cohort. Hong Kong
Med J 2005;11:20-9.
23. Wu T, Wong SK, Law BT, et al. Bariatric surgery is expensive
but improves co-morbidity: 5-year assessment of patients
with obesity and type 2 diabetes. Br J Surg 2021;108:554-65.
Crossref24. Mechanick JI, Kushner RF, Sugerman HJ, et al. American
Association of Clinical Endocrinologists, The Obesity
Society, and American Society for Metabolic & Bariatric
Surgery medical guidelines for clinical practice for the
perioperative nutritional, metabolic, and nonsurgical
support of the bariatric surgery patient. Obesity (Silver
Spring) 2009;17 Suppl 1:S1-70, v.
Crossref25. Mechanick JI, Youdim A, Jones DB, et al. Clinical practice
guidelines for the perioperative nutritional, metabolic, and
nonsurgical support of the bariatric surgery patient—2013
update: cosponsored by American Association of Clinical
Endocrinologists, The Obesity Society, and American
Society for Metabolic & Bariatric Surgery. Obesity (Silver
Spring) 2013;21 Suppl 1(01):S1-27.
Crossref26. Mechanick JI, Apovian C, Brethauer S, et al. Clinical
practice guidelines for the perioperative nutrition,
metabolic, and nonsurgical support of patients undergoing
bariatric procedures—2019 update: cosponsored by
American Association of Clinical Endocrinologists/American College of Endocrinology, The Obesity Society,
American Society for Metabolic and Bariatric Surgery,
Obesity Medicine Association, and American Society of
Anesthesiologists. Obesity (Silver Spring) 2020;28:O1-58.
Crossref27. Di Lorenzo N, Antoniou SA, Batterham RL, et al. Clinical
practice guidelines of the European Association for
Endoscopic Surgery (EAES) on bariatric surgery: update
2020 endorsed by IFSO-EC, EASO and ESPCOP. Surg
Endosc 2020;34:2332-58.
Crossref28. ASGE/ASMBS Task Force on Endoscopic Bariatric
Therapy. A pathway to endoscopic bariatric therapies. Surg
Obes Relat Dis 2011;7:672-82.
Crossref29. Eisenberg D, Shikora SA, Aarts E, et al. 2022 American
Society for Metabolic and Bariatric Surgery (ASMBS) and
International Federation for the Surgery of Obesity and
Metabolic Disorders (IFSO): indications for metabolic and
bariatric surgery. Surg Obes Relat Dis 2022;18:1345-56.
Crossref30. Kasama K, Mui W, Lee WJ, et al. IFSO-APC consensus
statements 2011. Obes Surg 2012;22:677-84.
Crossref31. Alberti KG, Zimmet P, Shaw J. Metabolic syndrome—a
new world-wide definition. A consensus statement from the International Diabetes Federation. Diabet Med
2006;23:469-80.
Crossref32. NICE guideline [NG28]. Type 2 diabetes in adults:
management. London: National Institute for Health and
Care Excellence (NICE); 2022.
33. Qaseem A, Wilt TJ, Kansagara D, et al. Hemoglobin A1c
targets for glycemic control with pharmacologic therapy
for nonpregnant adults with type 2 diabetes mellitus: a
guidance statement update from the American College of
Physicians. Ann Intern Med 2018;168:569-76.
Crossref34. Gómez V, Woodman G, Abu Dayyeh BK. Delayed gastric
emptying as a proposed mechanism of action during
intragastric balloon therapy: results of a prospective study.
Obesity (Silver Spring) 2016;24:1849-53.
Crossref35. Ali MR, Moustarah F, Kim JJ; American Society
for Metabolic and Bariatric Surgery Clinical Issues
Committee. American Society for Metabolic and Bariatric
Surgery position statement on intragastric balloon therapy
endorsed by the Society of American Gastrointestinal and
Endoscopic Surgeons. Surg Obes Relat Dis 2016;12:462-7.
Crossref