Hong Kong Med J 2024 Feb;30(1):16–24 | Epub 16 Jan 2024
https://doi.org/10.12809/hkmj2210249
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE CME
COVID-19 vaccination and transmission patterns among pregnant and postnatal women during the fifth wave of COVID-19 in a tertiary hospital in Hong Kong
PW Hui, MD, FRCOG; LM Yeung, BNur, MPH; Jennifer KY Ko, MB, BS, MRCOG; Theodora HT Lai, MB, BS, MRCOG; Diana MK Chan, MB, BS, MRCOG; Dorothy TY Chan, MB, BS; Sophia YK Mok, MB, BS, MRCOG; Kitty KW Ma, MB, BS; Pamela SY Kwok, BNur, MSM, Polly WC Pang, BN; Mimi TY Seto, MB, BS, MRCOG
Department of Obstetrics and Gynaecology, Queen Mary Hospital, Hong Kong SAR, China
Corresponding author: Dr PW Hui (apwhui@hku.hk)
Abstract
Introduction: Vaccination is a key strategy to
control the coronavirus disease 2019 (COVID-19)
pandemic. Safety concerns strongly influence
vaccine hesitancy. Disease transmission during
pregnancy could exacerbate risks of preterm birth
and perinatal mortality. This study examined
patterns of vaccination and transmission among
pregnant and postnatal women during the fifth wave
of COVID-19 in Hong Kong.
Methods: The Antenatal Record System and Clinical
Management System of the Hospital Authority
was used to retrieve information concerning the
demographic characteristics, vaccination history,
COVID-19 status, and obstetric outcomes of
women who were booked for delivery at Queen
Mary Hospital in Hong Kong and had attended the
booking antenatal visit from 1 July 2021 to 30 June
2022.
Results: Among 2396 women in the cohort, 2006
(83.7%), 1843 (76.9%), and 831 (34.7%) had received
the first, second, and third doses of COVID-19
vaccine, respectively. Among 1012 women who
had received the second dose, 684 (67.6%) women
were overdue for their third dose. There were 265
(11.1%) reported COVID-19 cases. Women aged 20
to 29 years had a low vaccination rate but the highest disease rate (19.1%). The disease rate was more
than tenfold higher in women who had no (20.3%)
or incomplete (18.8%) vaccination, compared
with women who had complete vaccination (2.1%;
P<0.001).
Conclusion: Acceptance of COVID-19 vaccination
was low in pregnant women. Urgent measures are
needed to promote vaccination among pregnant
women before the next wave of COVID-19.
New knowledge added by this study
- As of 30 June 2022, only 34.7% of women in Hong Kong had received three doses of coronavirus disease 2019 (COVID-19) vaccine.
- Two-thirds women scheduled for a third dose of COVID-19 vaccine did not receive the booster dose during pregnancy.
- The disease rate was almost ten times higher in women who had no or incomplete vaccination, compared with women who had complete vaccination.
- Women aged 20 to 29 years had a low vaccination rate but the highest disease rate.
- Pregnant women should receive education concerning the importance and safety of COVID-19 vaccination during pregnancy and breastfeeding.
- Delayed receipt of booster doses increase susceptibility to COVID-19 during future waves.
- A comprehensive programme incorporating pertussis and COVID-19 vaccination for pregnant women should be considered.
Introduction
Vaccination is an effective tool to combat the
coronavirus disease 2019 (COVID-19) pandemic.
Two types of COVID-19 vaccines are used in Hong
Kong: the Sinovac-CoronaVac inactivated severe
acute respiratory syndrome coronavirus 2 vaccine
(Sinovac Biotech Ltd, Beijing, China) and Pfizer
BioNTech BNT162b2 (Pfizer Inc, Philadelphia
[PA], United States) messenger RNA vaccine began
distribution on 26 February 2021 and 10 March
2021, respectively.
According to the World Health Organization,
vaccine hesitancy is defined as delaying or refusing
vaccination despite the availability of vaccination
services.1 In a study conducted during the third wave
of COVID-19 in Hong Kong, the overall vaccine
acceptance rate was approximately 37%.2 Although
the subsequent acceptance rate has varied with
pandemic progression, confidence in COVID-19
vaccines has remained a key factor in reducing
vaccine hesitancy.3
Pregnant women were generally excluded
from clinical trials focusing on the development,
safety, and efficacy of COVID-19 vaccines.4 When
COVID-19 vaccines were introduced in Hong
Kong, routine vaccination was not recommended
for women who were pregnant or breastfeeding,
except when there was a high risk of exposure or
complications.5 The relative lack of data may have
contributed to vaccine hesitancy among pregnant women.6 7 8 Based on data concerning the efficacy and
safety of COVID-19 vaccination in preventing serious
illness,9 COVID-19 vaccination is recommended for
people who are pregnant, breastfeeding, planning to
become pregnant, or may become pregnant in the
future.10 11
On 23 April 2021, the Hong Kong College of
Obstetricians and Gynaecologists (HKCOG) issued
an interim recommendation that pregnant women
receive the BioNTech COVID-19 vaccine at the same
time as the general population.12 On 18 February
2022, the Sinovac vaccine was also recommended
for use in pregnant women.12 Furthermore, the
recommended interval between the second and third
doses of COVID-19 vaccine was shortened from 180
days to 90 days, beginning on 4 March 2022. The
vaccine pass policy for entry to specific premises was
tightened on 31 May 2022.13 For persons who were
over 18 years old and had no history of infection, a
minimal of two doses of vaccination was required.
A third dose was required if the second dose was
taken over 6 months ago. Starting from 13 June 2022,
women attending obstetric clinics were required to
provide a negative result proof of a polymerase chain
reaction–based nucleic acid test conducted with
specimen collected within 48 hours before the visit
if they did not fulfil the vaccine pass requirement.14
The fifth wave of COVID-19 in Hong Kong has
resulted in an overwhelming number of COVID-19
cases. Pregnant women are not automatically
protected from COVID-19; indeed, their vaccine
hesitancy and low vaccination rate may lead to
greater susceptibility. Information concerning the
patterns of COVID-19 vaccination and disease
transmission among pregnant women in Hong
Kong is unavailable. This study examined patterns
of vaccination and transmission among pregnant
women who were booked for delivery at a tertiary
hospital in Hong Kong, with the goal of providing
insights into maternal disease characteristics.
Methods
This retrospective review included women who were
booked for delivery at Queen Mary Hospital in Hong
Kong and had attended the booking antenatal visit
from 1 July 2021 to 31 March 2022. Information
concerning COVID-19 vaccination history was
retrieved from the Clinical Management System of
the Hospital Authority, which captured COVID-19
vaccination data from the Department of Health.
Pregnant women were diagnosed with
COVID-19 because of symptoms or (in the absence
of symptoms) during admission screening. Women
diagnosed with COVID-19 through other channels
were able to reschedule their appointments. Phone
consultations were provided by the obstetric team
at Queen Mary Hospital. The clinical details of
COVID-19 cases were documented in the computerised Antenatal Record System.
Additionally, antenatal progress notes were updated
if a pregnant woman reported a history of COVID-19
during a follow-up visit. Data regarding demographic
characteristics, COVID-19 status, and obstetric
outcomes were retrieved from the Antenatal Record
System.
The vaccinated group comprised women who
received at least one dose of any type of COVID-19
vaccine. Vaccination periods were classified as pre-pregnancy,
antenatal, and postnatal for women with
a known date of delivery, miscarriage, or termination
of pregnancy as of 30 June 2022. For women with
ongoing pregnancies and unknown obstetric
outcomes, the vaccination period was estimated
according to the expected date of delivery. Antenatal
status was regarded as known ongoing pregnancy
before 42 weeks of gestation. A vaccination
episode was defined as any episode of COVID-19
vaccination including the first, second, and third
doses. The number of days elapsed since vaccination
was defined as the interval between the last dose of
COVID-19 vaccine and 30 June 2022 for women who
had received one or two doses of vaccine. Complete
vaccination was regarded as the period between
15 and 90 days after the second dose of COVID-19
vaccine, or 14 days after the third dose of COVID-19
vaccine for women who had never been diagnosed
with COVID-19. For women with COVID-19, the
date of diagnosis was regarded as the reference point
when determining vaccination status.
Descriptive statistics were reported.
Vaccination rates were calculated according to age-group.
Background demographic characteristics were
compared between vaccinated and unvaccinated
groups. Student’s t test, analysis of variance, and the
Chi squared test were used as appropriate. Regression
analyses were conducted to identify factors affecting
vaccine acceptance. P values <0.05 were considered
statistically significant. Statistical analyses were
performed using SPSS software (Windows version
26; IBM Corp, Armonk [NY], United States).
Results
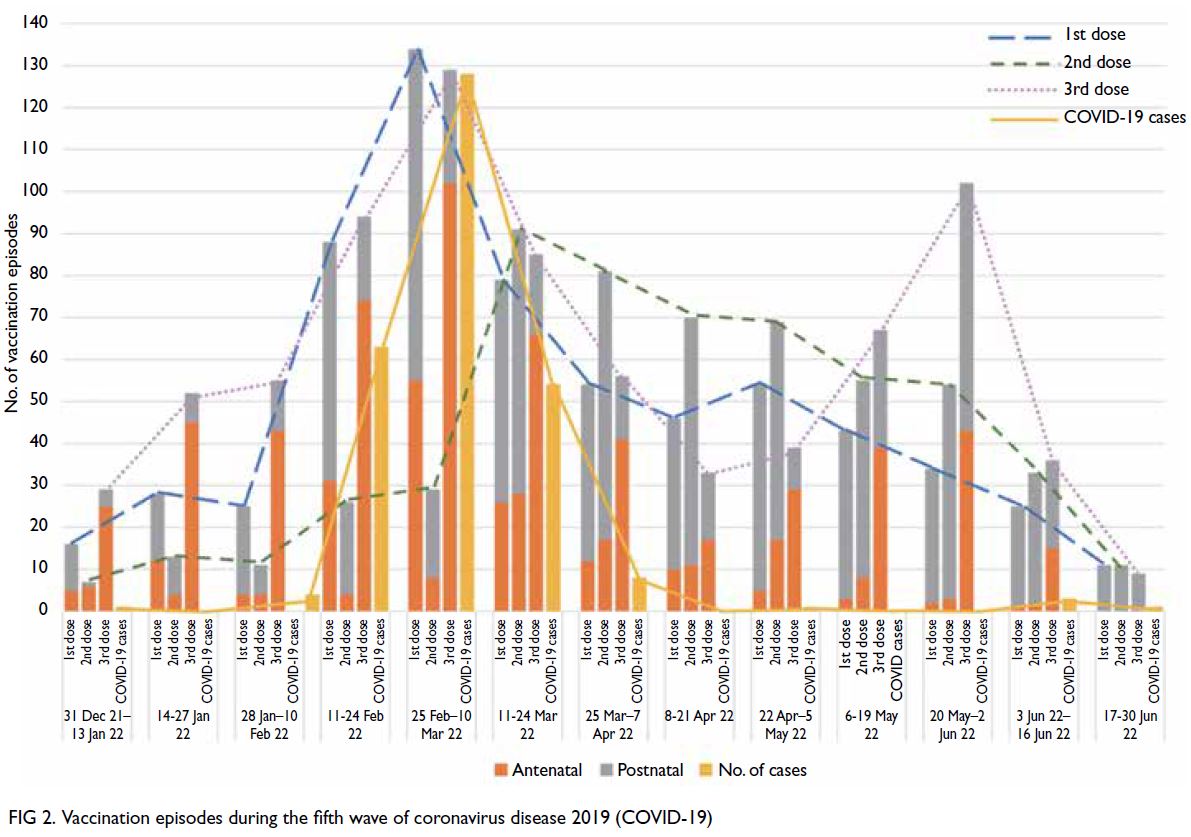
Table 1 shows the demographic characteristics of
2396 pregnant women who had attended the booking
antenatal visit between 1 July 2021 and 31 March 2022.
As of 30 June 2022, 2006 (83.7%), 1843 (76.9%), and
831 (34.7%) women had received the first, second,
and third doses of COVID-19 vaccine, respectively.
Among the 1843 women who had received two doses
of vaccine, 1056 (57.3%) underwent vaccination
before pregnancy (Fig 1). Of these 1843 women, 831
received a third dose; the median interval between
the second and third doses was 280 days (interquartile
range, 239-308). Of the remaining 1012 women who
had received only two doses of vaccine, 684 (67.6%)
and 504 (49.8%) had already passed the 90-day and 180-day intervals, respectively. Their median
number of days elapsed since the last vaccine was 315
(interquartile range, 145-368), which considerably
exceeded the recommended 90-day interval.
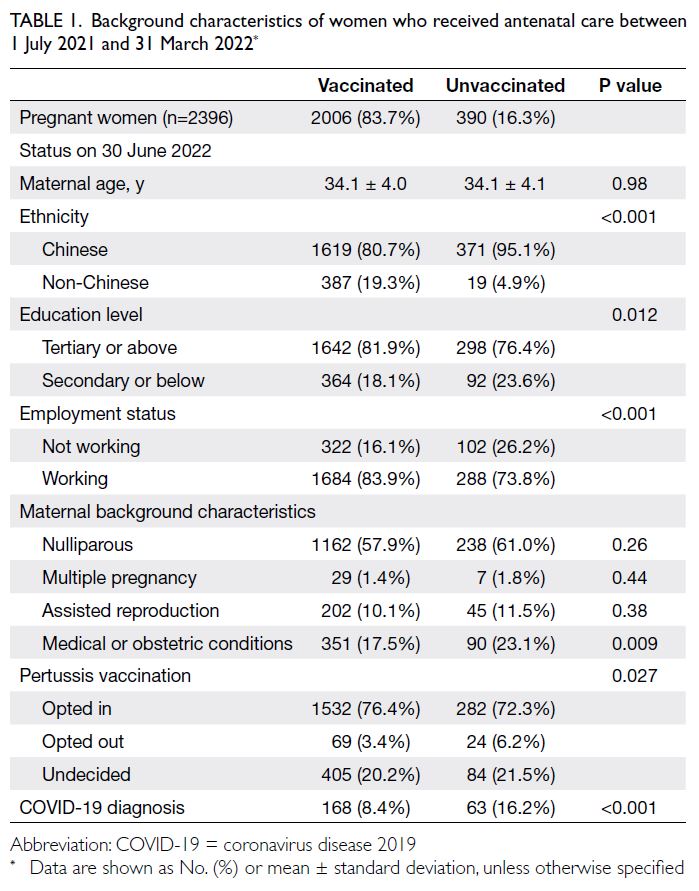
Table 1. Background characteristics of women who received antenatal care between 1 July 2021 and 31 March 2022
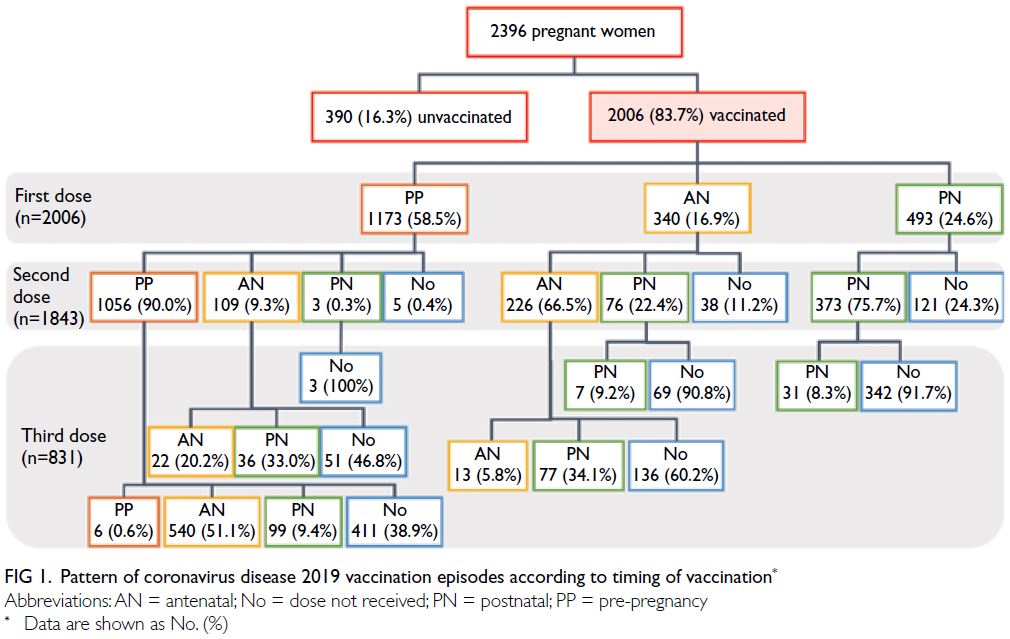
Figure 1. Pattern of coronavirus disease 2019 vaccination episodes according to timing of vaccination
Only 26.6% (1243/4680) of vaccination episodes
occurred during pregnancy. Among women who
underwent antenatal vaccination, 65.7% (817/1243)
had it during the fifth wave of COVID-19 between
January 2022 and June 2022; 65.7% (537/817) of
these women received the third dose. The two peaks
of vaccination for third dose were observed in early
March 2022 and late May 2022 (Fig 2).
The vaccination rate was the lowest among
Chinese women (81.4%), but the highest among
Caucasian women (96.4%) [Fig 3]. Multivariate
analysis showed that active working status (odds
ratio [OR]=1.94; 95% confidence interval [CI]=1.47-2.56) was significantly associated with a higher
COVID-19 vaccination rate, whereas Chinese
ethnicity (OR=0.21; 95% CI=0.13-0.33) and
women with obstetric complications (OR=0.72;
95% CI=0.55-0.94) were significantly associated with
a lower COVID-19 vaccination rate.
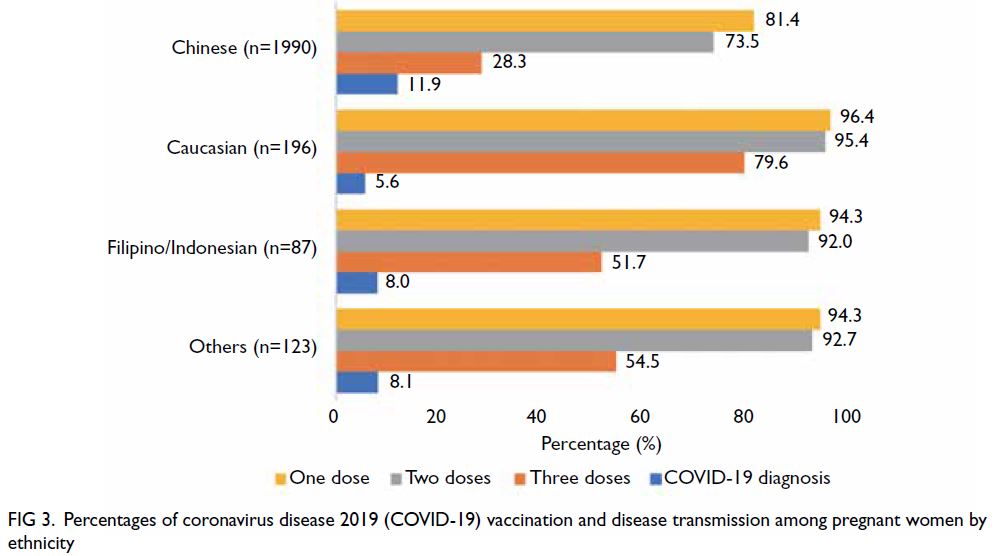
Figure 3. Percentages of coronavirus disease 2019 (COVID-19) vaccination and disease transmission among pregnant women by ethnicity
In total, there were 265 (11.1%) COVID-19
cases in this cohort; the earliest diagnosis was made
on 1 January 2022 during the fifth wave of COVID-19
in Hong Kong (Table 2). The disease rate was more
than tenfold higher in women who had no (20.3%)
or incomplete (18.8%) vaccination, compared
with women who had complete vaccination (2.1%;
P<0.001). After exclusion of pregnancies among
women aged ≤19 years, there was an insignificant
trend of lower vaccination among young women
(ie, aged 20-29 years), but their disease rate was the
highest (19.1%) [Fig 4].
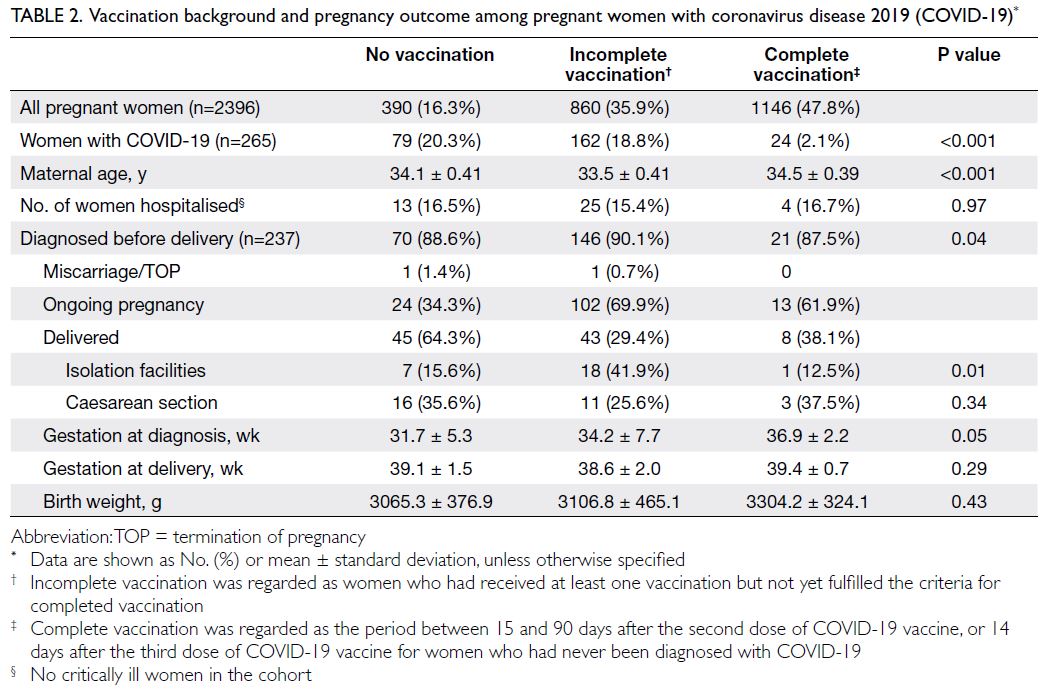
Table 2. Vaccination background and pregnancy outcome among pregnant women with coronavirus disease 2019 (COVID-19)
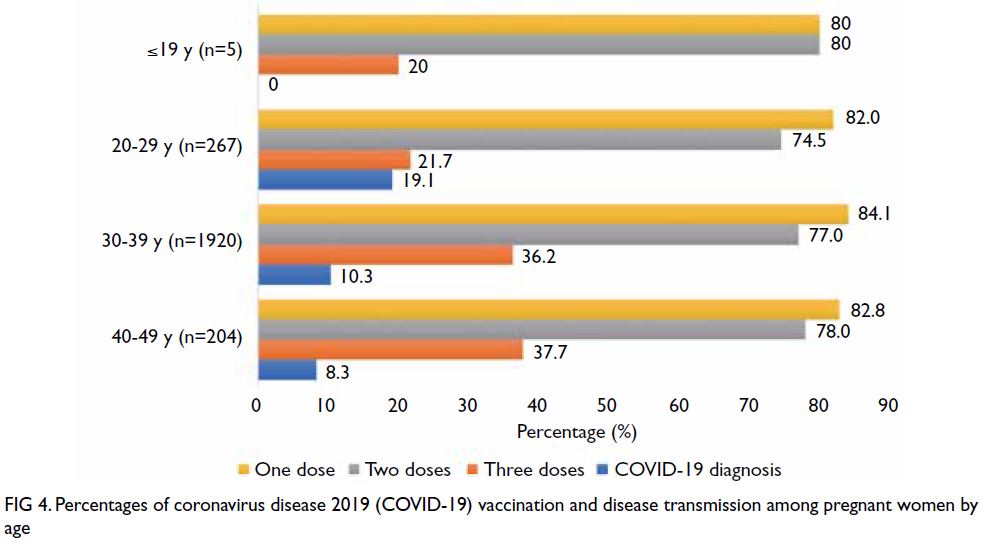
Figure 4. Percentages of coronavirus disease 2019 (COVID-19) vaccination and disease transmission among pregnant women by age
Among 237 (89.4%) women who had an
antenatal diagnosis of COVID-19, 42 (17.7%)
required admission for monitoring and 26 (11.0%)
delivered in an isolation facility. No women required
intensive care or oxygen support. There were no
adverse maternal outcomes or cases of vertical
transmission.
Discussion
Coronavirus disease 2019 vaccination
To our knowledge, this is the first report of the low
COVID-19 vaccination rate (83.7%) among pregnant
women in Hong Kong. This rate is considerably lower
than the single-dose rate among the general public
(92.7%) that was reported on the government’s
vaccination dashboard on the final day of the study
period (ie, 30 June 2022).15 Furthermore, the disease
rate was more than threefold higher in women who had no or incomplete vaccination, compared with
women who had complete vaccination.
Pregnant women are considered a vulnerable
group. The substantial increase in the disease
rate, combined with a lower vaccination rate,
among women aged 20 to 29 years is particularly
concerning. A case of COVID-19 during pregnancy
can lead to adverse obstetric outcomes, including
increased risks of preterm delivery, growth
restriction, and stillbirth.16 In addition to the effectiveness of vaccination in terms of reducing
severe complications, the transplacental transfer
of immunoglobulins after maternal vaccination
might provide infants with protection against
COVID-19.10 16 17 18
Vaccine hesitancy
Vaccine hesitancy is a potential public health
problem.19 The five psychological antecedents of
vaccination are confidence, complacency, constraints,
calculation, and collective responsibility.20 21
Acceptance of COVID-19 vaccination has varied
among countries, with the highest rates reported
in India, the Philippines, and Latin America.22 In
the present study, Chinese women had a lower
vaccination rate, compared with their non-Chinese
counterparts.
The COVID-19 pandemic has contributed to
a decrease in vaccine hesitancy.23 In May 2021, a
systemic review showed that an estimated 47% of
pregnant women worldwide intended to undergo
COVID-19 vaccination.24
Communities generally become more
complacent when the number of disease cases is
low, suggesting that the perceived risk of disease
transmission is minimal. This phenomenon was
evident in Hong Kong across several waves of
COVID-19 transmission.15 The vaccination rate
increased during the fifth wave of COVID-19 when
there was an exponential surge in the number of
disease cases. A similar pattern was observed in the
present study, such that two-thirds of the antenatal
vaccination episodes occurred during the fifth wave
of COVID-19 in Hong Kong.
Despite this relative surge in vaccination,
around two-thirds of women eligible for the third
dose did not receive it during pregnancy. This delay
poses a major threat because the protective effect of the previous two doses may have dissipated.
Importantly, although the rate of vaccination was
higher in the antenatal group than the postnatal
group, most women in the antenatal group had
undergone vaccination before pregnancy. Thus, they
may have a higher risk of serious adverse effects
from COVID-19 if they become ill in the peripartum
period. After exclusion of the small number of
pregnant women aged ≤19 years, vaccination rates
were consistently low among pregnant women of
all ages. Pregnant women may have a higher risk of
disease transmission in future waves of COVID-19;
at the end of the present study, only one-third of
pregnant women in this cohort had received three
doses of vaccine.
Lack of confidence has been identified as
the main factor consistently associated with lower
COVID-19 vaccine hesitancy.3 The implementation
of the stringent vaccine pass policy had driven
another peak of vaccination in late May 2022.
However, nearly half of the women who had received
two doses of vaccine were indeed overdue for the
third dose, and hence did not fulfil the vaccine
pass for entrance to specific premises or could not
attend obstetric clinics without undergoing nucleic
acid testing. This group of vaccine had received
COVID-19 vaccine before but had it mostly before
pregnancy. Pregnancy could represent the key
hindrance for their vaccination in the antenatal
period. Government policy might not be adequate
enough for promoting vaccination in pregnant
women. Concern about possible harmful side-effects
was the top reason for reluctance; confidence in
COVID-19 vaccine safety and efficacy was the main
predictor of acceptance, particularly in the pregnant
population.8 22 In a Japanese cohort, concerns about
potential effects on the fetus and breastfeeding were
the main reasons for low COVID-19 vaccination
acceptance.25 These findings highlight the need to
distribute correct information and provide sufficient
education to address concerns among women of
reproductive age. In particular, antenatal women
should receive additional information concerning
vaccine safety during pregnancy.
Vaccination promotion
A study in Hong Kong showed that recommendations
from the government constituted the strongest
factor driving COVID-19 vaccine acceptance.2
Education about the safety and benefit of vaccination
is also important.7 Webinars would be useful in
efforts to educate the general public. Within the
hospital setting, vaccination teams comprising
obstetricians and midwives could allay concerns
and dispel myths about vaccination among working
staff at all levels; this approach could provide useful
information for pregnant and breastfeeding women.
There is also a need to combat physician hesitancy in recommending COVID-19 vaccination for pregnant
women.26 To address this need, the HKCOG revised
its recommendations on 3 March 2022 to indicate
that women who are planning to become pregnant,
are pregnant, or are breastfeeding should undergo
COVID-19 vaccination along with the general
population.12 A corresponding educational video to
promote COVID-19 vaccination was made available
on 5 March 2022.12
Possible interventions to promote vaccination
in Hong Kong include the provision of vaccines at
convenient venues and the involvement of healthcare
professionals in information dissemination.27 During
the fifth wave of COVID-19, pregnant women
were proactively asked to consider COVID-19
vaccination when they attended obstetric clinics.
Leaflets were distributed with information about the
HKCOG recommendations, as well as community
vaccination sites. The establishment of a pathway
specifically for pregnant women, which reduced
their waiting time in vaccine clinics, also helped to
increase the vaccination rate. Moreover, vaccination
was provided to women in the maternity wards of
some hospitals and women attending antenatal
clinics in Maternal and Child Health Centres. All of
these measures helped reduce vaccine hesitancy in
pregnant women.28
In Hong Kong, a pertussis vaccination
programme for pregnant women was launched on
2 July 2020.29 The programme was incorporated
into antenatal care, such that all pregnant women
received counselling concerning the rationale for
vaccination; the vaccine was administered during
obstetric follow-up. To facilitate vaccine availability
in our hospital, all women were asked to indicate
their preference concerning pertussis vaccination
during the first antenatal visit. It may be useful
to incorporate COVID-19 vaccination into the
maternal immunisation programme.
Strengths
This study had some notable strengths. The results
of the present large cohort study provide clinicians
and policymakers with key insights concerning the
COVID-19 vaccination rate among pregnant women
in Hong Kong. The study period was designed to
include both antenatal and postnatal periods for
a better understanding of vaccination behaviour
among women in each period. A real-time collection
method was adopted to capture COVID-19
vaccination records from the Clinical Management
System, thereby ensuring data reliability.
Limitations
Nevertheless, this study had some limitations. A small number of women who underwent COVID-19
vaccination outside Hong Kong were not automatically identified in the system; however, they were included
in the cohort if their vaccination history had been
documented in antenatal records. Because rapid
antigen self-tests were acceptable for diagnosis in
Hong Kong beginning on 26 February 2022, the
number of recorded COVID-19 cases in our cohort
might have been lower than the actual number of
cases if patients did not report positive COVID-19
test results to our department. Finally, this study did
not explore whether the generally more cautious
approach of pregnant women, in terms of avoiding
all types of diseases, might contribute to a lower
disease rate compared with the general public.
Conclusion
The rate of COVID-19 vaccination was low among
pregnant and postnatal women in Hong Kong in
early 2022. Pregnant women had a high risk of
disease transmission because many of them had not
received the third dose of COVID-19 vaccine. Urgent
measures are needed to promote vaccination among
pregnant women before future waves of COVID-19.
In particular, women should receive information
concerning vaccine safety to avoid unnecessary
delays related to pregnancy.
Author contributions
Concept or design: PW Hui, DTY Chan.
Acquisition of data: All authors.
Analysis or interpretation of data: PW Hui.
Drafting of the manuscript: PW Hui, LM Yeung, JKY Ko, THT Lai, MTY Seto.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: PW Hui.
Drafting of the manuscript: PW Hui, LM Yeung, JKY Ko, THT Lai, MTY Seto.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
The authors thank Dr TW Chay, Dr YF Chiu, Ms WK Choi, Dr TY Hui, Dr KH Lam, Dr KS Lee, Dr YH Luk, Dr SK Ma,
Dr HS Wang, Dr CCY Wong, Dr CL Wong, Dr LC Wong, and Dr CWK Yan of Department of Obstetrics and Gynaecology, Queen Mary Hospital for their contributions to research data retrieval and entry.
Declaration
The abstract has been presented online in the Royal College of Obstetricians and Gynaecologists World Congress 2023 (14 June 2013, London, United Kingdom).
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
Ethics approval was obtained from the Institutional Review
Board of The University of Hong Kong/Hospital Authority
Hong Kong West Cluster (Ref No.: UW 22-205). Informed
patient consent has been waived by the Board due to the
retrospective nature of the research.
References
1. MacDonald NE; SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine 2015;33:4161-4. Crossref
2. Wong MC, Wong EL, Huang J, et al. Acceptance of the COVID-19 vaccine based on the health belief model: a population-based survey in Hong Kong. Vaccine 2021;39:1148-56. Crossref
3. Xiao J, Cheung JK, Wu P, Ni MY, Cowling BJ, Liao Q. Temporal changes in factors associated with COVID-19 vaccine hesitancy and uptake among adults in Hong Kong: serial cross-sectional surveys. Lancet Reg Health West Pac 2022;23:100441. Crossref
4. Beigi RH, Krubiner C, Jamieson DJ, et al. The need for inclusion of pregnant women in COVID-19 vaccine trials. Vaccine 2021;39:868-70. Crossref
5. Scientific Committee on Emerging and Zoonotic Disease
and Scientific Committee on Vaccine Preventable
Diseases, Centre for Health Protection, Hong Kong SAR
Government. Consensus interim recommendations on
the use of COVID-19 vaccines in Hong Kong (as of Jan 7,
2021). Available from: https://www.chp.gov.hk/files/pdf/consensus_interim_recommendations_on_the_use_of_covid19_vaccines_inhk.pdf . Accessed 30 Mar 2022.
6. Tao L, Wang R, Han N, et al. Acceptance of a COVID-19
vaccine and associated factors among pregnant women in
China: a multi-center cross-sectional study based on health
belief model. Hum Vaccin Immunother 2021;17:2378-88. Crossref
7. Sznajder KK, Kjerulff KH, Wang M, Hwang W, Ramirez SI,
Gandhi CK. COVID-19 vaccine acceptance and associated
factors among pregnant women in Pennsylvania 2020. Prev
Med Rep 2022;26:101713. Crossref
8. Sutton D, D’Alton M, Zhang Y, et al. COVID-19 vaccine
acceptance among pregnant, breastfeeding, and
nonpregnant reproductive-aged women. Am J Obstet
Gynecol MFM 2021;3:100403. Crossref
9. Shimabukuro TT, Kim SY, Myers TR, et al. Preliminary
findings of mRNA COVID-19 vaccine safety in pregnant
persons. N Engl J Med 2021;384:2273-82. Crossref
10. Halasa NB, Olson SM, Staat MA, et al. Effectiveness of
maternal vaccination with mRNA COVID-19 vaccine
during pregnancy against COVID-19–associated
hospitalization in infants aged <6 months—17 states, July
2021–January 2022. MMWR Morb Mortal Wkly Rep
2022;71:264-70. Crossref
11. Girardi G, Bremer AA. Scientific evidence supporting coronavirus disease 2019 (COVID-19) vaccine efficacy and safety in people planning to conceive or who are pregnant or lactating. Obstet Gynecol 2022;139:3-8. Crossref
12. The Hong Kong College of Obstetricians and
Gynaecologists. The Hong Kong College of
Obstetricians and Gynaecologists advice on COVID-19
vaccination in pregnant and lactating women (interim;
updated on 3rd March 2022). 2022. Available from:
http://www.hkcog.org.hk/hkcog/Upload/EditorImage/20220304/20220304134806_9035.pdf. Accessed 30 Mar 2022.
13. Hong Kong SAR Government. FEHD reminds catering
premises operators and customers to observe requirements
on third stage of Vaccine Pass. 2022. Available from:
https://www.info.gov.hk/gia/general/202205/30/P2022053000726.htm?fontSize=1. Accessed 30 May 2022.
14. Hong Kong SAR Government. Government to implement
Vaccine Pass arrangement in designated healthcare
premises. 2022. Available from: https://www.info.gov.hk/gia/general/202205/21/P2022052100421.htm. Accessed 21 May 2022.
15. Together, We Fight the Virus. The Government of the
Hong Kong Special Administrative Region. Available
from: https://www.coronavirus.gov.hk/eng/index.html. Accessed 30 Jun 2022.
16. Allotey J, Stallings E, Bonet M, et al. Clinical manifestations,
risk factors, and maternal and perinatal outcomes of
coronavirus disease 2019 in pregnancy: living systematic
review and meta-analysis. BMJ 2020;370:m3320. Crossref
17. Male V. SARS-CoV-2 infection and COVID-19 vaccination in pregnancy. Nat Rev Immunol 2022;22:277-82. Crossref
18. Nir O, Schwartz A, Toussia-Cohen S, et al. Maternal-neonatal
transfer of SARS-CoV-2 immunoglobulin
G antibodies among parturient women treated with
BNT162b2 messenger RNA vaccine during pregnancy. Am
J Obstet Gynecol MFM 2022;4:100492. Crossref
19. Shook LL, Kishkovich TP, Edlow AG. Countering COVID-19 vaccine hesitancy in pregnancy: the “4 Cs”. Am J Perinatol 2022;39:1048-54. Crossref
20. Betsch C, Schmid P, Heinemeier D, Korn L, Holtmann C,
Böhm R. Beyond confidence: development of a measure
assessing the 5C psychological antecedents of vaccination.
PLoS One 2018;13:e0208601. Crossref
21. Chau CY. COVID-19 vaccination hesitancy and challenges
to mass vaccination. Hong Kong Med J 2021;27:377-9. Crossref
22. Skjefte M, Ngirbabul M, Akeju O, et al. COVID-19 vaccine
acceptance among pregnant women and mothers of young
children: results of a survey in 16 countries. Eur J Epidemiol
2021;36:197-211. Crossref
23. Gencer H, Özkan S, Vardar O, Serçekuş P. The effects of
the COVID-19 pandemic on vaccine decisions in pregnant
women. Women Birth 2022;35:317-23. Crossref
24. Shamshirsaz AA, Hessami K, Morain S, et al. Intention to
receive COVID-19 vaccine during pregnancy: a systematic
review and meta-analysis. Am J Perinatol 2022;39:492-500. Crossref
25. Hosokawa Y, Okawa S, Hori A, et al. The prevalence of
COVID-19 vaccination and vaccine hesitancy in pregnant
women: an internet-based cross-sectional study in Japan. J
Epidemiol 2022;32:188-94. Crossref
26. Chervenak FA, McCullough LB, Grünebaum A. Reversing
physician hesitancy to recommend COVID-19 vaccination
for pregnant patients. Am J Obstet Gynecol 2022;226:805-12. Crossref
27. Wang K, Wong EL, Cheung AW, et al. Influence of vaccination
characteristics on COVID-19 vaccine acceptance among
working-age people in Hong Kong, China: a discrete choice
experiment. Front Public Health 2021;9:793533. Crossref
28. Iacobucci G. COVID-19 and pregnancy: vaccine hesitancy
and how to overcome it. BMJ 2021;375:n2862. Crossref
29. Hospital Authority. Public hospital pertussis vaccination
programme for pregnant women. Jun 28, 2020. Available
from: https://www.ha.org.hk/haho/ho/cc/pertussis_press_release_en.pdf. Accessed 29 Jun 2023.