Hong Kong Med J 2023 Oct;29(5):412–20 | Epub 5 Oct 2023
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Telemedicine acceptance by older adults in Hong Kong during a hypothetical severe outbreak and after the COVID-19 pandemic: a cross-sectional cohort survey
Maxwell CY Choi1; SH Chu, MB, ChB1; LL Siu1; Anakin Gajy Tse, MB, ChB1; Justin CY Wu, MD, FRCP2,3; H Fung, MB, BS, FHKAM (Community Medicine)3,4; Billy CF Chiu, MB, BS, MPH3; Vincent CT Mok, MD, FRCP5
1 Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong SAR, China
2 Division of Gastroenterology and Hepatology, Department of Medicine and Therapeutics, Prince of Wales Hospital, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong SAR, China
3 CUHK Medical Centre, Hong Kong SAR, China
4 The Jockey Club School of Public Health and Primary Care, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong SAR, China
5 Division of Neurology, Department of Medicine and Therapeutics, Prince of Wales Hospital, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong SAR, China
Corresponding author: Prof Vincent CT Mok (vctmok@cuhk.edu.hk)
Abstract
Introduction: Telemedicine services worldwide
have experienced unprecedented growth since
the early days of the coronavirus disease 2019
(COVID-19) pandemic. Multiple studies have
shown that telemedicine is an effective alternative
to conventional in-person patient care. This study
explored the public perception of telemedicine in
Hong Kong, specifically among older adults who are
most vulnerable to COVID-19.
Methods: Medical students from The Chinese
University of Hong Kong conducted in-person
surveys of older adults aged ≥60 years. Each survey
collected socio-demographic information, medical
history, and concerns regarding telemedicine use.
Univariate and multivariate logistic regression
analyses were conducted to identify statistically
significant associations. The primary outcomes were
acceptance of telemedicine use during a hypothetical
severe outbreak and after the COVID-19 pandemic.
Results: There were 109 survey respondents.
Multivariate logistic regression analyses revealed
that the expectation of government subsidies for
telemedicine services was the strongest common
driver and the only positive independent predictor
of telemedicine use during a hypothetical severe
outbreak (P=0.016) and after the COVID-19
pandemic (P=0.003). No negative independent
predictors of telemedicine use during a hypothetical
severe outbreak were identified. Negative
independent predictors of telemedicine use after
the COVID-19 pandemic included older age and residence in the New Territories (both P=0.001).
Conclusions: Government support, such as
telemedicine-specific subsidies, will be important for
efforts to promote telemedicine use in Hong Kong
during future severe outbreaks and after the COVID-19 pandemic. Robust dissemination of information
regarding the advantages and disadvantages of
telemedicine for the public, especially older adults,
is needed.
New knowledge added by this study
- Older age and residence in the New Territories were negative predictors of telemedicine use during a hypothetical severe outbreak and after the coronavirus disease 2019 (COVID-19) pandemic.
- The expectation of government support (eg, subsidies) is a positive predictor of telemedicine use during a hypothetical severe outbreak and after the COVID-19 pandemic.
- Telemedicine carries minimal risk of disease transmission and may serve as a powerful addition to conventional in-person consultation, but it will not completely replace conventional consultation methods.
- Government support, such as telemedicine-specific subsidies and public education, will help encourage telemedicine use in Hong Kong.
Introduction
In 2020, the coronavirus disease 2019 (COVID-19)
pandemic caused many healthcare services
worldwide to experience a decline in patient
numbers because of cancellations related to a fear of
disease transmission.1 This decline led to increasing
interest in the expansion of telemedicine services
(ie, the practice of medicine over a distance through
telecommunication systems2) as a potential solution
to address gaps in healthcare delivery and minimise
the risk of COVID-19 transmission.3
Despite the availability of numerous virtual
technological solutions, Hong Kong has not
experienced significant progress towards the
widespread implementation and promotion of
telemedicine.4 Therefore, exploration of the factors
contributing to the relative underutilisation of
telemedicine by older adults in Hong Kong will
help to identify current limitations of the healthcare
system, while facilitating future implementation of
telemedicine.
The primary objectives of this study were
to examine the main concerns that older adults
have towards telemedicine and then evaluate
telemedicine use in two hypothetical scenarios:
during a severe outbreak while under lockdown, and after the COVID-19 pandemic. In this study,
‘severe outbreak’ was defined as a sudden increase in
disease frequency within a limited geographic area,
which requires public health interventions (eg, a
government-imposed lockdown involving temporary
restrictions on travel and social interactions, along
with quarantine measures)5; ‘after the COVID-19
pandemic’ was defined as the expected new norm
(ie, endemic COVID-19 requiring regular vaccines,
with societal adaptation to seasonal deaths and
complications in the absence of lockdowns, masks,
or social distancing).6
This study specifically explored perception of
telemedicine among older adults because they have
the highest risk of severe COVID-197 8 and may
experience the greatest benefit from telemedicine
use.
Methods
Study design and participants
This study consisted of an online survey completed
by a cohort of older adults in Hong Kong. The survey
was conducted from 8 October to 15 November
2020, between the third and fourth waves of
COVID-19 in the city.9 10 Medical student volunteers
from The Chinese University of Hong Kong were
recruited to facilitate data collection from older
adults in their families. Considering the overall need
for social distancing, we assumed that random in-person
visits to older adults carried a high risk of
disease transmission.11 Therefore, we chose to survey
close relatives of medical students living in the same
household; this approach was expected to reduce the
risk of disease transmission among medical students
and participants.11
In total, 59 medical student volunteers
were recruited in September 2020. To ensure
standardisation of the survey protocol, a mandatory
virtual training course was conducted via Zoom
on 28 September 2020, which included a detailed
written survey guide to help the volunteers to
facilitate the survey.
This study adhered to the STROBE
(Strengthening the Reporting of Observational
Studies in Epidemiology) guidelines.
Procedures
The survey targeted older adults (aged ≥60 years) in
Hong Kong. The closest caretakers were allowed to
complete the survey on behalf of older adults who
had health-related difficulty expressing themselves.12
This completion-by-proxy approach was used
because such caretakers regularly accompany older
adults to medical appointments and are likely to
have a good overall understanding of those older
adults’ healthcare needs. The survey was completed and submitted online; consent was obtained from
each participant before the start of the survey, and all
surveys were facilitated by trained medical student
volunteers.
The survey consisted of multiple-choice
questions that addressed five factors with important
effects on the perception of telemedicine among
older adults: (1) socio-demographic characteristics,
including age, gender, education level, number of
cohabitants in the same household, employment
status, and residential area; (2) medical history,
including types of chronic illnesses, frequency and
difficulty of visiting regular doctors in public and
private sectors, numbers and types of prescribed
medications, and private health insurance enrolment
status; (3) domestic support for telemedicine use,
including digital device availability and internet
access; (4) acceptance of telemedicine use in
two scenarios (ie, during a hypothetical severe
outbreak and after the COVID-19 pandemic); and
(5) telemedicine-associated values, concerns, and
expectations (eg, concerns about effectiveness and
satisfaction). With respect to the acceptance of
telemedicine use in two scenarios, respondents were
informed that telemedicine is mainly used during
follow-up for chronic medical conditions or when
visiting a doctor who is familiar with the patient
and their medical history; it is rarely used to visit
an unfamiliar doctor for a new or acute medical
condition.
Statistical analysis
Data analysis was performed using SPSS (Windows
version 26.0; IBM Corp, Armonk [NY], United
States). The cohort survey responses were first
thematically classified into four main categories,
namely demographics, home characteristics, medical
history, and telemedicine-related factors. The two
main primary outcome variables in our study were
dichotomous variables concerning acceptance of
telemedicine use: during a hypothetical severe
outbreak and after the COVID-19 pandemic.
Univariate logistic regression analysis was
conducted to identify predictors of telemedicine
use during a hypothetical severe outbreak and after
the COVID-19 pandemic, respectively. Multivariate
logistic regression analysis was performed using
variables that were statistically significant in
univariate analysis. To avoid variable overfitting, for
acceptance of telemedicine use during a hypothetical
severe outbreak, only variables with P values <0.05
in univariate analysis were included in multivariate
analysis; for acceptance of telemedicine use after
the pandemic, only variables with P values <0.01
in univariate analysis were included in multivariate
analysis. Continuous data were reported as mean ±
standard deviation.
Results
Cohort characteristics
Of the 109 respondents surveyed by 59 medical
student volunteers, 93.6% were older adults, whereas
6.4% were caretakers who completed the survey on
behalf of an older adult they cared for. The detailed
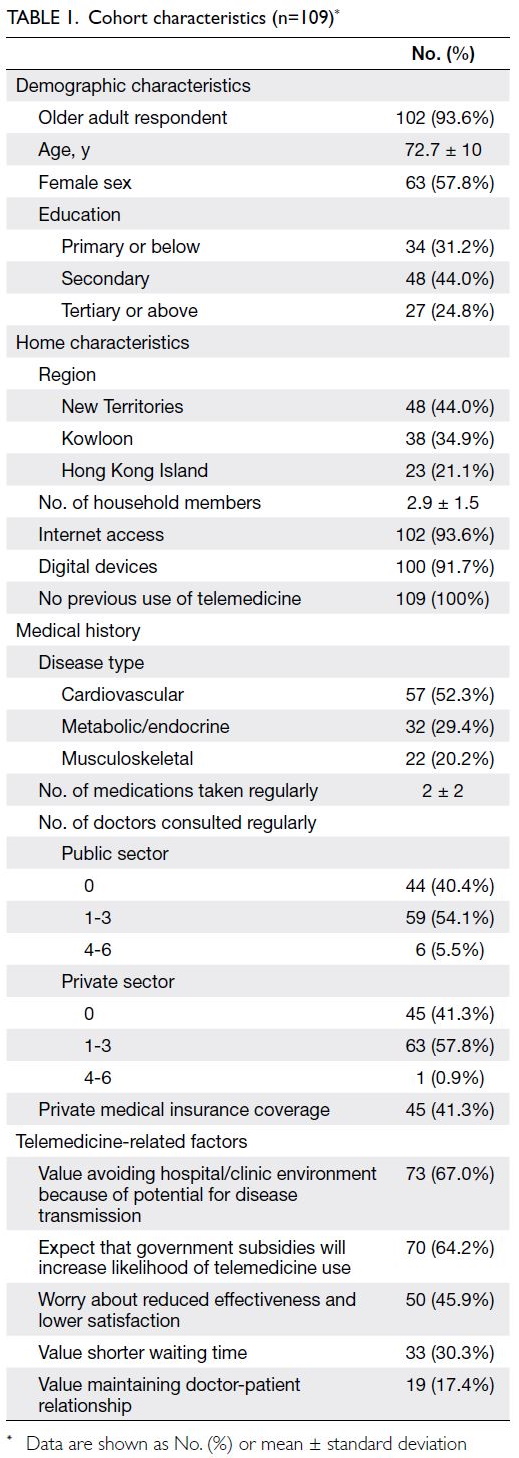
characteristics of the cohort are shown in Table 1.
The mean respondent age was 72.7 ± 10 years; most
respondents were women (57.8%) and had at least
completed secondary education (68.8%). In terms of
household characteristics, 44.0% of the respondents
lived in the New Territories and the mean size of each
household was 2.9 ± 1.5 members. Although most
respondents had access to both the internet (93.6%)
and digital devices (91.7%), none had previously
used telemedicine; thus, they were unable to indicate
which type of telemedicine they would prefer.
The survey also collected detailed information
about the respondents’ medical histories. In
terms of disease epidemiology, the most common
chronic disease types were cardiovascular (52.3%),
metabolic/endocrine (29.4%), and musculoskeletal
(20.2%); the mean number of medications taken
was 2 ± 2. Most respondents regularly consulted
one to three doctors in both the public (54.1%) and
private sectors (57.8%), but fewer than half of the
respondents had private medical insurance coverage
(41.3%). In terms of telemedicine, most respondents
valued avoiding hospital or clinic environments
because of the potential for disease transmission
(67.0%); they also expected that government
subsidies13 would increase their likelihood of using
telemedicine (64.2%).
Furthermore, nearly half of the respondents
worried that telemedicine use would lead to
reduced effectiveness and lower satisfaction (45.9%);
however, fewer than half of the respondents valued
maintaining the doctor-patient relationship (17.4%)
or reducing waiting time (30.3%).
Stratification of survey data according to
acceptance of telemedicine use revealed that 89
respondents (81.7%) would accept telemedicine
during a hypothetical severe outbreak; after the
COVID-19 pandemic, 43 respondents (39.4%)
would accept telemedicine. The characteristics
of respondents who would and would not accept
telemedicine during a hypothetical severe outbreak
and after the pandemic are presented in the online supplementary Appendix.
Factors affecting telemedicine use during a
hypothetical severe outbreak
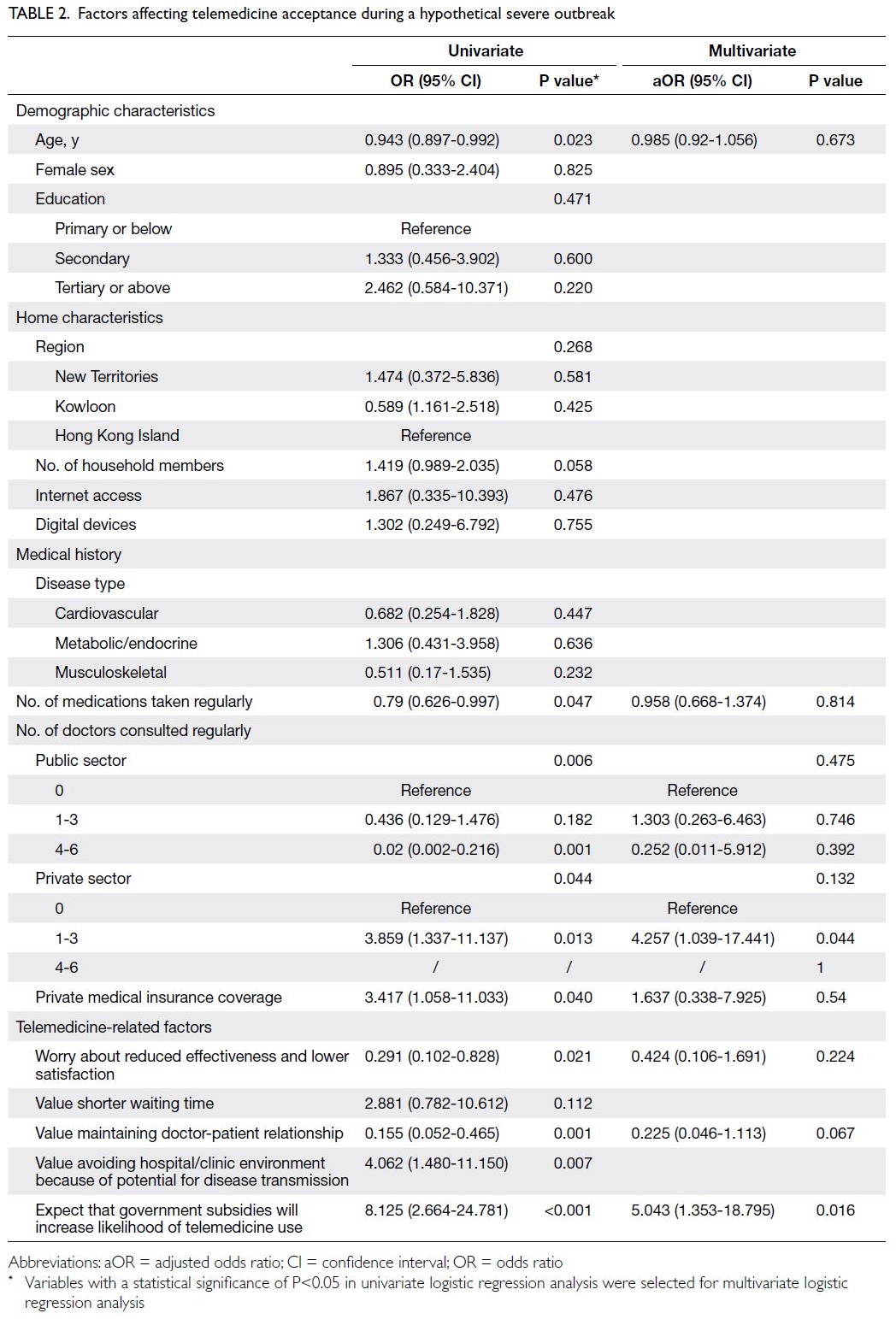
Multivariate logistic regression analysis (Table 2)
showed that the expectation of government subsidies
for telemedicine services was the only positive
independent predictor of telemedicine use during a hypothetical severe outbreak (adjusted odds ratio
[aOR]=5.043, 95% confidence interval [CI]=1.353-18.795; P=0.016). No negative independent predictors of telemedicine use during a hypothetical severe outbreak were identified.
Factors affecting telemedicine use after the
coronavirus disease 2019 pandemic
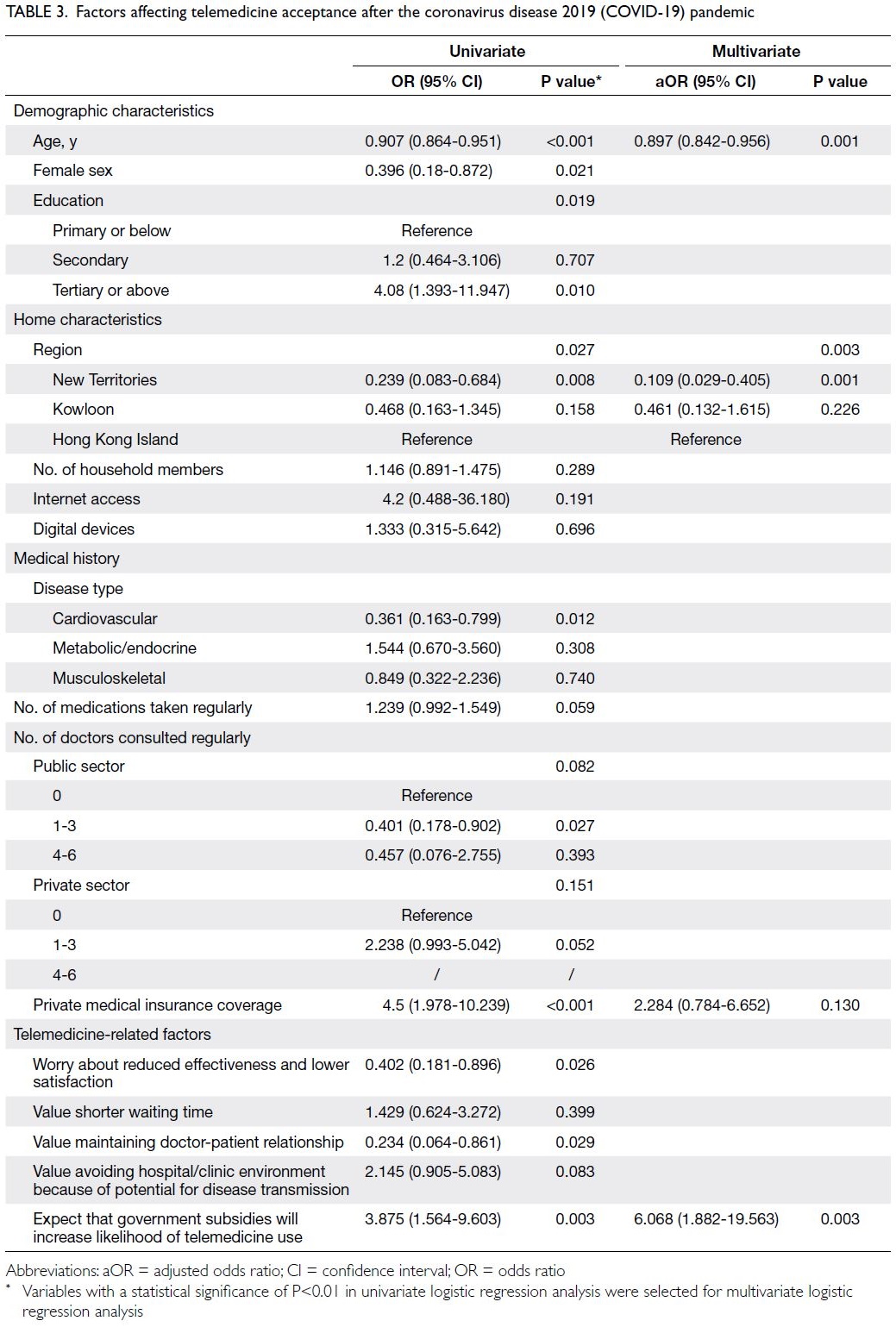
Multivariate logistic regression analysis (Table 3)
showed that the expectation of government subsidies
for telemedicine services was the strongest common
driver and the only positive independent predictor
of telemedicine use after the pandemic (aOR=6.068,
95% CI=1.882-19.563; P=0.003). However, there were
two negative independent predictors of telemedicine
use after the pandemic: older age (aOR=0.897,
95% CI=0.842-0.956; P=0.001) and residence in the
New Territories rather than on Hong Kong Island
(aOR=0.109, 95% CI=0.029-0.405; P=0.001).
Discussion
Interpretation of results
In this study, multivariate logistic regression analysis
revealed no negative independent predictors of
reduced telemedicine use during a hypothetical
severe outbreak. This result may be explained by the
fear of COVID-19 within the Hong Kong population,
which has prompted citizens to avoid public
transport and practise social distancing.14 Because
many Hong Kong citizens experienced the severe
acute respiratory syndrome epidemic in March 2003,
they remain fearful of unknown infectious diseases.15
Considering that telemedicine carries minimal risk
of disease transmission compared with conventional
in-person consultation,16 it is clearly valuable in
epidemic and pandemic scenarios; however, studies
thus far have shown that telemedicine is less effective
than hands-on procedures (eg, physical examination
or postoperative care).17 Nonetheless, rapid
technological advancements may soon overcome
these limitations. Therefore, it is reasonable to infer
that the characteristics and benefits of telemedicine
outweigh its limitations during severe outbreaks,
including epidemic and pandemic scenarios.
In both ‘severe outbreak’ and ‘after COVID-19
pandemic’ scenarios, the expectation of government
subsidies for telemedicine services was the strongest
common driver of telemedicine use; it was also the
only statistically significant positive independent
predictor of telemedicine use after the COVID-19
pandemic. For example, the Elderly Health Care
Voucher Scheme launched in Hong Kong in 2009
was intended to provide financial incentives for older
adults to seek healthcare services in the private sector,
thereby alleviating strain within the public healthcare
system. Thus far, this scheme has contributed
to positive uptake of telemedicine in the private
sector.13 Therefore, to encourage use of telemedicine
services during the pandemic, we propose extending
telemedicine-specific subsidies to older adults.
Furthermore, the role of government support
in promoting telemedicine use should be emphasised
and expanded. For example, Hong Kong’s older
adults could receive subsidies to purchase essential
digital devices for telemedicine consultations, such
as webcams and remote monitoring devices. Indeed,
a study in Australia showed that government support
for healthcare, such as the reduction of insurance
reimbursement restrictions, has been a key factor
in the country’s increased use of telemedicine.18
Moreover, public education regarding telemedicine
and digital health overall should be conducted
to address patient misconceptions and clarify
expectations regarding telemedicine. It is important
to emphasise that the use of telemedicine does
not imply that patients should discontinue follow-up.
Further education concerning the format (eg,
video calls and use of digital health applications),
effectiveness (ie, limited physical examination),
and other aspects of telemedicine is strongly
recommended because these were the most
important concerns among the respondents in the
current study.
There were two statistically significant negative
independent predictors of telemedicine use after
the COVID-19 pandemic: older age and residence
in the New Territories. For older adults, a lack of
technological competency is an important challenge
when adapting to a new mode of consultation. Older
adults often struggle with unfamiliar technology,
which may ultimately prevent many of them
from using telemedicine. To help older adults
adopt new technologies, telemedicine systems
should be designed with the goal of maximum
user-friendliness.19 For example, easy-to-navigate
interfaces and simple instructions with larger display
fonts may help increase older adults’ willingness to
use telemedicine for chronic illness follow-up after
the COVID-19 pandemic.
With respect to older adults who live in the
New Territories, a relatively more rural part of
Hong Kong, the digital infrastructure necessary to
provide telemedicine services may be less robust
than the infrastructure on Hong Kong Island and in
Kowloon. Indeed, the New Territories has the largest
number of high-poverty areas in Hong Kong, which
may be associated with low socio-economic status
and limited education leading to lower healthcare
utilisation.20 Poverty also has an effect on hospital
access, such that the New Territories generally
displays the least hospital access among all regions
of Hong Kong; however, considering the long travel
distances to hospitals and clinics, telemedicine
may be very beneficial for residents in this region.20
Overall, telemedicine accessibility in Hong Kong
remains a major concern that requires further
investigation.
Strengths
To our knowledge, this is the first study in Hong
Kong to comprehensively examine concerns about
telemedicine implementation among older adults,
both during a hypothetical severe outbreak and after
the COVID-19 pandemic. The use of telemedicine as
a novel approach to patient consultations may serve
as an important component of an effective geriatric
healthcare system during the pandemic and could
even be implemented as a powerful addition to in-person
consultation during clinical practice after the
pandemic.21
Additionally, the mandatory training course for
medical student volunteers and detailed explanation
of each question ensured adequate quality control, as
well as a full understanding of telemedicine, during
the completion of each survey. The training course
also ensured uniformity during survey delivery,
thereby minimising the potential for confirmation or
observer bias that could arise from unstandardised
survey delivery styles among different volunteers. A
survey guide was explicitly introduced in the training
course; it included a detailed rationale of the study
as well as key points to consider with each survey
question.
Limitations
Because the survey only included the responses of
family members of medical students, selection and
inter-observer biases were possible. However, these
biases were counterbalanced by the comprehensive
training course to achieve uniformity during survey
delivery. Retrospective analysis of the study results
did not suggest that the respondents favoured
telemedicine; thus, we concluded that the potential
for selection bias was negligible.
This study also had a relatively small sample size
because of pandemic-associated social distancing
restrictions. For example, the cohort did not involve
citizens residing on the outlying islands of Hong
Kong. These areas, with their remote locations and
limited hospital access,20 may have a greater need
for telemedicine. Therefore, caution is needed when
generalising our findings to populations outside of
Hong Kong. Furthermore, this study was performed
before the formal introduction of a COVID-19
vaccination programme, which has been shown to
greatly influence the attitude of the general public
towards health-seeking behaviours.22 Therefore, this
study may not be fully representative of the current
pandemic situation in Hong Kong.
Future studies
This study primarily focused on older adults.
Future studies should investigate the acceptance of
telemedicine among younger adults (aged <60 years), adolescents, and children. Future studies could also
compare the perspectives of caretakers and older
adults themselves on a larger scale to determine
whether concerns differ among stakeholders.
Conclusion
This study examined concerns among older adults
regarding the use of telemedicine, both during a
hypothetical severe outbreak while under lockdown,
and after the COVID-19 pandemic. The findings
indicated that government support was a key driver
of telemedicine use in Hong Kong under both
scenarios. After the pandemic, telemedicine-specific
subsidies and public education will be essential for
efforts to overcome telemedicine hesitancy that
arises from technological inconveniences related to
age and geographic location.
In the future, government support via
telemedicine-specific subsidies will be a key driver of
telemedicine use in Hong Kong, both during a severe
outbreak and after the COVID-19 pandemic. The
continued use of telemedicine after the pandemic
requires telemedicine systems that are designed
to ensure maximal age-friendliness. However,
telemedicine should be used in combination with
conventional in-person consultation rather than as
a replacement for such consultation.
Author contributions
Concept or design: JCY Wu, H Fung, BCF Chiu, VCT Mok.
Acquisition of data: MCY Choi, SH Chu, LL Siu, AG Tse.
Analysis or interpretation of data: MCY Choi, SH Chu, LL Siu, AG Tse.
Drafting of the manuscript: MCY Choi, SH Chu, LL Siu, AG Tse, VCT Mok.
Critical revision of the manuscript for important intellectual content: MCY Choi.
Acquisition of data: MCY Choi, SH Chu, LL Siu, AG Tse.
Analysis or interpretation of data: MCY Choi, SH Chu, LL Siu, AG Tse.
Drafting of the manuscript: MCY Choi, SH Chu, LL Siu, AG Tse, VCT Mok.
Critical revision of the manuscript for important intellectual content: MCY Choi.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
The authors thank Mr Brian Yiu from the Division of
Neurology, Department of Medicine and Therapeutics, The
Chinese University of Hong Kong for aid with statistical
analysis. The authors also thank all medical student volunteers
from The Chinese University of Hong Kong for assisting with
in-person surveys.
Declaration
This work was posted on medRxiv as a registered online preprint (https://www.medrxiv.org/content/10.1101/2021.07.15.21260346v1).
Funding/support
This research received no specific grant from any funding
agency in the public, commercial, or not-for-profit sectors.
Ethics approval
Ethics approval for the study protocol was obtained from
the Joint Chinese University of Hong Kong–New Territories
East Cluster Clinical Research Ethics Committee (Ref No.:
2020.536). This research was performed in accordance with
the Declaration of Helsinki and consent was obtained from
each participant before the start of the survey.
References
1. Wong SY, Zhang D, Sit RW, et al. Impact of COVID-19
on loneliness, mental health, and health service
utilisation: a prospective cohort study of older adults
with multimorbidity in primary care. Br J Gen Pract
2020;70:e817-24. Crossref
2. World Medical Association. WMA statement on the
ethics of telemedicine. 2018. Available from: https://www.wma.net/policies-post/wma-statement-on-the-ethics-of-telemedicine/. Accessed 6 Apr 2021.
3. Lau C. Telemedicine in the time of COVID-19 and beyond.
MIMS Respirology. 2020. Available from: https://specialty.mims.com/topic/telemedicine-in-the-time-of-covid-19-and-beyond. Accessed 16 Jun 2021.
4. Legislative Council, Hong Kong SAR Government.
Development of telehealth services. ISE14/20-21. 2020.
Available from: https://www.legco.gov.hk/research-publications/
english/essentials-2021ise14-development-of-telehealth-services.htm. Accessed 6 Apr 2021.
5. Reintjes R, Zanuzdana A. Outbreak investigations. In: Krämer A, Kretzschmar M, Krickeberg K, editors. Modern Infectious Disease Epidemiology. New York: Springer; 2010: 159-76. Crossref
6. Phillips N. The coronavirus is here to stay—here’s what that
means. Nature 2021;590:382-4. Crossref
7. Mok VC, Pendlebury S, Wong A, et al. Tackling challenges
in care of Alzheimer’s disease and other dementias amid the
COVID-19 pandemic, now and in the future. Alzheimers
Dement 2020;16:1571-81. Crossref
8. Centers for Disease Control and Prevention, United States
Government. COVID-19 risks and information for older
adults. 2023. Available from: https://www.cdc.gov/aging/covid19/index.html#:~:text=Older%20adults%20are%20more%20likely,very%20sick%20from%20COVID%2D19 .
Accessed 25 Sep 2023.
9. Wong MC, Wong EL, Huang J, et al. Acceptance of the
COVID-19 vaccine based on the health belief model:
a population-based survey in Hong Kong. Vaccine
2021;39:1148-56. Crossref
10. Chan WM, Ip JD, Chu AW, et al. Phylogenomic analysis
of COVID-19 summer and winter outbreaks in Hong
Kong: an observational study. Lancet Reg Health West Pac
2021;10:100130. Crossref
11. Chauhan V, Galwankar S, Arquilla B, et al. Novel
coronavirus (COVID-19): leveraging telemedicine to
optimize care while minimizing exposures and viral
transmission. J Emerg Trauma Shock 2020;13:20-4. Crossref
12. Reinhard SC, Given B, Petlick NH, Bemis A. Supporting
family caregivers in providing care. In: Hughes RG, editor.
Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008: 341-404.
13. Yam CH, Wong EL, Fung VL, Griffiths SM, Yeoh EK. What
is the long term impact of voucher scheme on primary
care? Findings from a repeated cross sectional study
using propensity score matching. BMC Health Serv Res
2019;19:875. Crossref
14. Sit SM, Lam TH, Lai AY, Wong BY, Wang MP, Ho SY. Fear
of COVID-19 and its associations with perceived personal
and family benefits and harms in Hong Kong. Transl Behav
Med 2021;11:793-801. Crossref
15. Choi EP, Hui BP, Wan EY. Depression and anxiety in Hong
Kong during COVID-19. Int J Environ Res Public Health
2020;17:3740. Crossref
16. Kadir MA. Role of telemedicine in healthcare during
COVID-19 pandemic in developing countries. Telehealth
Med 2020;5:1-5. Crossref
17. Williams AM, Bhatti UF, Alam HB, Nikolian VC. The role
of telemedicine in postoperative care. Mhealth 2018;4:11. Crossref
18. Thomas EE, Haydon HM, Mehrotra A, et al. Building on
the momentum: sustaining telehealth beyond COVID-19. J
Telemed Telecare 2022;28:301-8. Crossref
19. Narasimha S, Madathil KC, Agnisarman S, et al. Designing
telemedicine systems for geriatric patients: a review of the
usability studies. Telemed J E Health 2017;23:459-72. Crossref
20. Guo Y, Chang SS, Sha F, Yip PS. Poverty concentration
in an affluent city: geographic variation and correlates
of neighborhood poverty rates in Hong Kong. PLoS One
2018;13:e0190566. Crossref
21. Grossman Z, Chodick G, Reingold SM, Chapnick G,
Ashkenazi S. The future of telemedicine visits after
COVID-19: perceptions of primary care pediatricians. Isr J
Health Policy Res 2020;9:53. Crossref
22. Wang K, Wong EL, Ho KF, et al. Change of willingness to
accept COVID-19 vaccine and reasons of vaccine hesitancy
of working people at different waves of local epidemic
in Hong Kong, China: repeated cross-sectional surveys.
Vaccines (Basel) 2021;9:62. Crossref