Hong Kong Med J 2023 Oct;29(5):456–8 | Epub 2 Aug 2023
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Surgical correction of persistent eyelid lymphoedema after radiotherapy: four case reports
HY Chan, MB, BS, MRCSEd1; Leo KY Chan, MB, ChB, MSc2; Tracy YT Kwok, FCOphthHK, FHKAM2; Hunter KL Yuen, FRCSEd, FRCOphth (UK)2
1 Department of Ophthalmology and Visual Sciences, Prince of Wales Hospital, Hong Kong SAR, China
2 Department of Ophthalmology, Hong Kong Eye Hospital, Hong Kong SAR, China
Corresponding author: Dr HY Chan (chy896@ha.org.hk)
Case presentations
Case 1
A 40-year-old man presented with right upper
lid swelling for several months. There was no
pain or redness. He had received radiotherapy for
nasopharyngeal carcinoma 12 years ago. The swelling
did not respond to antibiotics nor non-steroidal
anti-inflammatory medication. On examination,
there was mechanical ptosis and loss of skin crease.
The marginal reflex distance, palpebral fissure height
(PFH), and levator function on the right eye were
2 mm, 8 mm, and 8 mm, respectively. Extraocular
movement was normal and there was no proptosis
(Fig 1a).
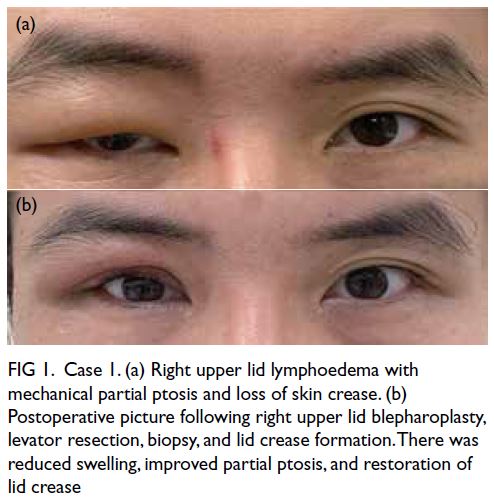
Figure 1. Case 1. (a) Right upper lid lymphoedema with mechanical partial ptosis and loss of skin crease. (b) Postoperative picture following right upper lid blepharoplasty, levator resection, biopsy, and lid crease formation. There was reduced swelling, improved partial ptosis, and restoration of lid crease
The diagnosis was periocular lymphoedema
affecting mainly the right upper lid. He underwent
right upper lid blepharoplasty, levator resection with
biopsy, debulking of orbital septum, preseptal tissues and preaponeurotic fat pad, and lid crease formation
under local anaesthesia. Histological examination
revealed skin, adipose tissue and fibrovascular tissue
with no evidence of malignancy. Postoperatively,
there was significant improvement in symptoms and
cosmesis (Fig 1b) and no recurrence after 9 months.
Case 2
A 57-year-old woman underwent left
hemiglossectomy and adjuvant radiotherapy for
carcinoma of tongue. She presented with gradual
swelling of the left upper lid causing visual
obstruction. Examination revealed left upper lid
swelling with secondary mechanical ptosis (Fig 2a). Her marginal reflex distance PFH, and levator
function on the left eye were 0 mm, 4 mm, and 9 mm,
respectively. There was also left hemifacial swelling.
Visual acuity, intraocular pressure, fundal and pupil
examination, and extraocular movement were all normal. There were no signs of recurrent carcinoma of tongue and no palpable cervical lymph nodes.
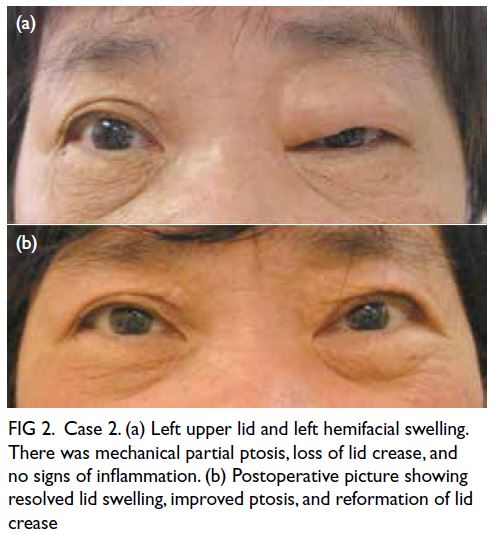
Figure 2. Case 2. (a) Left upper lid and left hemifacial swelling. There was mechanical partial ptosis, loss of lid crease, and no signs of inflammation. (b) Postoperative picture showing resolved lid swelling, improved ptosis, and reformation of lid crease
Similar to Case 1, surgical correction of eyelid
lymphoedema was performed. Postoperatively, lid
swelling resolved with reformation of lid crease
(Fig 2b). The patient remained well 4 years after the surgery with no recurrence.
Case 3
A 71-year-old man received radiotherapy for
nasopharyngeal carcinoma in 1982. He presented
with persistent non-pitting left upper lid swelling
for 20 years. Incisional biopsy performed in 2004
revealed non-specific changes with no malignant
cells. Additional eyelid surgery was offered but
the patient opted for conservative management.
Interval computed tomography imaging showed left
eyelid swelling with no retrobulbar mass, and rectus
muscles were not thickened. Examination revealed
left upper lid swelling with secondary mechanical
ptosis and loss of lid crease. Marginal reflex distance,
PFH, and levator function on the left eye were
0 mm, 1 mm, and 5 mm, respectively. Extraocular
movement and other physical examinations were
normal.
Due to persistent symptoms, the patient elected
surgical correction of eyelid lymphoedema. Biopsy
showed no signs of malignancy. Postoperatively, left
upper lid swelling resolved. The patient remained
well 3 years postoperatively with no recurrence.
Case 4
A 65-year-old woman presented with persistent
right upper lid swelling in 2008. She had a history of
nasopharyngeal carcinoma (T2N2M0) treated with
radiotherapy in 1995. There was non-pitting oedema
of the right upper lid. Liver and renal function tests
were normal. She had no oedema in her extremities
or elsewhere.
Computed tomography of the orbits showed
smooth soft tissue oedema of the right upper lid with
no abnormal mass. Cavernous sinuses were normal.
Patchy sclerosis in the skull base was present and
thought to represent post-radiotherapy changes.
Right upper lid blepharoplasty had been
performed elsewhere in March 2009, where
excessive and thickened skin was excised together
with hypertrophic orbicularis muscles. The orbital
septum was kept intact with preservation of the
preaponeurotic fat pad. A similar repeat procedure
was performed 4 months later by the same surgeon
for persistent symptoms.
In 2019, the patient presented to us with
residual bilateral upper lid oedema. Palpebral fissure
height was 5 mm on the right eye and 6 mm on the left.
Marginal reflex distance was 0 mm on the right eye
and 1 mm on the left. Levator function was 9 mm on
both eyes. There was secondary mechanical partial ptosis, loss of lid crease, and facial lymphoedema.
Surgical correction of eyelid lymphoedema
was performed. Histological examination was
compatible with lymphoedema. The patient
recovered well postoperatively and there was no
recurrence 6 months after surgery.
Discussion
There are only a few reports of eyelid lymphoedema
following neck dissection, surgery or radiation.1 2 3
As none of our cases underwent neck dissection,
we hypothesise that radiotherapy alone can impede
lymphatic drainage with consequent periocular
lymphoedema. In this series, eyelid lymphoedema
was frequently related to nasopharyngeal carcinoma,
unlike other series.
Eyelid lymphoedema presents as a non-pitting
oedema with thickening of the eyelid. In cases with
severe swelling, visual field defect and disfigurement
may occur.
Rosacea is the most reported eyelid
lymphoedema association, albeit rare. More common
presentations are blepharitis, conjunctivitis, and
meibomianitis.3 4 5 6 7
Lymphoedema can usually be managed
conservatively with manual drainage, compression
garments, and skin care.8 Medical therapy with
tetracycline and steroids have limited efficacy.4 5 7
Surgical treatment by debulking and split thickness
skin grafting has been reported with favourable
results.3 4 9 Lymphovenous anastomosis or bypass
is also performed to divert lymphatic drainage to
venous circulation.10 Nonetheless this is difficult in
the periocular region where a lack of large superficial
veins may result in an unsightly facial scar. Therefore,
surgical debulking may remain the treatment of
choice.
For surgical debulking, excessive skin and
orbicularis should be addressed. Orbital septum
debulking is essential since fluid tends to accumulate
in this loose connective tissue. Debulking of the
preaponeurotic fat pad can reduce upper lid swelling
and enhance formation of skin crease. In our fourth
case without such debulking, there was residual
swelling. We addressed this in her last surgery
resulting in marked improvement. In all four cases,
there was no recurrence as the loose connective
tissue was removed with orbital septum and
preaponeurotic fat pad debulking. Levator resection
should be performed in cases with long-standing
oedema and levator muscle dysfunction. Skin crease
forming sutures are placed for symmetry with the
opposite eye, noting that Asian patients have thicker
skin and orbicularis muscle, affecting skin crease
formation and margin reflex distance. We prefer an
incision 1 to 2 mm lower than the opposite normal
side for better symmetry. Although surgery can
improve eyelid oedema, patients should be informed that abnormal-appearing skin will persist. The longevity of improvement may be enhanced with
presence of scar tissue making oedematous fluid less
likely to accumulate.
Author contributions
Concept or design: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: HY Chan, HKL Yuen.
Acquisition of data: All authors.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: HY Chan, HKL Yuen.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
As an editor of the journal, HKL Yuen was not involved in the peer review process. Other authors have disclosed no
conflicts of interest.
Declaration
Case 2 in this study has been previously published in part in: Yuen KLH, Kwok YT. Surgical management of unusual eyelid
swelling. iPlastics: official newsletter of the Asia Pacific Society
of Ophthalmic Plastic and Reconstructive Surgery: 2016; 2(4):
4-6. Permission from the newsletter editor for publication of
the case has been obtained. The authors confirm that there
is no intentional or unintentional plagiarism in the present
manuscript.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This study was conducted in accordance with the Declaration of Helsinki. All patients were informed of the purpose of
the study and their consent was obtained for all treatments,
procedures, photography, and publication.
References
1. Sagili S, Selva D, Malhotra R. Eyelid lymphedema following neck dissection and radiotherapy. Ophthalmic Plast Reconstr Surg 2013;29:e146-9. Crossref
2. Possin ME, Burkat CN. Severe symmetric and chronic lower eyelid lymphedema in the setting of neck surgery and psoriasis. Open J Ophthalmol 2012;2:103-9. Crossref
3. Chalasani R, McNab A. Chronic lymphedema of the eyelid: case series. Orbit 2010;29:222-6. Crossref
4. Bernardini FP, Kersten RC, Khouri LM, Moin M, Kulwin DR, Mutasim DF. Chronic eyelid lymphedema and acne rosacea. Report of two cases. Ophthalmology 2000;107:2220-3. Crossref
5. Carruth BP, Meyer DR, Wladis EJ, et al. Extreme eyelid lymphedema associated with rosacea (Morbihan disease): case series, literature review, and therapeutic considerations. Ophthalmic Plast Reconstr Surg 2017;33(3S Suppl 1):S34-8. Crossref
6. Marzano A, Vezzoli P, Alessi E. Elephantoid oedema of the eyelids. J Eur Acad Dermatol Venereol 2004;18:459-62. Crossref
7. Lai TF, Leibovitch I, James C, Huilgol SC, Selva D. Rosacea lymphoedema of the eyelid. Acta Ophthalmol Scand 2004;82:765-7. Crossref
8. Mayrovitz HN. The standard of care for lymphedema: current concepts and physiological considerations. Lymphat Res Biol 2009;7:101-8. Crossref
9. Kabir SM, Raurell A, Ramakrishnan V. Lymphoedema of the eyelids. Br J Plast Surg 2002;55:153-4. Crossref
10. Chang EI, Skoracki RJ, Chang DW. Lymphovenous anastomosis bypass surgery. Semin Plast Surg 2018;32:22-7. Crossref

