Hong Kong Med J 2024 Apr;30(2):170–2 | Epub 15 Apr 2024
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
The challenge of detecting monoclonal protein in
POEMS syndrome: two case reports
YN Mew, MB, BS, FHKAM (Medicine)1; YO Lam, MB, BS, FHKAM (Medicine)2; TH Luk, MB, ChB, FHKAM (Medicine)1; KF Hui, MB, ChB, FHKAM (Medicine)2; WC Fong, MB, BS, FHKAM (Medicine)1
1 Department of Medicine, Queen Elizabeth Hospital, Hong Kong SAR, China
2 Department of Medicine and Geriatrics, United Christian Hospital, Hong Kong SAR, China
Corresponding author: Dr YN Mew (myn760@hhh.ha.org.hk)
Case presentations
Case 1
A 60-year-old woman presented to United
Christian Hospital in 2019 with a 2-month history
of progressive generalised ascending weakness
and numbness affecting all four limbs. On clinical
examination, she had significant oedema involving
her hands and feet. Proximal limb power was full
while distal limb power was rated grade 3 on the
Medical Research Council scale. Sensory modalities
involving pinprick, light touch and proprioception
were all diminished distally. She had generalised
areflexia. Nerve conduction study revealed
markedly reduced motor conduction velocity at 18
to 28 m/s (normal range, >50) in the upper limbs,
consistent with demyelination. There was evidence
of secondary axonal injury. Limited by significant
oedema, lower limb nerve compound muscle action
potential and sensory nerve action potential were
unrecordable. Cerebrospinal fluid study showed
elevated protein level at 899 mg/L with normal
white blood cell count. The patient was managed
as presumed chronic inflammatory demyelinating
polyneuropathy (CIDP). Evaluation of monoclonal
gammopathy with serum protein electrophoresis
(SPE), urine Bence Jones protein and serum
immunoglobulin pattern was unrevealing. Systemic
steroid was commenced followed by intravenous
immunoglobulin due to disease progression but the
patient deteriorated further with distal power grade
0 and became wheelchair bound.
Repeated SPE and urine Bence Jones protein
test failed to detect any monoclonal gammopathy.
Serum free light chain assay of the patient showed
persistently raised lambda light chain but normal
kappa/lambda ratio. Serum immunofixation was
negative. Six months after her initial presentation,
positron emission tomography–computed
tomography (PET-CT) scan revealed multiple
hypermetabolic bony lesions in the skeleton.
The dominant lesions were mixed lytic-sclerotic
lesions at the left sacrum (maximum standardised
uptake value=22.4) and left L5 vertebra (maximum
standardised uptake value=16.3). Mild inactive bilateral pleural effusion, pericardial effusion as
well as diffuse subcutaneous oedema were also
noted. Random trephine bone marrow examination
performed at the right iliac crest was unremarkable.
At this juncture, the patient developed skin
changes with plethora, white nails, flushing, and
hypertrichosis of the trunk and limbs (Fig). She
was oedematous with orthopnoea and paroxysmal
nocturnal dyspnoea. A diagnosis of POEMS
syndrome (polyneuropathy, organomegaly,
endocrinopathy, monoclonal plasma cell disorder,
and skin changes) was strongly suspected in view
of her polyneuropathy, skin changes, lytic-sclerotic
bone lesion, and extracellular volume overload.
Plasma vascular endothelial growth factor was
checked and was markedly elevated at 370 pg/mL
(reference range, <96.2).
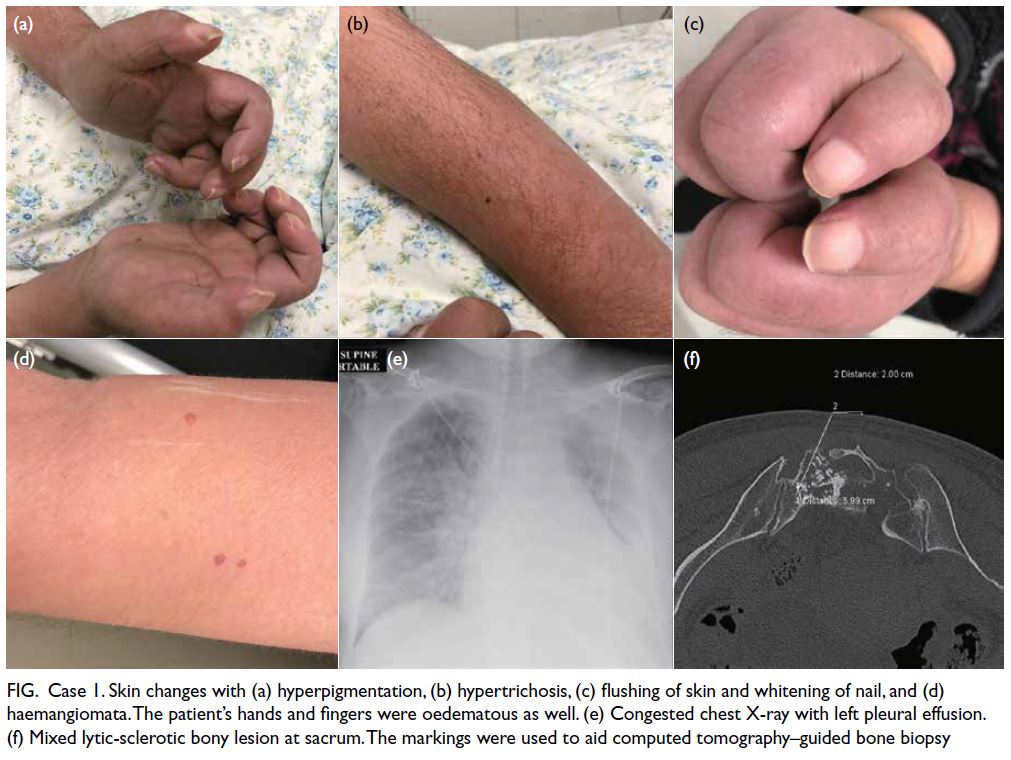
Figure. Case 1. Skin changes with (a) hyperpigmentation, (b) hypertrichosis, (c) flushing of skin and whitening of nail, and (d) haemangiomata. The patient’s hands and fingers were oedematous as well. (e) Congested chest X-ray with left pleural effusion. (f) Mixed lytic-sclerotic bony lesion at sacrum. The markings were used to aid computed tomography–guided bone biopsy
The patient’s fluid overload symptoms
deteriorated with respiratory distress. She was
oxygen dependent and diuretic therapy was only
partially helpful. Therapeutic thoracentesis of the
left chest drained 700 mL of transudative fluid.
She subsequently underwent CT-guided bone
biopsy (Fig). Her sacrum bone biopsy revealed
plasmacytoma with lambda light chain restriction. A
diagnosis of POEMS was confirmed.
Around the same time, DNA from the previous
random bone marrow blood was extracted from
the patient for immunoglobulin heavy chain and
kappa light chain B-cell clonality assay (BIOMED-2
polymerase chain reaction assay). Results revealed
clonal gene rearrangement (targeting Vk-Jk segments
of immunoglobulin kappa gene) consistent with the
presence of a clonal B-cell population.
The patient was prescribed a combination of
bortezomib, cyclophosphamide and corticosteroid.
Oedema resolved first with subsequent improved
limb power and dexterity. Her follow-up PET-CT
scan after 10 months showed similar bony lesions
with reduced metabolic activity.
Case 2
A 40-year-old man presented to Queen Elizabeth Hospital in 2013 with progressive generalised oedema. He had had repeated admissions for bilateral
lower limb oedema, dyspnoea and orthopnoea.
Diuretics were partially helpful. Echocardiogram
showed normal left ventricular ejection fraction
but evidence of pulmonary hypertension. Serum
and urine albumin level was normal. Computed
tomography of the thorax and abdomen revealed
bilateral pleural effusion, pericardial effusion and
ascites. He subsequently developed severe distal
limb weakness and became wheelchair bound.
Nerve conduction study showed demyelinating
sensorimotor polyneuropathy in his upper limbs.
Lower limb nerves were unable to be assessed due to
severe oedema. The patient developed other features
of POEMS with hepatosplenomegaly, papilledema,
skin changes with hypertrichosis and acrocyanosis.
A PET-CT scan revealed sclerotic bony lesions over
the left ilium and multiple thoracic and lumbar
vertebral bodies.
Similar to Case 1, the patient’s serum and urine
were negative for paraprotein. Serum free light chain
assay revealed an unremarkable kappa/lambda ratio.
Random bone marrow aspiration and trephine biopsy
revealed active marrow with mild plasmacytosis.
Targeted left iliac bone biopsy showed plasmacytic infiltrates with reversed kappa/lambda ratio.
Although plasmacytoma was a concern, there were
no definitive histological criteria. Nonetheless based
on the highly compatible clinical features of POEMS,
he was managed accordingly with cyclophosphamide
and corticosteroid. His oedema resolved and he was
subsequently able to mobilise with a stick.
Discussion
The POEMS is a rare paraneoplastic syndrome
caused by plasma cell disorder. Presentation may
mimic that of demyelinating polyneuropathy. The
diagnostic criteria of POEMS include two mandatory
criteria, namely, presence of monoclonal plasma
cell disorder of lambda origin and demyelinating
polyneuropathy. Major criteria include sclerotic
bone lesions, elevated vascular endothelial growth
factor, and Castleman disease; minor criteria include
skin changes, organomegaly, endocrinopathy,
extravascular volume overload, papilledema,
thrombocytosis, and polycythemia.1 The diagnosis
of POEMS is often delayed. The median time for
diagnosis has been reported to be 15 months in a
longitudinal cohort of 100 patients, by which time 35% patients had become bed or wheelchair bound.2
The above two cases illustrate the difficulty in
establishing monoclonal gammopathy even though
neurologists and haematologists were alert to the
possibility of POEMS. Repeated SPE test, Bence
Jones protein test and random bone biopsy were all
negative. Plasmacytoma can be demonstrated only
on targeted bone biopsy. As a mandatory diagnostic
criterion, failure to detect monoclonal gammopathy
delays the subsequent management of POEMS. In
a large retrospective series, positive monoclonal
protein detection on SPE was only 24% to 54%.1
Thorough investigations with serum, urine
and histological samples are essential. These consist
of performing serum protein electrophoresis,
immunofixation, serum free light chain assay
as well as urine equivalents. Failure to perform
immunofixation and serum free light chain
analysis may result in missing 30% of POEMS
cases.3 Haematological advice and laboratory
communication is of utmost importance to exhaust
diagnostic means. For Case 1, immunofixation
was performed after liaison with the laboratory. A
similar situation arises in the United Kingdom where
it is a common practice for laboratories to perform
immunofixation only if a paraprotein is present in
SPE, despite having superior sensitivity.4
Non-targeted bone marrow examination
carries a high chance of missing the pathology,
reflected by a prior case series of six patients in
whom three had their pathology missed.5 Image
guidance, eg, PET-CT, should be considered in the
diagnostic workflow of POEMS. It plays a significant
role not only in detecting abnormal bone lesions, but
also in increasing diagnostic yield for plasmacytoma
in biopsy.
Case 1 also illustrates the diagnostic delay
of POEMS syndrome partly due to a trial of CIDP
treatment, a not uncommon phenomenon. This
issue was addressed in a cost-effective analysis of
POEMS patients in the United Kingdom.4 The study
introduced a diagnostic algorithm incorporating
early mandatory vascular endothelial growth factor
testing in acquired demyelinating neuropathy
patients and helped avoid misdiagnosis and
associated healthcare costs.4
The two cases are also similar in terms of the
debilitation from significant oedema. One should
be alert of POEMS when a CIDP patient presents
with unexplained oedema. Extravascular volume
overload is a common feature of POEMS and can
occur in 90% patients, presumably due to a capillary
leak phenomenon.1 This includes leg oedema, pleural
effusion, pericardial effusion, ascites, papilledema,
and asymptomatic pachymeningeal thickening from
fluid collection. Presence of oedema in POEMS
should not be overlooked as it is a helpful diagnostic
clue to differentiate POEMS from CIDP. It also causes significant patient morbidity. Patients may
require repeated paracentesis if the oedema remains
refractory to diuretics.
These two cases illustrate the challenge
of establishing monoclonal gammopathy in
POEMS. Negative serum and urine paraprotein,
immunofixation, serum free light chain assay, or a
normal random bone marrow examination do not
exclude POEMS and warrant further investigations.
We should be aware of the limitation of test methods.
Comprehensive clinical assessment, thorough
investigations and multidisciplinary communication
are essential for early diagnosis and management.
Author contributions
Concept or design: YN Mew, WC Fong.
Acquisition of data: All authors.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: YN Mew.
Critical revision of the manuscript for important intellectual content: WC Fong, KF Hui.
Acquisition of data: All authors.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: YN Mew.
Critical revision of the manuscript for important intellectual content: WC Fong, KF Hui.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
The authors thank Dr Kwan-hung Leung, haematologist at United Christian Hospital, for contributing to patient management.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patients were managed in accordance with the Declaration of Helsinki and provided informed consent for publication.
References
1. Dispenzieri A. POEMS syndrome: 2019 update on diagnosis, risk-stratification, and management. Am J Hematol 2019;94:812-27. Crossref
2. Keddie S, Foldes D, Caimari F, et al. Clinical characteristics, risk factors, and outcomes of POEMS syndrome: a longitudinal cohort study. Neurology 2020;95:e268-79. Crossref
3. Keddie S, D’Sa S, Foldes D, Carr AS, Reilly MM, Lunn MP. POEMS neuropathy: optimising diagnosis and management. Pract Neurol 2018;18:278-90. Crossref
4. Marsh ES, Keddie S, Terris-Prestholt F, D’Sa S, Lunn MP.
Early VEGF testing in inflammatory neuropathy avoids
POEMS syndrome misdiagnosis and associated costs. J
Neurol Neurosurg Psychiatry 2021;92:172-6. Crossref
5. Li Y, Valent J, Soltanzadeh P, Thakore N, Katirji B.
Diagnostic challenges in POEMS syndrome presenting with
polyneuropathy: a case series. J Neurol Sci 2017;378:170-4. Crossref

