Hong Kong Med J 2024 Feb;30(1):56–61 | Epub 19 Feb 2024
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PERSPECTIVE
Feasible non-surgical options for management of knee osteoarthritis during the COVID-19 pandemic and beyond
JR Khoo, MB, BS1; PK Chan, FHKCOS, FHKAM (Orthopaedic Surgery)1; Chunyi Wen, MB,BS, PhD (Orthopaedic Surgery)2; Lawrence CM Lau, FHKCOS, FHKAM (Orthopaedic Surgery)1; Thomas KC Leung, MB, BS, FHKCOS3; Michelle Hilda Luk, FHKCOS, FHKAM (Orthopaedic Surgery)3; Vincent WK Chan, FHKCOS, FHKAM (Orthopaedic Surgery)3; Amy Cheung, FHKCOS, FHKAM (Orthopaedic Surgery)3; MH Cheung, FHKCOS, FHKAM (Orthopaedic Surgery)1; Henry Fu, FHKCOS, FHKAM (Orthopaedic Surgery)1; KY Chiu, FHKCOS, FHKAM (Orthopaedic Surgery)1
1 Department of Orthopaedics and Traumatology, The University of Hong Kong, Hong Kong SAR, China
2 Department of Biomedical Engineering, The Hong Kong Polytechnic University, Hong Kong SAR, China
3 Department of Orthopaedics and Traumatology, Queen Mary Hospital, Hong Kong SAR, China
Corresponding author: Dr PK Chan (cpk464@yahoo.com.hk)
Introduction
Osteoarthritis (OA) is a common degenerative joint
disease involving progressive deterioration of joint
cartilage and underlying bone. It most commonly
affects the distal interphalangeal, hip, and knee joints
through degeneration resulting in progressive loss of
function, increasing stiffness, and worsening pain.1
Knee OA is a common debilitating disease among
older adults. In 2018, 1.27 million (17.9%) Hong
Kong residents were aged ≥65 years; this number
is projected to double to 2.44 million by 2038.2 The
increasing ageing population and worsening obesity
epidemic are expected to greatly increase the number
of individuals with knee OA. Although early-stage
OA can be asymptomatic, subsequent joint pain
often causes healthcare-seeking behaviour.
Patients with knee OA experience rapidly
worsening pain and decreasing joint functionality
during prolonged inactivity. The social distancing
measures enforced during the coronavirus disease
2019 (COVID-19) pandemic in Hong Kong have
hindered patient adherence to international OA
guidelines.3 Due to the possibility of future pandemics
and outbreaks, it is crucial that we provide patients
with practical non-surgical approaches to pain
management and minimising the risk of progression.
Considering language barriers, treatment availability,
and variations in COVID-19 regulations, locality-specific
recommendations are essential. Primary
healthcare practitioners and Hong Kong residents can
utilise the therapeutic tools described in this article to
promote self-management of knee OA in Hong Kong
throughout the COVID-19 pandemic and beyond.
Overview of knee osteoarthritis treatment during coronavirus disease 2019
A recent analysis of COVID-19 effects on arthroplasty services in Hong Kong showed large (>50%) decreases
in elective arthroplasties and surgical volume from
January to June 2020.4 Although the rate of revision
operations remained similar during this period, the
number of primary arthroplasty operations decreased
by 91%, emphasising the importance of effective
non-surgical treatment options for knee OA.4 The
multifactorial aetiology and slow progression of knee
OA enable implementation of diverse therapeutic
regimens. Non-surgical treatments can be broadly
divided into non-pharmacological (preferred) and
pharmacological options (Fig).
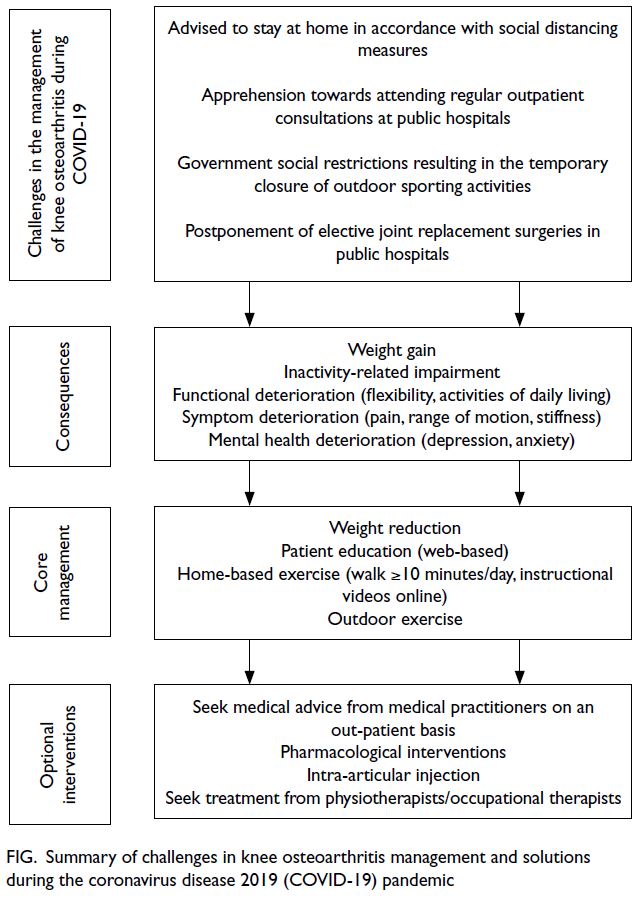
Figure. Summary of challenges in knee osteoarthritis management and solutions during the coronavirus disease 2019 (COVID-19) pandemic
Non-pharmacological treatments
Non-pharmacological options are the first-line
treatment for OA. Despite their high efficacy and
favourable side-effect profiles, such treatments are
often overlooked in favour of pharmacological or
surgical approaches.5 Non-pharmacological options
involve patient education, weight reduction and
exercise, physical and occupational therapy, and
orthotic assistance. Their principle outcomes include
slower disease progression, pain relief, and improved
functionality.
Education
A better understanding of knee OA and its
progression can motivate patients to assume
an active role in their treatment plan, thereby
improving compliance and promoting health-seeking
behaviours. Knowledgeable patients can
recognise relevant symptoms, reducing anxiety and
enabling clear reporting. Patient education also
limits misinformation and misconceptions. In a
qualitative study of patients with hip and knee OA
during the COVID-19 pandemic, most individuals
failed to utilise first-line interventions for OA (ie,
therapeutic exercises) despite pandemic-related
restrictions; they believed that complementary OA treatments (ie, physiotherapy) offered better
therapeutic effects than exercise.6 The Elderly
Health Service, a subsidiary of the Department of
Health of Hong Kong, has published official OA fact
sheets, instructional exercise videos, and treatment
guidelines in Cantonese, English and Mandarin,
facilitating use by the Hong Kong population, where
Cantonese is the first language.7 There are also
other web-based education programmes worldwide
(online supplementary Table 1).
Weight reduction
Knee OA is strongly associated with obesity. The
2014/15 Hong Kong Population Health Survey
revealed that approximately 50% of adults in the
general population were obese or overweight.8 A
meta-analysis9 found that obesity and overweight
increased the risk of knee OA by 35% for every
5 kg/m2 increase in body mass index. Weight
reduction can decrease the mechanical and inflammatory stressors involved in knee OA.
Treatment methods include lifestyle
modification, calorie restriction, regular physical
activity, pharmacological means, and surgical
approaches. Pandemic-related social restrictions have
hampered outdoor physical activity. Additionally,
stress-related calorie intake may increase during
lockdown. Access to outpatient dietetic services has
been limited during the pandemic, hindering patient
accountability for eating habits. In Hong Kong,
telemedicine consultations with dietitians were
more effective than face-to-face dietetic services
for promoting intermediate- and long-term weight
reduction in overweight individuals.10 There is
evidence showing the benefits of weight reduction
on pain and physical disability.11
Exercise
Exercise can help reduce body weight and strengthen
surrounding muscles. Although exercises involving
excessive joint loads should be avoided, low-impact
aerobic exercises can reduce pain, improve limb
mobility, and restore joint function.12 International
OA guidelines recommend multimodal exercise
programmes that incorporate targeted resistance
and flexibility training.3 Resistance programmes can
include resistance training machines (isokinetic)
and body weight (isotonic) exercises to strengthen
quadricep muscles, improving joint stability
and reducing pain severity. Recent COVID-19 restrictions in Hong Kong have resulted in
temporary closures of fitness centres and mandatory
mask usage during physical activity. These new
restrictions have precluded the exercise intensity
needed to improve knee OA outcomes. Nevertheless,
a randomised controlled trial showed that simple
home-based exercises led to 30% reduction in
the WOMAC (Western Ontario and McMaster
Universities Osteoarthritis Index) compared with
educational control and diet groups.13 A prospective
cohort study assessing the effects of the COVID-19
lockdown on hip and knee OA revealed significant
pain exacerbation (according to visual analogue scale
score) and reduced joint functionality (according
to WOMAC score for pain, stiffness, and physical
function) among individuals with decreased physical
activity.14 To prevent inactivity-related impairment,
adults with knee OA are advised to walk at least 10
minutes per day15; this goal is feasible for individuals
confined to their homes during the fifth wave of the
COVID-19 pandemic in Hong Kong.
Physiotherapy
Physiotherapy is important for patients with knee
OA. Full-range active and passive joint movements
can prevent contractures that limit joint function
and precede disability. Resistance training restores
periarticular muscle strength, thus improving physical function, reducing joint pain, and slowing
cartilage degeneration. The clinical effects on
knee OA include improvements in walking speed,
walking distance, timed up and go test outcomes,
and stair climbing. A community-based aquatic
exercise programme for patients with knee OA
recently demonstrated effectiveness and feasibility
in Hong Kong. Improvements in joint functionality
and quadricep strength were observed after 10
weeks of physiotherapist-led aquatic exercises.16
Although pandemic-related rehabilitation service
disruption interrupted treatment for some
patients, tele-rehabilitation usage in Hong Kong
significantly increased during the pandemic.17
Among 9101 patients utilising tele-rehabilitation,
rates of satisfaction and adherence to prescribed
rehabilitation activities were high; moreover, 1112
therapists (50.6% of the workforce) prescribed tele-rehabilitation
during the pandemic.17
Orthotics
Considering their affordability, negligible adverse
effects, and relative ease of application, braces are
ideal for Hong Kong patients with knee OA in the
COVID-19 era. The use of a soft knee brace improves
knee instability and functionality. A cohort study of
bracing and orthotics efficacy showed improvements
in pain and joint functionality among patients with
knee OA in Hong Kong after 24 weeks.18 Although
shoe insoles had a compliance rate exceeding
90%, bracing had a compliance rate of 54.5%; skin
discomfort in the hot and humid climate contributed
to poor adherence.18
Transcutaneous electrical nerve stimulation
Transcutaneous electrical nerve stimulation
has become a convenient option for in-home
pain relief among patients with knee OA. Retail
chains throughout Hong Kong offer affordable
stimulation devices, reducing barriers to treatment.
A recent randomised controlled trial demonstrated
considerable improvements in the visual analogue
scale score for pain and distance walked in the 6-minute walk test, following a trial of transcutaneous
electrical nerve stimulation in patients with minimal
knee pain.19
Pharmacological treatments
Pharmacological agents may be indicated for patients
with recalcitrant symptomatic knee OA. No available
pharmacological therapies for knee OA are disease-modifying;
they should only be used during symptom
worsening. A step-up approach should be utilised
regarding pharmacological treatments, with careful
and deliberate assessment of the clinical context
before administration. According to international
guidelines, paracetamol is not considered first-line firstline
treatment for knee OA because of its clinically
insignificant effects on pain management.3 However,
Hong Kong guidelines recommend paracetamol as
first-line treatment.20
Non-steroidal anti-inflammatory drugs
Topical and oral formulations of non-steroidal anti-inflammatory
drugs (NSAIDs) can be administered
to patients with knee OA. Under Hong Kong and
international guidelines, topical NSAIDs are strongly
recommended for the first-line management of knee
OA because of their pain management efficacy
and satisfactory safety.20 Patients with inadequate
symptom relief from topical NSAIDs may transition
to oral NSAIDs with satisfactory gastrointestinal,
cardiovascular, and renal profiles. The minimum
necessary dose of oral NSAIDs for pain control
should be used because of possible side-effects.
Patients with gastrointestinal complications
should receive a proton pump inhibitor along with
NSAIDs.21
Glucosamine and chondroitin sulphate
Glucosamine and chondroitin sulphate are
considered safe and useful conservative treatments
in oral supplement form. Both compounds have anti-inflammatory
and immunomodulatory activities that
can decrease cartilage degeneration and increase
hyaluronic acid (HA) synthesis.22 Despite strong
international recommendations against glucosamine
usage, Hong Kong guidelines support its application
in mild to moderate knee OA.20 Although active
prescribing of glucosamine and chondroitin sulphate
is discouraged, clinicians should not prohibit its use
among patients who experience clear benefits.
Opioids
Opioid administration for pain relief should be
reserved for patients with severe recalcitrant pain.
Similar to NSAIDs, the minimum necessary dosage
of opioids should be used while monitoring for
common side-effects. Opioid use is discouraged
because of negative impacts on patients and society.
The high incidences of short-term side-effects and
long-term consequences highlight the importance
of limiting opioid use.23 There is a negligible pain
reduction benefit during long-term use of opioid
medications for knee OA. The risks of opioid use
consistently outweigh the benefits of such treatment.
Clinicians should utilise alternative non-surgical
treatments in a stepwise manner.23
Topical capsaicin
Topical capsaicin is an alternative treatment
option for patients with mild recalcitrant knee OA.
Capsaicin alleviates pain by depleting substance P
and inhibiting the TRPV1 receptor on nociceptive sensory neurons. Prolonged capsaicin application
can desensitise nociceptive fibres and inhibit
pain transmission. Low-concentration capsaicin
formulations have consistently demonstrated
safety and efficacy. Nevertheless, topical NSAIDs
remain preferable as first-line treatment for knee
OA because of their favourable side-effect profile
and greater evidence of efficacy. A trial regimen of
capsaicin should be offered to patients with a poor
response (or contraindications) to topical NSAIDs.24
Injection
Intra-articular corticosteroids
Intra-articular corticosteroids are useful for
patients with symptoms recalcitrant to NSAIDs.
Although they are highly effective in reducing
short-term pain, they have poor long-term efficacy.3
Corticosteroids exhibit both anti-inflammatory and
immunosuppressive effects: after treatment, patients
typically experience improved joint mobility and
rapid reductions of erythema, swelling, heat, and
tenderness in affected joints.3 Frequent intra-articular
corticosteroid use should be avoided
because of the increased infection risk and potential
damage to joints and cartilage.
Intra-articular hyaluronic acid
Hyaluronic acid, a naturally occurring
glycosaminoglycan, increases the viscosity and
elasticity of synovial fluid, thereby facilitating
joint lubrication and reducing cartilage stress.
Additionally, HA has anti-inflammatory and
chondroprotective properties. Elevated levels of
inflammatory cytokines and proteolytic enzymes in
OA interfere with these properties and contribute to
knee joint deterioration.25 Intra-articular injection of
HA may restore viscoelasticity to synovial fluid. A
Cochrane review comparing intra-articular HA with
corticosteroids revealed no significant differences 4
weeks after administration; however, intra-articular
HA was more effective 5 to 13 weeks after injection.26
Other studies have shown that HA treatment for
moderate OA decreased the mean number of opioid
prescriptions (both existing and new), improved the
maintenance of medial and lateral joint space areas,
and delayed the need for total knee replacement
surgery.27 Although various intra-articular HA
preparations exist (online supplementary Table 2), their clinical effects remain controversial
because of conflicting data. The American College
of Rheumatology and American Academy of
Orthopaedic Surgeons do not recommend using HA
as an analgesic for OA. Although there is evidence
of HA safety and efficacy in knee OA, this expensive
treatment may be unsuitable for some patients.26
In Hong Kong, HA is recommended because it
significantly reduces pain and has an excellent safety profile. A study of hylan G-F 20 injection safety
and efficacy among patients with knee OA in Hong
Kong showed significant improvements in pain and
function over 6 months after a single 6-mL intra-articular
injection; that study also demonstrated
the feasibility of locality-wide HA use in outpatient
settings.28
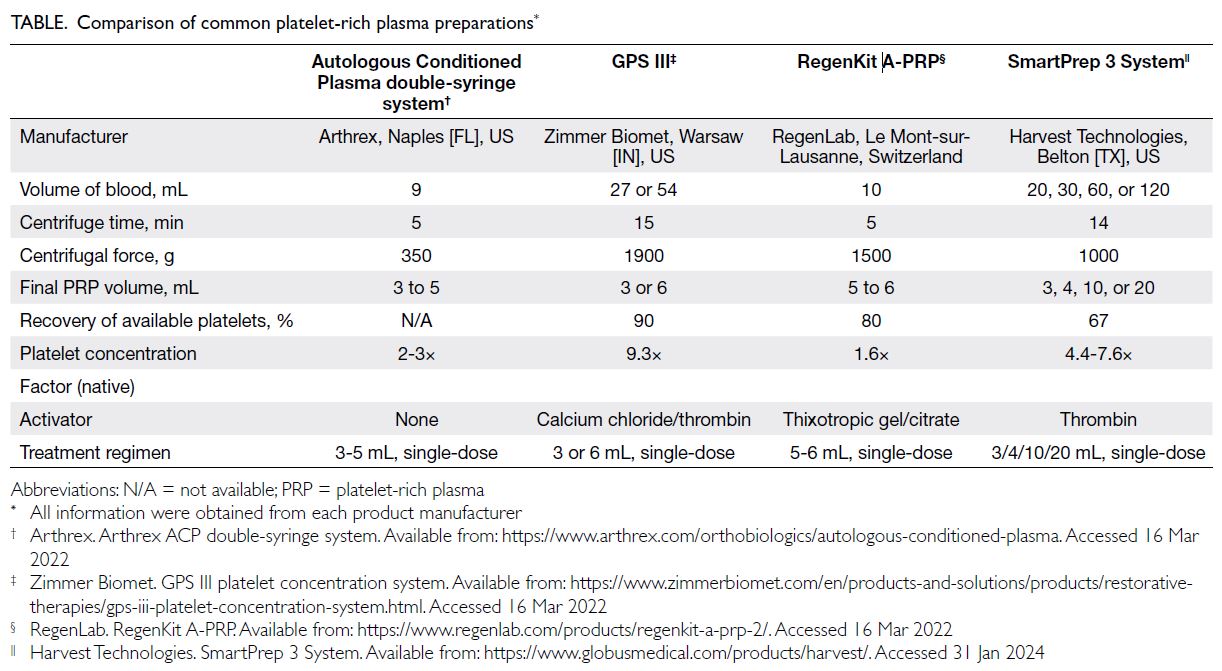
Platelet-rich plasma
Platelet-rich plasma (PRP) is a minimally invasive,
inexpensive method to obtain biologically active
molecules for the treatment of knee OA.29 Whereas
HA requires exogenous fermentation, PRP is
obtained by centrifugation of autologous blood.
There are four common PRP preparations (Table).
Extracted plasma can exhibit considerably higher
concentrations of platelets compared with normal
blood. The extracted platelets degranulate upon
reinjection, releasing growth factors and bioactive
molecules that promote healing at injured sites.
Improvements in chondrocyte apoptosis, cartilage
proteoglycan concentrations, and OA progression
have been observed after intra-articular injection
of PRP. Furthermore, pain relief, knee function,
and quality of life are improved, compared with
HA level.30 The Osteoarthritis Research Society
International discourages PRP usage considering the
low quality of evidence and lack of standardisation
among formulations. However, applications of PRP
persist in private clinics in Hong Kong; thus, patients
and clinicians should be knowledgeable regarding
the available formulations.
Mesenchymal stem cells
Mesenchymal stem cells (MSCs) are multipotent
progenitors that can be obtained from numerous
tissues. Although they do not have unlimited
differentiation potential, MSCs are preferred
among stem cell treatments for OA because of
their widespread availability.31 The pluripotency
of MSCs enables differentiation into osteoblasts,
chondrocytes, and adipocytes, facilitating the
recovery of knee joints with OA. Additionally, MSCs
secrete cytokines and growth factors with anti-inflammatory
and immunomodulatory properties
that can enhance cartilage regeneration, reduce
inflammation, and improve angiogenesis. Primary
isolated stromal cells constitute the best option for
knee OA treatment. Bone marrow–derived stromal
cells (from the posterior superior iliac spine) and
adipose tissue–derived stromal cells (from the
infrapatellar fat pad and subcutaneous sites) are
most commonly utilised in clinical settings.32 Despite
the promising potential of MSCs, existing evidence
has been obtained from small uncontrolled studies
with diverse cell preparation methods and short
follow-up. The optimal tissue source and cell dose
also remain unclear, hindering conclusions about the clinical effects of MSCs. Randomised controlled
trials with larger patient cohorts are needed to
confirm the safety and efficacy of MSCs in knee OA.
Exacerbation of knee pain during coronavirus disease 2019
Numerous underlying aetiologies may explain the
pronounced exacerbation of OA-related knee pain
throughout the COVID-19 pandemic. Prolonged
inactivity and inadequate non-surgical management
have been associated with worsening knee pain and
joint functionality during the pandemic.14 There
have also been reports of COVID-19–related
arthritis; although its clinical presentation was
similar to knee OA, affected patients had reactive
or inflammatory arthritis that could require disease-modifying
antirheumatic drugs.33 Accordingly,
primary healthcare practitioners should make
referrals to appropriate specialists when doubt
arises.
Conclusion
Social distancing measures during the COVID-19
pandemic have hindered care for patients with knee
OA. Prolonged inactivity has been associated with
worsening symptoms, disease progression, and poor
functional outcomes. The non-surgical modalities
highlighted in this article are specifically tailored to
the Hong Kong population; they are feasible under stringent social distancing. Primary healthcare
practitioners should utilise and promote these tools
to enhance self-management and prepare patients
for future outbreaks and pandemics.
Author contributions
Concept or design: PK Chan, C Wen, LCM Lau, TKC Leung, MH Luk, VWK Chan, A Cheung, MH Cheung, H Fu, KY Chiu.
Acquisition of data: JR Khoo.
Analysis or interpretation of data: JR Khoo.
Drafting of the manuscript: JR Khoo.
Critical revision of the manuscript for important intellectual content: PK Chan, C Wen, LCM Lau, TKC Leung, MH Luk, VWK Chan, A Cheung, MH Cheung, KY Chiu.
Acquisition of data: JR Khoo.
Analysis or interpretation of data: JR Khoo.
Drafting of the manuscript: JR Khoo.
Critical revision of the manuscript for important intellectual content: PK Chan, C Wen, LCM Lau, TKC Leung, MH Luk, VWK Chan, A Cheung, MH Cheung, KY Chiu.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Supplementary material
The supplementary material was provided by the authors and some information may not have been peer reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by the Hong Kong Academy of Medicine and the Hong Kong Medical Association. The Hong Kong Academy of Medicine and the Hong Kong Medical Association disclaim all liability and responsibility arising from any reliance placed on the content.
References
1. Abramoff B, Caldera FE. Osteoarthritis: pathology, diagnosis, and treatment options. Med Clin North Am 2020;104:293-311. Crossref
2. Wong K, Yeung M. Office of the Government Economist,
Hong Kong SAR Government. Population ageing trend of
Hong Kong. January 2019. Available from: https://www.hkeconomy.gov.hk/en/pdf/el/el-2019-02.pdf. Accessed 8 Mar 2022.
3. Bannuru RR, Osani MC, Vaysbrot EE, et al. OARSI
guidelines for the non-surgical management of knee, hip,
and polyarticular osteoarthritis. Osteoarthritis Cartilage
2019;27:1578-89. Crossref
4. Lee LS, Chan PK, Fung WC, et al. Lessons learnt from the
impact of COVID-19 on arthroplasty services in Hong
Kong: how to prepare for the next pandemic? Arthroplasty
2021;3:36. Crossref
5. Hussain SM, Neilly DW, Baliga S, Patil S, Meek RM. Knee
osteoarthritis: a review of management options. Scott Med
J 2016;61:7-16. Crossref
6. Battista S, Dell’Isola A, Manoni M, Englund M, Palese A,
Testa M. Experience of the COVID-19 pandemic as lived
by patients with hip and knee osteoarthritis: an Italian
qualitative study. BMJ Open 2021;11:e053194. Crossref
7. Elderly Health Service, Department of Health, Hong Kong
SAR Government. Elderly Health Service. Available from:
https://www.elderly.gov.hk/eindex.html. Accessed 8 Mar
2022.
8. Centre for Health Protection, Department of Health, Hong
Kong SAR Government. Report of Population Health
Survey 2014/2015. 2017. Available from: https://www.chp.gov.hk/files/pdf/dh_phs_2014_15_full_report_eng.pdf. Accessed 8 Mar 2022.
9. Zheng H, Chen C. Body mass index and risk of knee
osteoarthritis: systematic review and meta-analysis of
prospective studies. BMJ Open 2015;5:e007568. Crossref
10. Chung LM, Law QP, Fong SS, Chung JW, Yuen PP. A cost-effectiveness analysis of teledietetics in short-, intermediate-, and long-term weight reduction. J Telemed Telecare 2015;21:268-75. Crossref
11. Christensen R, Bartels EM, Astrup A, Bliddal H. Effect of
weight reduction in obese patients diagnosed with knee
osteoarthritis: a systematic review and meta-analysis. Ann
Rheum Dis 2007;66:433-9. Crossref
12. Tanaka R, Ozawa J, Kito N, Moriyama H. Efficacy of
strengthening or aerobic exercise on pain relief in people
with knee osteoarthritis: a systematic review and meta-analysis
of randomized controlled trials. Clin Rehabil
2013;27:1059-71. Crossref
13. Jenkinson CM, Doherty M, Avery AJ, et al. Effects of dietary
intervention and quadriceps strengthening exercises on
pain and function in overweight people with knee pain:
randomised controlled trial. BMJ 2009;339:b3170. Crossref
14. Endstrasser F, Braito M, Linser M, Spicher A, Wagner M,
Brunner A. The negative impact of the COVID-19
lockdown on pain and physical function in patients with
end-stage hip or knee osteoarthritis. Knee Surg Sports
Traumatol Arthrosc 2020;28:2435-43. Crossref
15. Jakiela JT, Waugh EJ, White DK. Walk at least 10 minutes
a day for adults with knee osteoarthritis: recommendation
for minimal activity during the COVID-19 pandemic. J
Rheumatol 2021;48:157-9. Crossref
16. Lau MC, Lam JK, Siu E, Fung CS, Li KT, Lam MW. Physiotherapist-designed aquatic exercise programme for community-dwelling elders with osteoarthritis of the knee:
a Hong Kong pilot study. Hong Kong Med J 2014;20:16-23. Crossref
17. Ku BP, Tse AW, Pang BC, et al. Tele-rehabilitation
to combat rehabilitation service disruption during
COVID-19 in Hong Kong: observational study. JMIR
Rehabil Assist Technol 2021;8:e19946. Crossref
18. Fu HC, Lie CW, Ng TP, Chen KW, Tse CY, Wong WH.
Prospective study on the effects of orthotic treatment for
medial knee osteoarthritis in Chinese patients: clinical
outcome and gait analysis. Hong Kong Med J 2015;21:98-106. Crossref
19. Shimoura K, Iijima H, Suzuki Y, Aoyama T. Immediate
effects of transcutaneous electrical nerve stimulation
on pain and physical performance in individuals with
preradiographic knee osteoarthritis: a randomized
controlled trial. Arch Phys Med Rehabil 2019;100:300-6.e1. Crossref
20. Kan HS, Chan PK, Chiu KY, et al. Non-surgical treatment of knee osteoarthritis. Hong Kong Med J 2019;25:127-33. Crossref
21. Cao P, Li Y, Tang Y, Ding C, Hunter DJ. Pharmacotherapy
for knee osteoarthritis: current and emerging therapies.
Expert Opin Pharmacother 2020;21:797-809. Crossref
22. Simental-Mendía M, Sánchez-García A, Vilchez-Cavazos F,
Acosta-Olivo CA, Peña-Martínez VM, Simental-Mendía
LE. Effect of glucosamine and chondroitin sulfate in
symptomatic knee osteoarthritis: a systematic review and
meta-analysis of randomized placebo-controlled trials.
Rheumatol Int 2018;38:1413-28. Crossref
23. da Costa BR, Pereira TV, Saadat P, et al. Effectiveness and
safety of non-steroidal anti-inflammatory drugs and opioid
treatment for knee and hip osteoarthritis: network meta-analysis.
BMJ 2021;375:n2321. Crossref
24. Persson MS, Stocks J, Sarmanova A, et al. Individual
responses to topical ibuprofen gel or capsaicin cream
for painful knee osteoarthritis: a series of n-of-1 trials.
Rheumatology (Oxford) 2021;60:2231-7. Crossref
25. Axe JM, Snyder-Mackler L, Axe MJ. The role of viscosupplementation. Sports Med Arthrosc Rev 2013;21:18-22. Crossref
26. Bellamy N, Campbell J, Robinson V, Gee T, Bourne R, Wells G. Viscosupplementation for the treatment of osteoarthritis of the knee. Cochrane Database Syst Rev 2006;2006:CD005321. Crossref
27. Bansal H, Leon J, Pont JL, et al. Platelet-rich plasma (PRP)
in osteoarthritis (OA) knee: correct dose critical for long
term clinical efficacy. Sci Rep 2021;11:3971. Crossref
28. Yan CH, Chan WL, Yuen WH, et al. Efficacy and safety of
hylan G-F 20 injection in treatment of knee osteoarthritis
in Chinese patients: results of a prospective, multicentre,
longitudinal study. Hong Kong Med J 2015;21:327-32. Crossref
29. Ayhan E, Kesmezacar H, Akgun I. Intraarticular injections
(corticosteroid, hyaluronic acid, platelet rich plasma) for
the knee osteoarthritis. World J Orthop 2014;5:351-61. Crossref
30. Wang-Saegusa A, Cugat R, Ares O, Seijas R, Cuscó X,
Garcia-Balletbó M. Infiltration of plasma rich in growth
factors for osteoarthritis of the knee short-term effects
on function and quality of life. Arch Orthop Trauma Surg
2011;131:311-7. Crossref
31. Kim C, Keating A. Cell therapy for knee osteoarthritis:
mesenchymal stromal cells. Gerontology 2019;65:294-8. Crossref
32. Cianca JC, Jayaram P. Musculoskeletal injuries and regenerative medicine in the elderly patient. Phys Med Rehabil Clin N Am 2017;28:777-94. Crossref
33. Mukarram MS, Ishaq Ghauri M, Sethar S, Afsar N, Riaz A,
Ishaq K. COVID-19: an emerging culprit of inflammatory
arthritis. Case Rep Rheumatol 2021;2021:6610340. Crossref