Hong Kong Med J 2023 Oct;29(5):448–52 | Epub 15 Sep 2023
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PERSPECTIVE
Hong Kong Academy of Medicine position paper on postgraduate medical education 2023
HY So, FHKAM (Anaesthesiology)1; Philip KT Li, FHKAM (Medicine)2; Paul BS Lai, FHKAM (Surgery)3; Alexander CL Chan, FHKAM (Pathology)4; Karen KL Chan, FHKAM (Obstetrics and Gynaecology)5; TM Chan, FHKAM (Medicine)6; David VK Chao, FHKAM (Family Medicine)7; SN Chiu, FHKAM (Psychiatry)8; KM Chu, FHKAM (Surgery)9;
KY Ho, FHKAM (Dental Surgery)10; Hugh Simon HS Lam, FHKAM (Paediatrics)11; CK Law, FHKAM (Radiology)12; SW Law, FHKAM (Orthopaedic Surgery)13; CM Ngai, FHKAM (Otorhinolaryngology)14; FC Pang, FHKAM (Community Medicine)15; Clement CY Tham, FCOphthHK, FHKAM (Ophthalmology)16; Clara WY Wu, FHKAM (Emergency Medicine)17; Gilberto KK Leung, FHKAM (Surgery)18
1 Educationist, Hong Kong Academy of Medicine / President, The Hong Kong College of Anaesthesiologists, Hong Kong SAR, China
2 Vice-President (Education and Examinations), Hong Kong Academy of Medicine, Hong Kong SAR, China
3 Immediate Past Vice-President (Education and Examinations), Hong Kong Academy of Medicine, Hong Kong SAR, China
4 President, The Hong Kong College of Pathologists, Hong Kong SAR, China
5 President, The Hong Kong College of Obstetricians and Gynaecologists, Hong Kong SAR, China
6 President, Hong Kong College of Physicians, Hong Kong SAR, China
7 President, The Hong Kong College of Family Physicians, Hong Kong SAR, China
8 President, The Hong Kong College of Psychiatrists, Hong Kong SAR, China
9 President, The College of Surgeons of Hong Kong, Hong Kong SAR, China
10 President, The College of Dental Surgeons of Hong Kong, Hong Kong SAR, China
11 President, Hong Kong College of Paediatricians, Hong Kong SAR, China
12 President, Hong Kong College of Radiologists, Hong Kong SAR, China
13 President, The Hong Kong College of Orthopaedic Surgeons, Hong Kong SAR, China
14 President, The Hong Kong College of Otorhinolaryngologists, Hong Kong SAR, China
15 President, Hong Kong College of Community Medicine, Hong Kong SAR, China
16 Immediate Past President, The College of Ophthalmologists of Hong Kong, Hong Kong SAR, China
17 President, Hong Kong College of Emergency Medicine, Hong Kong SAR, China
18 President, Hong Kong Academy of Medicine, Hong Kong SAR, China
Corresponding author: Prof Gilberto KK Leung (gilberto@hku.hk)
Introduction
The Hong Kong Academy of Medicine (HKAM)
is committed to promoting the development of
postgraduate medical education (PGME) and
continuing medical education (CME). In 2010,
HKAM published a position paper outlining the
necessary reforms to modernise PGME.1 Progress
has been made in areas such as defining core
competencies, incorporating communication skills
into specialist training, standardising training
programmes, and implementing comprehensive
assessments. An Education Office, operated by The
Hong Kong Jockey Club Innovative Learning Centre
for Medicine, has been established under the HKAM
Education Committee to support the development
of PGME.
As HKAM celebrates its 30th Anniversary,
we aim to build upon the foundation established
in the 2010 Position Statement by embracing
new opportunities and adapting to the evolving
professional landscapes of medical education
and healthcare delivery.2 In light of this, HKAM
organised the Tripartite Medical Education
Conference (MEC) 2023 and the Strategic Planning Retreat on Education and Training 2023 to evaluate
existing frameworks and formulate actions for the
future.
The Tripartite MEC 2023, themed ‘Actualising
the Curriculum Continuum’, brought together
local and international medical experts to share
experiences and insights on optimal alignment of
postgraduate and undergraduate education. In the
roundtable discussion on 14 January 2023, titled ‘Ten
Years Down the Line’, four distinguished speakers
discussed critical topics including the challenges
faced by young doctors; the importance of quality
assurance, role modelling, and demographic
shifts; the need for trust in the healthcare system;
the impacts of technology and data sciences on
healthcare delivery; the concept of mandatory
teaching skills instruction for trainees; and the
importance of resilience and well-being among
young doctors.3
The Strategic Planning Retreat on Education
and Training, held on 4 March 2023, aimed to
establish directions for HKAM in terms of fulfilling
its fundamental responsibilities and functions within
PGME and CME.
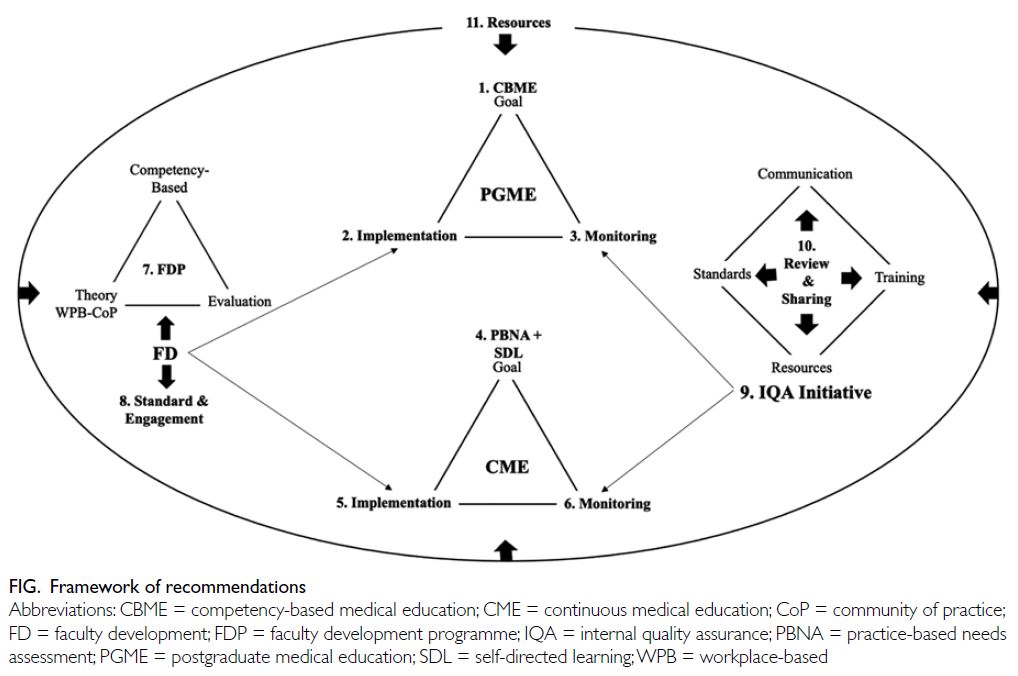
This position paper represents an update and
extension of the 2010 Position Statement based
on discussions arising from the Tripartite MEC
2023, the results of a survey conducted before
and discussed during the Retreat, and relevant
literature.4 The Figure illustrates the framework of
the recommendations made in this position paper.
Postgraduate medical education
Postgraduate medical education traditionally focused
on clinical competency alone. However, there is
increasing recognition that modern professional
training must prepare doctors to adapt to rapid
advancements in medicine, understand patient
perspectives, appreciate other professionals’ skills,
and work effectively in teams.2 5 Therefore, training
for ‘Hong Kong’s Specialist’ must encompass the
seven domains of competencies defined by HKAM.1
Postgraduate medical education has
traditionally been time-based, but there are
compelling reasons to move towards competency-based
medical education (CBME),6 which focuses on specialists’ abilities and organises competencies
based on societal and patient needs.2 While the 2010 Position Statement recommended a combination
of competency-based and time-based training,
the current view is that time should be regarded
as a resource for learning, rather than the basis for
competency progression.2 5 Therefore, instead of a
combination of time-based and CBME approaches,the focus should be on advancing towards CBME as the primary approach.
Recommendation 1: Colleges should continue to advance specialist training towards CBME.
Advancement towards CBME presents
challenges that can be addressed through four key
strategies.5 7 First, CBME is a complicated concept
that significantly differs from current practice.
Effective communication with stakeholders is
essential to engage them in this resource-intensive
change. Second, CBME requires trainers to master
teaching skills that may not be well-known. Faculty
development programmes (FDPs) are crucial. Third,
the alignment of learning and assessment methods
with CBME approaches requires educational
standards and procedures to be redesigned. Finally,
PGME is a relatively new discipline with limited
academic presence. Knowledge specific to our context
should be generated to guide implementation.2
Recommendation 2: HKAM and the Colleges should undertake the following actions to implement CBME.
(1) develop and implement a comprehensive
communication plan through appropriate channels
to effectively engage with each stakeholder segment;
(2) design and deliver FDPs that empower Fellows to
master the teaching and facilitation skills required
for CBME; (3) redesign training and assessment standards and procedures to align with the principles
and approaches of CBME; and (4) support and
participate in research activities that advance the field
of PGME and generate evidence concerning CBME
benefits that can be used to engage stakeholders.
Competency-based medical education is
a constantly evolving approach that focuses on
achieving better healthcare through effective medical
education.6 Regular evaluations are necessary to ensure progress and continuous improvement.
Recommendation 3: HKAM and the Colleges should establish a mechanism to regularly evaluate
CBME implementation and impact. A timeline for
this process should be implemented and external
reviewer involvement should be considered.
Continuing medical education/continuous professional development
Because our profession is constantly advancing,
specialists must engage in lifelong learning, known
as continuing medical education/continuous
professional development (CME/CPD).8 The
Institute of Medicine states that effective CME/CPD
should prepare healthcare professionals to provide
patient-centred care, work in teams, use evidence-based
practice, apply quality improvement, and
utilise health informatics.9 However, current CME
practices, which mainly involve didactic activities
that are not always related to patient outcomes,
have demonstrated limited impacts on physician
practice.8 Thus, there is a need for transformation.
Continuing medical education/continuous
professional development can improve performance
and patient outcomes if it is driven by practice-based
needs assessment, is ongoing, uses interactive
learning methods, and is contextually relevant.10
Recommendation 4: HKAM and the Colleges should promote lifelong learning driven by practice-based
needs assessment and self-directed learning.
The transformation of CME/CPD faces several
challenges. First, stakeholders are unfamiliar with
the new paradigm; effective communication is
essential to engage them. Second, many learners
currently view CME/CPD as a mere requirement
for specialist registration rather than an opportunity
for lifelong learning. This motivational problem
requires both engagement efforts and changes in
the CME system. Third, there is a need to empower
Fellows and CME/CPD providers to use methods
that support adult learning, and online learning is
a particularly promising method for this learning.11
Finally, many learners lack the skills and personal
attributes needed for self-directed learning; they
require support to acquire these abilities.12
Recommendation 5: HKAM and the Colleges should undertake actions to transform CME/CPD, including:
(1) devise and deliver a comprehensive
communication plan to effectively engage all
stakeholders; (2) reform the structure and redesign
the standards and procedures of CME requirements
and accreditation to align with the new CME
paradigm; (3) design and implement FDPs to
empower Fellows and possibly other CME providers
to use learning methods which support adult learning;
(4) nurture the capacities of learners to practise self-directed
learning; (5) support the development of
online learning through the provision of technology
and relevant training in educational practices; and
(6) establish partnerships with overseas CME/CPD
accreditation bodies.
The process of transforming CME/CPD will
be a long journey that requires regular evaluation to
ensure forward movement in the correct direction.
Recommendation 6: HKAM and the Colleges should establish a mechanism and regularly
evaluate the progress of CME transformation.
Faculty development
The development of PGME and CME relies on
clinical educators who are equipped with modern
medical education knowledge and skills. This
reliance highlights the critical need for faculty
development.13
A generic FDP that can be adapted to meet
specific needs of each College would be beneficial.
The objectives of the generic FDP should not be
limited to teaching skills; they should also focus
on motivating Fellows to participate in education,
emphasise professional identity, and build leadership
skills for Fellows with leading roles.14 15 The generic
FDP should be competency-based, be driven by
sound education theories, promote workplace
learning, foster the development of communities
of practice, and be evaluated for continuous
improvement.13 14 15
Recommendation 7: HKAM and the Colleges should enhance teaching skills, motivate
participation in educational activities, and
strengthen leadership in medical education through
the introduction of FDPs.
The Academy should create competency-based
curricula for FDPs that can be implemented
for clinical teachers at various levels, according to
their respective roles and responsibilities. Faculty
development programmes should comprise
induction courses or workshops based on theories
of situated learning, experiential learning, and adult
learning. Additionally, opportunities for workplace learning and mutual learning should be provided
through communities of practice involving clinical
educators. Moreover, HKAM and the Colleges
should establish mechanisms to evaluate FDPs using
both quantitative and qualitative methods.
The statuses of trainers should be enhanced
to engage Fellows in teaching activities. The
Academy should establish a benchmark, which
can be customised by each College, for trainer
accreditation and define trainers’ expected teaching
responsibilities. Additionally, HKAM and the
Colleges should explore ways to acknowledge
Fellows’ contributions to education. For example,
training activities should be eligible for credit
towards CME/CPD.
Recommendation 8: HKAM and the Colleges should develop a set of guidelines for trainers, a
system for certifying trainers, and strategies to
cultivate a distinguished image of clinical educators.
Quality assurance
As providers of PGME and CME, HKAM and
the Colleges are responsible for ensuring quality
and must be accountable for the training they
provide.16 However, quality assurance is not widely
regarded as a priority; greater communication and
encouragement are needed.
We focus on internal quality assurance (IQA),
which involves implementing activities and processes
that control, monitor, improve, and enhance
educational quality.17 The IQA cycle consists of three
steps: defining measurement parameters, judging
quality based on collected data, and taking actions
for improvement.17
The World Federation for Medical Education
has defined standards in eight areas for PGME,18
two of which were highlighted during the Retreat:
trainer quality and assessments. Evaluation of the
psychometric properties of assessments can be
supported by psychometricians and appropriate
software; training is necessary to interpret findings.
Qualitative methods are often used to collect
valuable data for improvement purposes. However,
Fellows may require training to become familiar
with these methods.
Next, criteria and standards can be established
to interpret the collected data and assess the quality
of education.17 Finally, actions taken for improvement
require the assignment of responsibility as well as the
development of a culture of continuous improvement
and a sense of ownership and commitment among
learners and staff.17 19
Recommendation 9: HKAM and Colleges should implement a structured quality assurance initiative
by taking the following steps:
(1) develop and execute a comprehensive
communication strategy that reaches each
stakeholder segment through appropriate channels;
(2) establish quality assurance standards; (3) provide
training to Fellows responsible for quality assurance
on quality assurance fundamentals, standard
establishment, quality metric interpretation, and
qualitative evaluation methods; and (4) allocate
resources to facilitate quality assurance initiatives.
Recommendation 10: HKAM and Colleges should create a mechanism for Colleges to regularly review
and share their experiences in quality assurance and improvement activities.
For IQA to yield helpful results, the assessment
tasks must be integrated into the Colleges’ daily
operations and executed in an organised and
structured manner.20 The Academy and the Colleges
should scrutinise their quality assurance procedures
to ensure compliance with these conditions.
Recommendation 11: HKAM should liaise with the Government, the Hospital Authority, and other
funding sources to secure resources that support
advancement towards CBME, transformation
of CME/CPD, faculty development, and quality
assurance. HKAM should work in partnership with
the Hospital Authority to identify training needs
for the whole territory, rather than the Hospital
Authority alone.
Successful implementation of the above 11
recommendations will require significant resource
investment. Both Fellows and doctors in training will
need to devote considerable time and effort towards
these aspirations. However, because of staffing
limitations and heavy clinical workload, it may be
challenging to assign the necessary personnel and
accomplish the recommended actions. The Academy
must liaise with the Government and the Hospital
Authority to obtain their support.
There are also needs for other resources
such as medical education expertise, information
technology, and secretarial assistance. Considering
the staffing limitations, it is essential to explore
the possibility of utilising technology. E-learning
can be developed that allows trainers to focus on
workplace-based learning activities rather than
information transmission. In addition, the Academy
should seek potential funding resources to support
these initiatives.
Conclusion
The recommendations expressed in this position
paper are the products of intense deliberations
involving all Colleges and the Education Office of
HKAM, as well as leaders from the two medical
schools and the Hospital Authority. The progressive implementation of these recommendations is
expected to provide an evidence-based and effective
framework of postgraduate training in the context
of new opportunities and challenges arising from
changes in professional landscapes, healthcare
delivery models, and societal needs.
Author contributions
All authors contributed to the concept or design, acquisition of data, analysis or interpretation of data, drafting of the
manuscript, and critical revision for important intellectual
content of the manuscript. All authors had full access to the
data, contributed to the study, approved the final version
for publication, and take responsibility for its accuracy and
integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
The authors thank the following individuals and parties for their contributions to the article:
- Prof Francis KL Chan, Dean, Faculty of Medicine, The Chinese University of Hong Kong (for participation in Tripartite Medical Education Conference [MEC] 2023: roundtable);
- Dr Pamela PW Lee, Assistant Dean (Clinical Curriculum), Li Ka Shing Faculty of Medicine, The University of Hong Kong (for participation in Tripartite MEC 2023: roundtable);
- Dr Tony PS Ko, Chief Executive of the Hospital Authority (for participation in Tripartite MEC 2023: roundtable);
- Education Office, Hong Kong Academy of Medicine [HKAM] (for conducting survey and preparing the Strategic Planning and Retreat on Education and Training 2023 and Tripartite MEC 2023);
- Secretariat, HKAM (for conducting survey and preparing the Strategic Planning and Retreat on Education and Training 2023 and Tripartite MEC 2023); and
- Mr Johnson ST Lo, Chief Innovative Learning Officer, HKAM (for preparing manuscripts).
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
1. Hong Kong Academy of Medicine. Position paper on postgraduate medical education. 2010. Available from:
https://www.hkam.org.hk/sites/default/files/HKAM_position_paper.pdf. Accessed 28 Aug 2023.
2. So HY. Postgraduate medical education: see one, do one, teach one…and what else? Hong Kong Med J 2023;29:104.e1-
9. Crossref
3. Lai PB, Wong GT, Wong SY. ‘Ten Years Down the Line’: a roundtable on the progress and advancement of medical education and training. Hong Kong Med J 2023;29:195-7. Crossref
4. Hong Kong Academy of Medicine. Summary report of Strategic Planning Retreat on Education and Training
held on 4 March 2023. 2023. Available from: https://online.hkam.org.hk/lms/retreat2023/Report-on-Strategic-Planning-Retreat-with-appendixes.pdf. Accessed 28 Aug 2023.
5. Frank JR, Danoff D. The CanMEDS initiative: implementing an outcomes-based framework of physician competencies. Med Teach 2007;29:642-7. Crossref
6. Holmboe ES, Sherbino J, Englander R, Snell L, Frank JR; ICBME Collaborators. A call to action: the controversy of
and rationale for competency-based medical education.
Med Teach 2017;39:574-81. Crossref
7. Caverzagie KJ, Nousiainen MT, Ferguson PC, et al. Overarching challenges to the implementation of competency-based medical education. Med Teach 2017;39:588-93. Crossref
8. Stevenson R. Learning and Behaviour in Medicine: A Voyage Around CME and CPD. London, England: CRC Press; 2022. Crossref
9. Institute of Medicine Committee on Planning a Continuing Health Professional Education Institute. Redesigning Continuing Education in The Health Professions. Washington DC: National Academies Press; 2010.
10. Cervero RM, Gaines JK. The impact of CME on physician performance and patient health outcomes: an updated synthesis of systematic reviews. J Cont Educ Health Prof 2015;35:131-8. Crossref
11. Gerstein J. Moving from education 1.0 through education 2.0 towards education 3.0. In: Hase S, Kenyon C, editors. Self-Determined Learning: Heutagogy in Action. London, England: Bloomsbury Academic; 2015: 83-98.
12. Sawatsky AP, Ratelle JT, Bonnes SL, Egginton JS, Beckman TJ. A model of self-directed learning in internal
medicine residency: a qualitative study using grounded
theory. BMC Med Educ 2017;17:31. Crossref
13. Steinert Y. Faculty development: core concepts and principles. In: Steinert Y. Faculty Development in the
Health Professions: A Focus on Research and Practice.
Dordrecht: Springer; 2013: 3-25. Crossref
14. Steinert Y, Naismith L, Mann K. Faculty development initiatives designed to promote leadership in medical education. A BEME systematic review: BEME Guide No. 19. Med Teach 2012;34:483-503. Crossref
15. Steinert Y. Developing medical educators: a journey, not a
destination. In: Swanwick T, Forrest K, O’Brien BC, editors.
Understanding Medical Education: Evidence, Theory, and
Practice, Third Edition. The Association for the Study of
Medical Education (ASME); 2019: 531-48. Crossref
16. Vroeijenstijn AI. Quality assurance in medical education. Acad Med 1995;70(7 Suppl):S59-67; discussion S68-9. Crossref
17. Stalmeijer R, Dolmans D, van Berkel H, Wolfhagen I. Quality assurance. In: van Berkel H, Scherpbier A, Hillen
H. editors. Lessons from Problem Based Learning. Oxford,
United Kingdom: Oxford University Press; 2010: 157-66. Crossref
18. World Federation for Medical Education. WFME Global Standards for Quality Improvement in PGME. 2023.
Available from: https://www.webfepafem-pafams.org/wp-content/uploads/2023/01/WFME-Standards-for-PGME-2023.pdf. Accessed 28 Aug 2023.
19. Stalmeijer RE, Whittingham JR, Bendermacher GW, Wolfhagen IH, Dolmans DH, Sehlbach C. Continuous enhancement of educational quality—fostering a quality culture: AMEE Guide No. 147. Med Teach 2023;45:6-16. Crossref
20. Dolmans DH, Wolfhagen HA, Scherpbier AJ. From quality assurance to total quality management: how can quality assurance result in continuous improvement in health professions education? Educ Health (Abingdon) 2003;16:210-7. Crossref