Hong Kong Med J 2023 Dec;29(6):498–505 | Epub 20 Nov 2023
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Cross-sectional study to assess the psychological
morbidity of women facing possible miscarriage
Patricia NP Ip, FHKCOG, FHKAM (Obstetrics & Gynaecology); Karen Ng, FHKCOG, FHKAM (Obstetrics & Gynaecology); Osanna YK Wan, FHKCOG, FHKAM (Obstetrics & Gynaecology); Janice WK Kwok, BSc; Jacqueline PW Chung, FHKCOG, FHKAM (Obstetrics & Gynaecology); Symphorosa SC Chan, MD, FHKCOG
Department of Obstetrics and Gynaecology, The Chinese University of Hong Kong, Hong Kong SAR, China
Corresponding author: Dr Patricia NP Ip (patricia.ip@cuhk.edu.hk)
Abstract
Introduction: Threatened miscarriage is a common
complication of pregnancy. This study aimed to
assess psychological morbidity in women with
threatened miscarriage, with the goal of identifying
early interventions for women at risk of anxiety or
depression.
Methods: Women in their first trimester attending
an Early Pregnancy Assessment Clinic were recruited
between July 2013 and June 2015. They were asked to
complete the 12-item General Health Questionnaire
(GHQ-12), the Beck Depression Inventory (BDI),
Spielberger’s State Anxiety Inventory State form
(STAI-S), the Fatigue Scale–14 (FS-14), and the
Profile of Mood States (POMS) before consultation.
They were also asked to rate anxiety levels before and
after consultation using a visual analogue scale (VAS).
Results: In total, 1390 women completed the study.
The mean ± standard deviation of GHQ-12 (bi-modal)
and GHQ-12 (Likert) scores were 4.04 ±
3.17 and 15.19 ± 5.30, respectively. Among these
women, 48.4% had a GHQ-12 (bi-modal) score
≥4 and 76.7% had a GHQ-12 (Likert) score >12,
indicating distress. The mean ± standard deviation
of BDI, STAI-S, and FS-14 scores were 9.35 ± 7.19,
53.81 ± 10.95, and 2.40 ± 0.51, respectively. The
VAS score significantly decreased after consultation (P<0.001). Compared with women without a history
of miscarriage, women with a previous miscarriage
had higher GHQ-12, BDI, and POMS scores (except
for fatigue-inertia and vigour-activity subscales).
A higher bleeding score was strongly positively
correlated with GHQ-12 (Likert) score. There were
weak correlations between pain score and the
GHQ-12 (bi-modal) ≥4, BDI >12, and POMS scores
(except for confusion-bewilderment subscale which
showed a strong positive correlation).
Conclusion: Women with threatened miscarriage
experience a considerable psychological burden,
emphasising the importance of early recognition for
timely management.
New knowledge added by this study
- A substantial proportion of women with threatened miscarriage had symptoms of anxiety or depression.
- Women with a previous miscarriage had a higher level of distress and would benefit from additional attention and psychological support.
- Women with problems in early pregnancy should receive both clinical and psychological care to alleviate their anxiety.
- Further studies of maternal psychological outcomes and fetal outcomes are needed to determine the long-term effects of anxiety and depression among women with threatened miscarriage in the first trimester.
Introduction
Miscarriage occurs in 10% to 15% of pregnancies,
mainly in the first trimester.1 Spontaneous
miscarriage is associated with psychological
problems such as anxiety and depression.2 3 4 Post-traumatic
stress disorder may also occur after
a miscarriage.3 Threatened miscarriage affects
15% to 20% of pregnant women.5 Management of
threatened miscarriage involves reassurance and
counselling. Women with threatened miscarriage and/or pregnancy-related uncertainty may
experience frustration and anxiety. Although there
are extensive data regarding the association between
miscarriage and psychological morbidity, higher
incidences of anxiety and depression among women
with threatened miscarriage have only been detected
in small studies.6 7
Antenatal depression and anxiety disorders are
associated with increased fetal risks, such as low birth
weight; antenatal symptoms of depression have been positively associated with postnatal depression.8 9
Furthermore, antenatal maternal stress and anxiety
appear to predict long-term behavioural and
emotional problems in children.10 11 Therefore, early
detection and intervention are needed in women
with antenatal psychological symptoms to minimise
the impacts of those symptoms.
This study assessed psychological morbidity in
women with threatened miscarriage, with the goal of
identifying early interventions for women at risk of
anxiety or depression.
Methods
Study design
This cross-sectional study, conducted at a university
hospital in Hong Kong between July 2013 and
June 2015, was part of a study that examined the
ability of an early pregnancy viability scoring
system to support counselling for women.12 In this
hospital, an outpatient Early Pregnancy Assessment
Clinic (EPAC) provides medical care for women
experiencing abdominal pain, vaginal bleeding,
or other problems in early pregnancy (gestational
age ≤12 weeks). Referrals are usually made by
medical officers from the Accident and Emergency
Departments across Hong Kong, as well as general
practitioners. All gynaecologists at the EPAC have ≥3
years of experience performing ultrasound scans. All Chinese women attending the EPAC were invited to
participate; written informed consent was obtained
from women who agreed to take part in the study.
Exclusion criteria were age <18 years, ectopic
pregnancy, multiple pregnancies, gestational age
>84 days (>12 weeks), requested termination of
pregnancy, and loss to follow-up. Demographic
data, obstetric history, smoking status, alcohol
consumption, and body mass index were recorded.
Details of early pregnancy complaints were assessed,
including abdominal pain (graded by a pain score of
0 to 3, where a higher score represents greater pain)
and vaginal bleeding (determined by a pictorial
blood loss chart according to the number of pads
used, where 0 corresponds to no bleeding and 4
corresponds to clots or flooding).
Psychometric instruments
Chinese validated versions of five questionnaires
were used to assess psychological well-being among
the participants: the 12-item General Health
Questionnaire (GHQ-12), the Beck Depression
Inventory (BDI), Spielberger’s State Anxiety
Inventory State form (STAI-S), the Fatigue Scale–14
(FS-14), and the Profile of Mood States (POMS).
All questionnaires have demonstrated reliability
and validity in previous studies.13 14 15 The GHQ-12
and BDI scores were reported as both continuous
and categorical variables, while the scores of
other questionnaires were reported as continuous
variables.
The GHQ-12 is a self-reporting rating scale
intended to identify individuals with reduced
psychological well-being or diminished quality of
life. It is sensitive to short-term psychiatric disorders.
A total score of ≥4 using the bi-modal scoring
method (0-0-1-1) is considered ‘high distress’. When
using the Likert scoring method (0-1-2-3), scores
≤12 are considered normal, while scores >12 are
considered evidence of psychological distress.16 17
The questionnaire has been used as a tool to evaluate
women with miscarriage.18 19 20
The BDI is a 21-item self-reporting rating
scale intended to measure symptoms of depression
in both general and psychiatric populations.21
It is used to measure depression severity, and
psychological morbidity is defined as a score of >12,
indicating probable depressive disorder. The STAI-S
is a 20-item self-reporting inventory that measures
state anxiety, including transitory and situational
feelings of worry.22 Its use has been validated in
pregnant women.23 A higher score indicates a higher
level of anxiety. The FS-14 is a 14-item self-rating
questionnaire that measures fatigue severity. A
lower score indicates a higher level of fatigue.
The POMS is a self-reporting tool for the
assessment of mood alterations in clinical and
psychiatric populations.24 This 65-item questionnaire contains seven components: tension-anxiety,
depression-dejection, anger-hostility, fatigue-inertia,
confusion-bewilderment, vigour-activity, and total
mood disturbance. Scores range from 0 (not at all) to
4 (extremely). Higher positive mood scores indicate
an ideal mood, whereas higher negative mood scores
indicate severe mood disturbance.
In addition to the above questionnaires,
each woman’s level of anxiety and worry before
consultation was assessed using a 0 to 10 cm visual
analogue scale (VAS). A higher value represents
a higher level of anxiety and worry about their
pregnancies. The VAS has previously been validated
with respect to its correlations with other measures
of anxiety.25 26
During the consultation, women were
counselled based on their ultrasound findings and
clinical diagnosis. These women used the VAS to
indicate their level of pregnancy-related anxiety
after consultation. Follow-up scans (1-2 weeks
later) were offered for women with a pregnancy
of uncertain viability. Actual pregnancy outcomes
were reassessed at 13 to 16 weeks, either by phone
or by retrieval of information from the hospital’s
centralised computer antenatal records system.
Statistical analysis
The sample size was calculated based on the number
of participants required for the primary study
to validate the scoring system.12 SPSS software
(Windows version 26.0; IBM Corp, Armonk [NY], United States) was used for data entry and analysis.
A 95% confidence interval (95% CI) was calculated
to determine the estimated errors and prevalence.
Descriptive analyses were used for demographic
data. The Chi squared test was used to explore
associations between categorical variables. The
Mann-Whitney U test was used to compare median
values when data were not normally distributed,
while the t test was used to compare means when
data were normally distributed. Univariate analyses
were performed to identify factors associated with
psychological distress or morbidity. Factors with
P values <0.1 in univariate analysis were entered
into multivariate analysis, which was conducted
via binary logistic regression. P values <0.05 were
considered statistically significant.
Results
Among the 1508 women who attended the EPAC
during the study period, 64 were excluded and 54
declined to participate; thus, 1390 women completed
the study (Fig). The demographic data are shown
in Table 1. At the first clinic visit, most women
(n=1048, 75.4%) had a viable pregnancy, 223 women
(16.0%) had a pregnancy of uncertain viability, and
119 (8.6%) women had a miscarriage. At 13 to 16
weeks of gestation, 1111 women (79.9%) had a viable
pregnancy, and an additional 160 (11.5%) women
had a miscarriage.
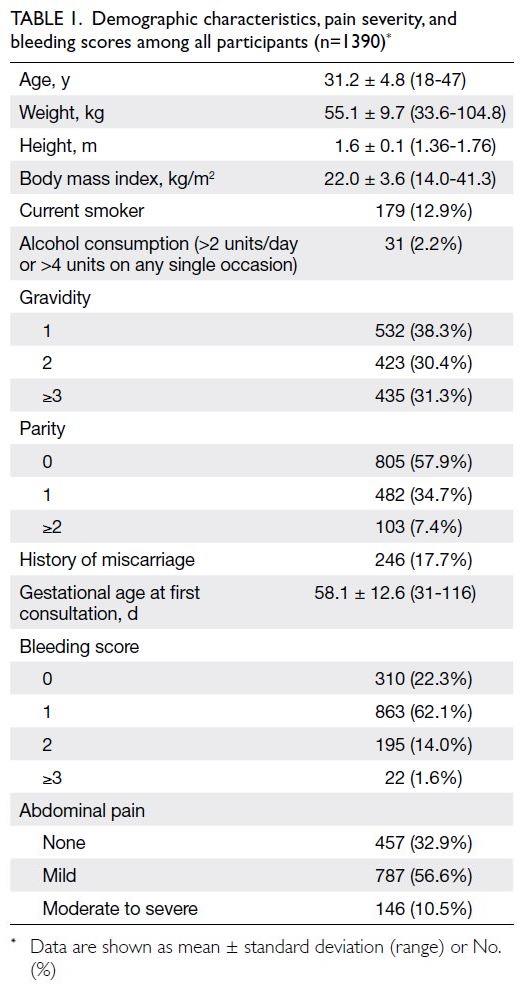
Table 1. Demographic characteristics, pain severity, and bleeding scores among all participants (n=1390)
The GHQ-12 (both bi-modal and Likert), BDI,
STAI-S, FS-14, POMS, and VAS results are presented in Table 2. Overall, 48.4% and 76.7% of women had
a GHQ-12 (bi-modal) score ≥4 and a GHQ-12
(Likert) score >12, respectively, indicating distress.
Among the viable pregnancy, uncertain viability,
and miscarriage groups, the percentages of women
with a GHQ-12 (bi-modal) score ≥4 (43-52%) and a
GHQ-12 (Likert) score >12 (73-83%) were similar.
Women with miscarriage had the highest GHQ-12
score and the highest percentages of a GHQ-12 (bi-modal)
score ≥4 and a GHQ-12 (Likert) score >12. The
miscarriage group also had relatively higher POMS
subscale scores for tension-anxiety, depression-dejection,
anger-hostility, confusion-bewilderment,
and total mood disturbance compared with women
who had other diagnoses.
The VAS scores for anxiety are also presented
in Table 2. The score before consultation was the
highest among women with a miscarriage (mean ±
standard deviation=7.02 ± 2.50). Although the scores for the viable pregnancy and uncertain viability
groups were significantly lower after consultation,
the score was substantially higher in the uncertain
viability group than in the viable pregnancy group.
Subgroup analysis showed that GHQ-12, BDI,
and POMS (except fatigue-inertia and vigour-activity
subscales) scores were significantly higher among
women with previous miscarriage than among those
without (Table 3). The bleeding score was strongly
positively correlated with the GHQ-12 (Likert) score
(correlation coefficient=0.56; P=0.032). Univariate
analysis revealed that compared with women who
had a lower bleeding score (<2), women with a higher
bleeding score (≥2) had a significantly higher risk of
having a GHQ-12 (bi-modal) score ≥4 (P=0.041),
a GHQ-12 (Likert) score >12 (P=0.025), and a BDI
score >12 (P=0.022) [Table 4]. There were statistically
significant but weak positive correlations between
the pain score and a GHQ-12 (bi-modal) score ≥4
(P=0.001), a BDI score >12 (P<0.001), and a POMS
total mood disturbance score (P<0.001), as well as
various subscales. Notably, the POMS confusion-bewilderment
subscale (correlation coefficient=0.93;
P<0.001) demonstrated a strong positive correlation
with the pain score.
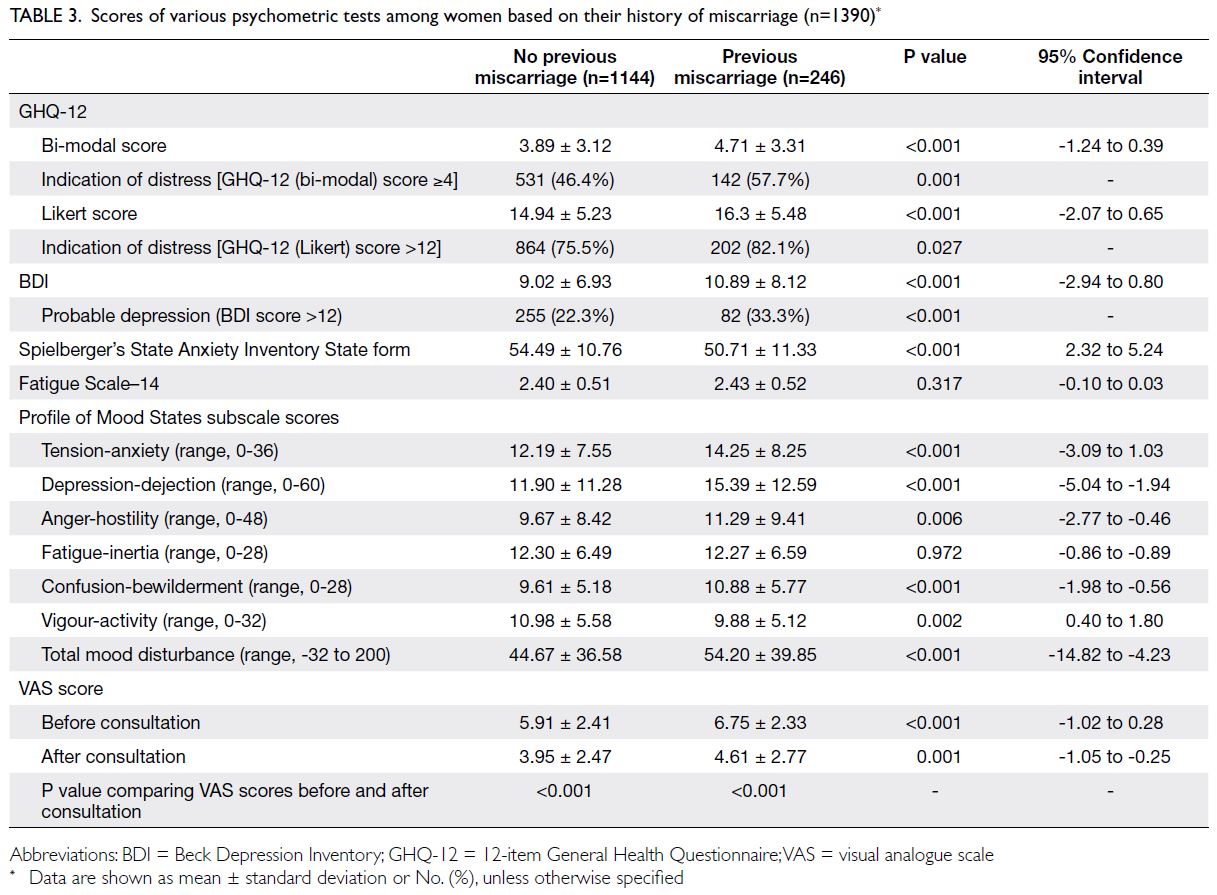
Table 3. Scores of various psychometric tests among women based on their history of miscarriage (n=1390)
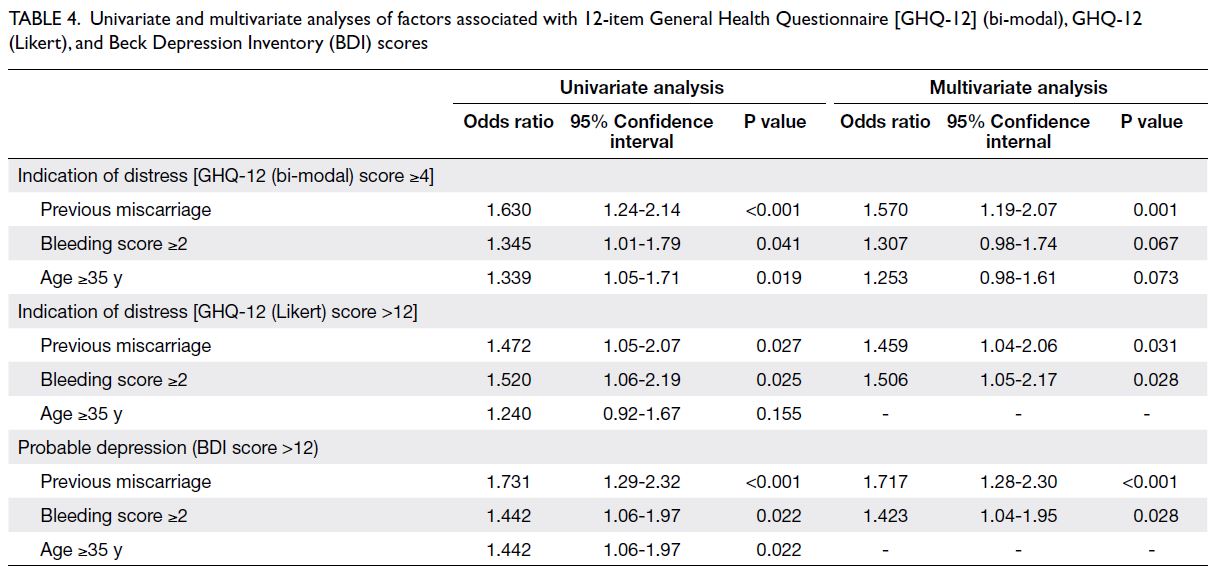
Table 4. Univariate and multivariate analyses of factors associated with 12-item General Health Questionnaire [GHQ-12] (bi-modal), GHQ-12 (Likert), and Beck Depression Inventory (BDI) scores
Statistically significant factors associated with
the various psychometric instrument scores were
subjected to multivariate analysis (Table 4). Previous
miscarriage was an independent risk factor for a
GHQ-12 (bi-modal) score ≥4 (odds ratio [OR]=1.570,
95% CI=1.19-2.07) and a GHQ-12 (Likert) score >12
(OR=1.459, 95% CI=1.04-2.06), indicating distress; it
was also a risk factor for a BDI score >12 (OR=1.717,
95% CI=1.28-2.30), suggesting probable depression.
A bleeding score ≥2 was an independent risk
factor for a GHQ-12 (Likert) score >12 (OR=1.506,
95% CI=1.05-2.17) and a BDI score >12 (OR=1.423,
95% CI=1.04-1.95).
Discussion
In this cohort study, nearly 50% and approximately
77% of women had a GHQ-12 (bi-modal) score ≥4
and a GHQ-12 (Likert) score >12, indicating distress.
Around one-fourth (24.5%) of women had a BDI
score >12, suggesting probable depression.
Regardless of diagnosis, the VAS score
decreased after consultation. However, the decrease
in VAS score was smaller for the uncertain viability
group, which may be attributed to the enhanced
anxiety resulting from uncertainty among these
women. This anxiety would be alleviated after an
ultrasound examination and consultation with an
accurate diagnosis. These findings emphasise the
need to implement an early pregnancy assessment
service that provides both clinical and psychological
guidance to alleviate anxiety among women with
problems in early pregnancy.
Emotional disturbances can have long-term effects on women with a previous miscarriage.
Lok et al19 reported consistently higher scores on the
GHQ-12 and BDI among women with a previous
miscarriage, although these scores could decrease
over time. In the present study, we observed a higher
level of distress among women with a previous
miscarriage, as demonstrated by the significantly
greater proportion of women with GHQ-12 (bi-modal)
score ≥4, GHQ-12 (Likert) score >12, and
BDI score >12. Profile of Mood States scores were
also significantly higher on all subscales, except for
the fatigue-inertia and vigour-activity subscales.
Similarly, the baseline VAS score before consultation
was significantly higher among women with a
previous miscarriage than among those without.
In multivariate analysis, previous miscarriage was
an independent risk factor for GHQ-12 (bi-modal)
score >4, GHQ-12 (Likert) score >12, and BDI
score >12. Baseline psychological morbidity may be
greater among women with a previous miscarriage
than among those without, consistent with findings
in other studies.3 27 Therefore, additional attention
and psychological support would be beneficial for women with greater distress and worse mood status.
A higher pain score was positively correlated
with higher levels of distress and anxiety, as indicated
by the positive relationships with various scales used
in the present study. Pain is associated with anxiety
and depression in pregnant women.28 Nevertheless,
we observed weak relationships between pain and
anxiety or distress, which might be related to the
subjective nature of pain assessment.
Women with moderate to heavy bleeding
(bleeding score ≥2) had significantly higher GHQ-12
(bi-modal), GHQ-12 (Likert), and BDI scores.
Additionally, multivariate analysis showed that
moderate to heavy bleeding (bleeding score ≥2) was
an independent risk factor for a GHQ-12 (bi-modal)
score ≥4, a GHQ-12 (Likert) score >12, and a BDI score
>12. Heavy bleeding is often regarded as a common
sign of threatened miscarriage. These findings
highlight the importance of addressing pain and
bleeding symptoms among women who attend early
pregnancy services. The underlying complications of
pregnancy, as well as anxiety and low mood in affected
women, should be promptly managed.
Pregnancy loss is associated with negative mood
status, including depression and anxiety.3 18 19 27 29
Whereas many studies have investigated the effects
of miscarriage or pregnancy loss on depression,
the effects of threatened miscarriage or early
pregnancy-related complaints on women have not
been extensively explored, despite the burdensome
experience of a threatened miscarriage that
appropriately causing anxiety in affected women.
Our results are consistent with findings by Zhu et al,6
who reported that a substantial proportion of
women with threatened miscarriage had symptoms
of depression or anxiety.
The present study had a large sample size and
a high rate of participation. Additionally, multiple
psychometric instruments were used to assess the
participants. The findings emphasise the importance
of assessing and managing depression and anxiety
symptoms in women with threatened miscarriage.
Mental health assessments should be performed
when women with threatened miscarriage attend
clinics and hospitals. Early recognition of relevant
mood problems will facilitate timely management.
Non-pharmacological interventions, such as
antenatal group therapy, constitute effective
treatment for pregnant women with anxiety
and depression.6 Pharmacological therapies (eg,
most selective serotonin reuptake inhibitors
and benzodiazepines) can be administered after
considering the side-effects of medications relative
to the risk of untreated antenatal depression and
anxiety.30
Limitations
Nevertheless, this study had some limitations. First,
it used a cross-sectional design without longitudinal
follow-up, and the subgroup analysis might have been
underpowered. Second, information was unavailable
regarding social factors (eg, education level or
marital status) and the presence of an underlying
psychiatric disorder, which might contribute to
differences in baseline mood status. Third, the study
did not include a comparison group of women
without symptoms of threatened miscarriage.
Conclusion
There is a considerable psychological burden among
women with early pregnancy problems and concerns
about future pregnancy viability. These women
experience emotional disturbances, as indicated by a
significant proportion of women in this study who had
high scores on psychometric tests. A gynaecologist
consultation, in combination with an ultrasound
assessment, is reassuring and can alleviate anxiety
among women with early pregnancy problems. This
study on maternal psychological outcomes provides
insights concerning psychological morbidity among women with threatened miscarriage in the first
trimester, while also demonstrating the usefulness
and feasibility of various psychometric instruments
in identifying women who require additional
psychological support. Further studies exploring
maternal psychological well-being later in pregnancy,
as well as fetal outcomes, are needed to determine
the long-term effects of anxiety and depression
among women with threatened miscarriage in the
first trimester.
Author contributions
Concept or design: OYK Wan, SSC Chan.
Acquisition of data: OYK Wan, JWK Kwok.
Analysis or interpretation of data: PNP Ip, K Ng.
Drafting of the manuscript: PNP Ip, K Ng.
Critical revision of the manuscript for important intellectual content: PNP Ip, K Ng, OYK Wan, JPW Chung, SSC Chan.
Acquisition of data: OYK Wan, JWK Kwok.
Analysis or interpretation of data: PNP Ip, K Ng.
Drafting of the manuscript: PNP Ip, K Ng.
Critical revision of the manuscript for important intellectual content: PNP Ip, K Ng, OYK Wan, JPW Chung, SSC Chan.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
As an editor of the journal, JPW Chung was not involved in
the peer review process. Other authors have disclosed no
conflicts of interest.
Funding/support
This research was supported by a grant from the Health and
Medical Research Fund of the former Food and Health Bureau, Hong
Kong SAR Government (Ref No.: 12131091). The study sponsor was not
involved in the collection, analysis, or interpretation of data,
or in the writing of the manuscript.
Ethics approval
This research was approved by the Joint Chinese University of
Hong Kong–New Territories East Cluster Clinical Research
Ethics Committee (Ref No.: CRE.2013.348). Written informed
consent was obtained from all participants.
References
1. Tong S, Kaur A, Walker SP, Bryant V, Onwude JL,
Permezel M. Miscarriage risk for asymptomatic women
after a normal first-trimester prenatal visit. Obstet Gynecol
2008;111:710-4. Crossref
2. Broen AN, Moum T, Bödtker AS, Ekeberg O. Predictors of
anxiety and depression following pregnancy termination:
a longitudinal five-year follow-up study. Acta Obstet
Gynecol Scand 2006;85:317-23. Crossref
3. Farren J, Jalmbrant M, Ameye L, et al. Post-traumatic
stress, anxiety and depression following miscarriage or
ectopic pregnancy: a prospective cohort study. BMJ Open
2016;6:e011864. Crossref
4. Jensen KL, Temple-Smith MJ, Bilardi JE. Health
professionals’ roles and practices in supporting women
experiencing miscarriage: a qualitative study. Aust N Z J
Obstet Gynaecol 2019;59:508-13. Crossref
5. Park C, Kang MY, Kim D, Park J, Eom H, Kim EA.
Prevalence of abortion and adverse pregnancy outcomes
among working women in Korea: a cross-sectional study. PLoS One 2017;12:e0182341. Crossref
6. Zhu CS, Tan TC, Chen HY, Malhotra R, Allen JC, Østbye T.
Threatened miscarriage and depressive and anxiety
symptoms among women and partners in early pregnancy.
J Affect Disord 2018;237:1-9. Crossref
7. Aksoy H, Aksoy Ü, İdem Karadağ Ö, et al. Effect of
threatened miscarriage on maternal mood: a prospective
controlled cohort study. J Clin Obstet Gynecol 2015;25:92-8. Crossref
8. Gelaye B, Sanchez SE, Andrade A, et al. Association
of antepartum depression, generalized anxiety, and
posttraumatic stress disorder with infant birth weight and
gestational age at delivery. J Affect Disord 2020;262:310-6. Crossref
9. Siu BW, Leung SS, Ip P, Hung SF, O’Hara MW. Antenatal
risk factors for postnatal depression: a prospective study of
Chinese women at maternal and child health centres. BMC
Psychiatry 2012;12:22. Crossref
10. Ibanez G, Bernard JY, Rondet C, et al. Effects of antenatal
maternal depression and anxiety on children’s early
cognitive development: a prospective cohort study. PLoS
One 2015;10:e0135849. Crossref
11. O’Connor TG, Heron J, Golding J, Glover V; ALSPAC
Study Team. Maternal antenatal anxiety and behavioural/emotional problems in children: a test of a programming
hypothesis. J Child Psychol Psychiatry 2003;44:1025-36. Crossref
12. Wan OY, Chan SS, Chung JP, Kwok JW, Lao TT, Sahota DS.
External validation of a simple scoring system to
predict pregnancy viability in women presenting to an
early pregnancy assessment clinic. Hong Kong Med J
2020;26:102-10. Crossref
13. Chan DW, Chan TS. Reliability, validity and the structure
of the General Health Questionnaire in a Chinese context.
Psychol Med 1983;13:363-71. Crossref
14. Shek DT. Reliability and factorial structure of the Chinese
version of the Beck Depression Inventory. J Clin Psychol
1990;46:35-43. Crossref
15. Shek DT. Reliability and factorial structure of the Chinese
version of the State-Trait Anxiety Inventory. J Psychopathol
Behav Assess 1988;10:303-17. Crossref
16. Liang Y, Wang L, Yin X. The factor structure of the 12-item
General Health Questionnaire (GHQ-12) in young Chinese
civil servants. Health Qual Life Outcomes 2016;14:136. Crossref
17. Rao WW, Yang MJ, Cao BN, et al. Psychological distress in
cancer patients in a large Chinese cross-sectional study. J
Affect Disord 2019;245:950-6. Crossref
18. Lok IH, Lee DT, Yip SK, Shek D, Tam WH, Chung TK.
Screening for post-miscarriage psychiatric morbidity. Am
J Obstet Gynecol 2004;191:546-50. Crossref
19. Lok IH, Yip AS, Lee DT, Sahota D, Chung TK. A 1-year
longitudinal study of psychological morbidity after
miscarriage. Fertil Steril 2010;93:1966-75. Crossref
20. Kong GW, Lok IH, Yiu AK, Hui AS, Lai BP, Chung TK.
Clinical and psychological impact after surgical, medical
or expectant management of first-trimester miscarriage—a
randomised controlled trial. Aust N Z J Obstet Gynaecol
2013;53:170-7. Crossref
21. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An
inventory for measuring depression. Arch Gen Psychiatry
1961;4:561-71. Crossref
22. Hedberg AG. Review of State–Trait Anxiety Inventory.
[Review of the Book State–Trait Anxiety Inventory, by C.
D. Spielberger, R. L. Gorsuch & R. E. Lushere]. Prof Psychol
1972;3:389-90. Crossref
23. Bann CM, Parker CB, Grobman WA, et al. Psychometric
properties of stress and anxiety measures among
nulliparous women. J Psychosom Obstet Gynaecol
2017;38:53-62. Crossref
24. McNair DM, Heuchert P. Profile of mood states: technical
update. North Tonawanda (NY): Multi-Health Systems;
2013. Crossref
25. Williams VS, Morlock RJ, Feltner D. Psychometric
evaluation of a visual analog scale for the assessment of
anxiety. Health Qual Life Outcomes 2010;8:57. Crossref
26. Facco E, Stellini E, Bacci C, et al. Validation of visual
analogue scale for anxiety (VAS-A) in preanesthesia
evaluation. Minerva Anestesiol 2013;79:1389-95.
27. Cumming GP, Klein S, Bolsover D, et al. The emotional
burden of miscarriage for women and their partners:
trajectories of anxiety and depression over 13 months.
BJOG 2007;114:1138-45. Crossref
28. Virgara R, Maher C, Van Kessel G. The comorbidity of
low back pelvic pain and risk of depression and anxiety
in pregnancy in primiparous women. BMC Pregnancy
Childbirth 2018;18:288. Crossref
29. Kong GW, Lok IH, Lam PM, Yip AS, Chung TK. Conflicting
perceptions between health care professionals and patients
on the psychological morbidity following miscarriage. Aust
N Z J Obstet Gynaecol 2010;50:562-7. Crossref
30. Vitale SG, Laganà AS, Muscatello MR, et al.
Psychopharmacotherapy in pregnancy and breastfeeding.
Obstet Gynecol Surv 2016;71:721-33. Crossref



