Hong Kong Med J 2023 Oct;29(5):404–11 | Epub 12 Oct 2023
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
User perceptions of COVID-19 telemedicine testing services, disease risk, and pandemic preparedness: findings from a private clinic in Hong Kong
Kevin KC Hung, FHKCEM, FHKAM (Emergency Medicine)1,2,3; Emily YY Chan, MD1,2,3,4; Eugene SK Lo, MPH2,3; Zhe Huang, MPH2,3; Justin CY Wu, MD3,5; Colin Alexander Graham, MD1,2,3
1 Accident and Emergency Medicine Academic Unit, The Chinese University of Hong Kong, Hong Kong SAR, China
2 Collaborating Centre for Oxford University and CUHK for Disaster and
Medical Humanitarian Response, The Chinese University of Hong Kong,
Hong Kong SAR, China
3 Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong SAR, China
4 Nuffield Department of Medicine, University of Oxford, Oxford, United Kingdom
5 CUHK Medical Centre, Hong Kong SAR, China
Corresponding author: Prof Emily YY Chan (emily.chan@cuhk.edu.hk)
Abstract
Introduction: During the coronavirus disease 2019
(COVID-19) pandemic, telemedicine has been
regarded as a method for providing safe access to
healthcare. Here, we explored the experiences of
individuals using telemedicine in Hong Kong during
the COVID-19 pandemic to understand their risk
perceptions and preparedness measures.
Methods: We conducted a cross-sectional online
survey of telemedicine users of private clinic–based COVID-19 testing services from 6 April to
11 May 2020. All users were invited to complete an
anonymous online survey regarding COVID-19 risk
perception and preparedness measures. The results
of the survey were compared with the findings of a
previous territory-wide survey.
Results: In total, 141 of 187 telemedicine users
agreed to participate; the response rate was 75.4%.
Of the participants, 95.1% (116/122) believed that
telemedicine consultations were useful. Nearly half
of the participants (49.0%) agreed or strongly agreed
that telemedicine consultations were appropriate
during the COVID-19 pandemic. Most participants
believed that telemedicine consultations could
perform the functions of ‘health protection,
promotion and disease prevention’ (73.6%) and
‘diagnosis’ (64.0%). Concerning the choice of
telemedicine provider, almost all participants (99.2%) were willing to consult medical doctors;
more than half of the participants (54.1%) were
willing to consult registered nurses, but only 13.1%
were willing to consult non-clinical staff who had
been trained to provide telemedicine services.
Conclusions: The use of telemedicine for screening
and patient education can be encouraged during the
COVID-19 pandemic in Hong Kong.
New knowledge added by this study
- Telemedicine use in Hong Kong was limited before the pandemic, but telemedicine users had high satisfaction with coronavirus disease 2019 (COVID-19) testing services.
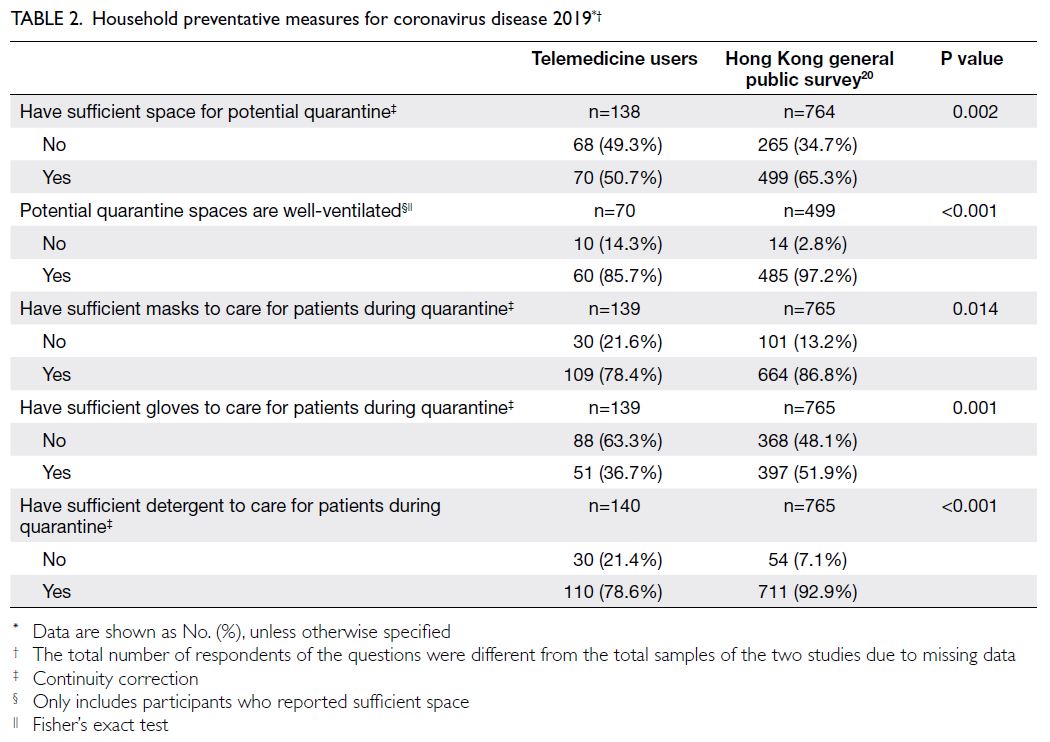
- Most participants believed that the telemedicine consultations could perform the functions of ‘health protection, promotion and disease prevention’ and ‘diagnosis’.
- Among telemedicine users, the preferred channels of infectious disease information were the internet or mobile applications as well as personal sources (eg, family, friends, or healthcare professionals).
- Telemedicine users in this study were relatively young; previous reports suggest that these users are less likely to use healthcare in the absence of telemedicine and less likely to have a follow-up visit in any setting, compared with patients who visit a clinic for a similar condition. The use of telemedicine services might provide opportunities for healthcare access that are not otherwise available.
- Additional training for telemedicine providers might be needed to improve the quality and scope of telemedicine services.
- The use of telemedicine for screening and patient education can be encouraged during the COVID-19 pandemic in Hong Kong and elsewhere.
Introduction
In the early days of the coronavirus disease
2019 (COVID-19) pandemic, telemedicine was
recommended as a solution to provide safe
access to healthcare.1 In 2020, the World Health
Organization reported that most global health
authorities regarded telemedicine as a potential
method to provide services for patients with
non-communicable diseases.2 For example, in a
national survey of healthcare providers in Germany,
approximately 60% of participants reported routine
or partial use of telemedicine during the COVID-19
pandemic.3 In the US in 2020, telemedicine was used
for COVID-19 screening, monitoring of patients
with positive COVID-19 test results, management of
chronic diseases, and virtual monitoring and follow-up.4 Telemedicine reduces patient travel costs and
improves access, while reducing the use of personal
protective equipment and the risk of COVID-19
transmission. In China, ‘internet hospitals’ offered
essential medical support to the public during the
early days of the COVID-19 pandemic.5
However, from a patient perspective, there are
limitations and barriers to the use of telemedicine. A
qualitative study conducted in Hong Kong in 20166
revealed that patient concerns included technical
and logistical issues (eg, difficulty in accessing and
using computers), limited personal interactions (eg, lack of in-person physical examinations and risk of
incorrect diagnosis related to poor communication),
concerns regarding cybersecurity and safety, and
problems with prescriptions (eg, distrust of local
community pharmacies). In 2020, clinical guidelines
were published concerning the performance of
remote primary care assessments and treatments
for patients with suspected COVID-19 in the United
Kingdom.7 During the COVID-19 pandemic, a
digital health ecosystem may benefit the healthcare
system, as well as the broader population (eg,
through tracking and communication strategies) and
research and health technology sectors (eg, online
activity monitoring and digital support for isolation
and quarantine situations).8
Telemedicine consists of remote healthcare
service delivery by healthcare professionals for
diagnosis, treatment, and prevention efforts, as
well as research and continuing education.9 The
fundamental goal of telemedicine is to increase
access to care, thereby serving populations that
otherwise would not receive timely medical
evaluation and treatment. Research concerning
telemedicine effectiveness has been controversial.10 11 12 13 14
A previous systematic review found that many
studies showed no difference between telemedicine
and usual care, and there remains limited evidence
concerning the cost-effectiveness of telemedicine.10
With respect to chronic disease management via
telemedicine, another review found publication
bias and a tendency to report only short-term
outcomes.11 Moreover, a Cochrane review revealed
improved control of blood glucose among patients
with diabetes using telemedicine, compared with
patients receiving in-person care; conversely, the
care modality did not affect health outcomes among
patients with heart failure.12 Regarding the impacts
and costs of telemedicine services, economic
analyses have been problematic because of complex
and unpredictable collaborative achievement
processes13; generalisability has been limited by poor
quality and low reporting standards.14 There is a need
to focus on patient perspectives and telemedicine
innovations.
In 2020, the health system in Hong Kong
was considerably impacted by COVID-19
transmission risk and public health responses.15
During the early days of the COVID-19 pandemic,
the number of in-person medical consultations
decreased worldwide.16 17 In the Netherlands, the
use of telemedicine offset this decrease.17 Before
the COVID-19 pandemic, telemedicine was not
widely used in Hong Kong6 18; user perspectives
concerning the role of telemedicine during the
COVID-19 pandemic and future pandemics
require investigation. This study of telemedicine
users in Hong Kong explored their perceptions of
telemedicine use during the COVID-19 pandemic, their perceptions of disease risk, and their COVID-19
preparedness measures. We hypothesised that
telemedicine users have distinct perceptions of
risk, compared with the general public; we sought
to determine the effects of such differences on the
delivery of health services.
Methods
We conducted a cross-sectional online survey from 6
April to 11 May 2020. Participants in this study were
users of COVID-19 testing services provided by The
Chinese University of Hong Kong (CUHK) Medical
Clinic,19 a multispecialty clinic offering specialist
consultations, health screenings, vaccinations, and
COVID-19 testing services.
Testing services and recruitment procedure
All service users completed a telemedicine
consultation, followed by COVID-19 testing. The
consultation, delivered using a standard telephone,
focused on assessment of the user’s COVID-19 risk
prior to the time of testing. Users were offered a deep
throat saliva test for COVID-19 detection. After the
telemedicine consultation and COVID-19 test, all
users were invited to complete an anonymous online
survey within 1 month for service evaluation and
data collection.
Survey design
The online survey consisted of 24 questions
regarding telemedicine services, COVID-19 risk
perception, and preparedness measures in Hong
Kong. The survey specifically focused on reasons for
using CUHK telemedicine and testing services, user
perceptions and attitudes regarding telemedicine
consultations, user perceptions and attitudes
regarding the COVID-19 pandemic and prevention,
and user characteristics (eg, age and sex). Questions
about user perceptions and attitudes regarding the
current COVID-19 pandemic and prevention were
phrased in a manner identical to a previous study,20
allowing direct comparison with survey results
from a study focused on the Hong Kong general
public. The survey was pilot tested and subsequently
modified to ensure content validity. Most questions
included ‘yes’ or ‘no’ answers and a 5-point Likert
scale. Written consent to take part in the study was
obtained from all participants before they began the
survey.
Statistical analysis
Descriptive statistics were reported for participant
characteristics, perceptions, and attitudes regarding
telemedicine consultations. Perceptions and
attitudes regarding the COVID-19 pandemic and
prevention were recorded in a manner that allowed
comparison with the results of a prior COVID-19–focused telephone survey of the Hong Kong general
public.20 The prior telephone survey—a cross-sectional,
population-based landline telephone
survey using a computerised random-digit dialling
method—included 765 adult Hong Kong residents
during the period from 22 March to 1 April 2020.
The participants in that study were representative
of Hong Kong Census population data with respect
to age, sex, marital status, and residential district,
although they had higher levels of education and
household income.20 Chi squared tests were used
for comparisons between the prior survey and
the present survey. The threshold of statistical
significance was set at 0.05. All statistical analyses
were conducted using SPSS (Windows version 21.0;
IBM Corp, Armonk [NY], US).
Results
Among 187 telemedicine users of COVID-19
testing services at the CUHK Medical Clinic, we
identified 150 responses to the online survey during
the period from 6 April to 11 May 2020. In total,
141 telemedicine users (response rate of 75.4%)
were willing to participate in this study. Table 1
shows the participants’ characteristics. Notably,
56.1% were men, over half (50.7%) were aged 18 to 24 years (all participants were aged <65 years),
most (59.4%) lived in private housing, and most
(65.4%) resided in the New Territories. The most
common reason for COVID-19 testing was a work-related
requirement (56.7%, 80/141), followed by
recent international travel (39.7%, 56/141); 14.9%
(21/141) of the participants sought testing because
of concerns about the spread of COVID-19. Overall,
14.2% (20/141) of the participants had either been
in close contact with a confirmed case or suspected
that they had symptoms of COVID-19.
Perceptions of telemedicine consultations
In total, 95.1% (116/122) participants believed
that COVID-19 telemedicine consultations were
useful. Most participants believed that telemedicine
consultations could perform the functions of ‘health
protection, promotion and disease prevention’
(73.6%) and ‘diagnosis’ (64.0%) [Fig 1]. Concerning
the choice of telemedicine provider, almost all
participants (99.2%) would accept medical doctors;
more than half of the participants (54.1%) would
accept trained nurses, but only 13.1% would accept
non-clinical staff who had been trained to provide
telemedicine services.
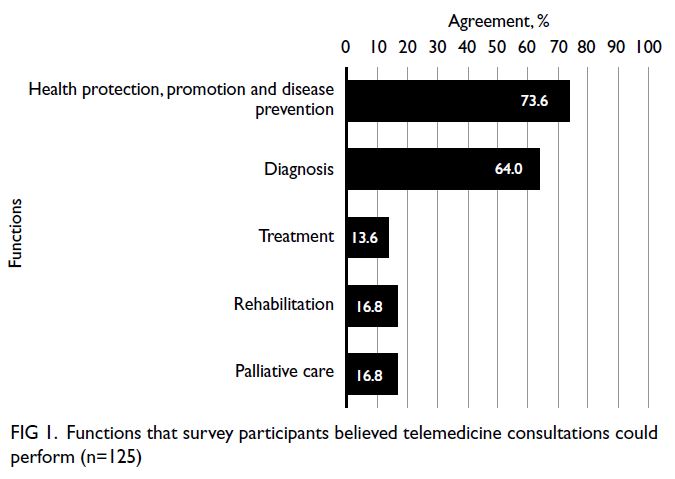
Figure 1. Functions that survey participants believed telemedicine consultations could perform (n=125)
Nearly half of the participants (49.0%) agreed or
strongly agreed that telemedicine consultations were
appropriate during the COVID-19 pandemic (Fig 2).
More than half (61.0%) of the participants reported
satisfaction with telemedicine consultations (‘agree’
or ‘strongly agree’) and services provided by clinic
staff (73.8% responded ‘agree’ or ‘strongly agree’).
However, only 36.2% agreed or strongly agreed that
service quality was identical between telemedicine
consultations and in-person consultations.
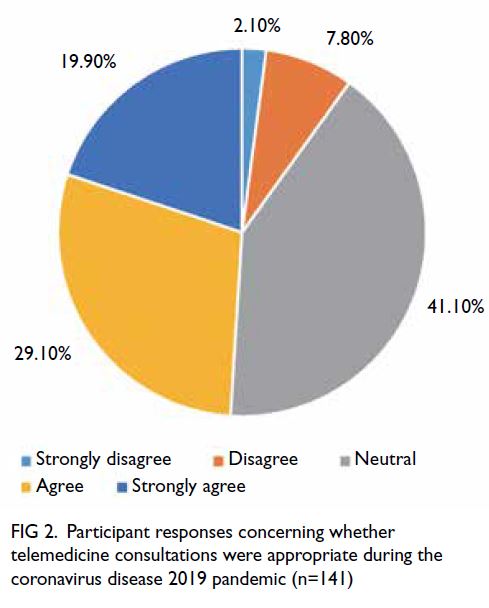
Figure 2. Participant responses concerning whether telemedicine consultations were appropriate during the coronavirus disease 2019 pandemic (n=141)
Household capacity for potential coronavirus
disease 2019–related quarantine
Household capacities for potential COVID-19—related quarantine were compared between
telemedicine users in this study and respondents
in the prior Hong Kong general public telephone
survey20 (Table 2). Telemedicine users reported
having less space at home, fewer masks, fewer
gloves, and less detergent for potential quarantine
situations, compared with respondents in the Hong
Kong general public telephone survey (all P<0.05).
In response to the question ‘How many
designated caregivers are appropriate for each
isolated/quarantined person?’, telemedicine users
were less likely to answer correctly (limit to one
main carer, 8.1%), compared with respondents in
the Hong Kong general public telephone survey
(51.3%)20 [P<0.001, Chi squared with continuity correction].
Perceptions of coronavirus disease 2019
preparedness
Most telemedicine users (76.4%) believed that
household prevention could prevent COVID-19;
approximately 67% of them believed that they had
sufficient knowledge to manage COVID-19—related
health risks. These percentages were higher than
the percentages in the Hong Kong general public
telephone survey20 (Table 3). Additionally, >80% of telemedicine users believed that Hong Kong had
achieved better control of COVID-19, compared
with other major cities.
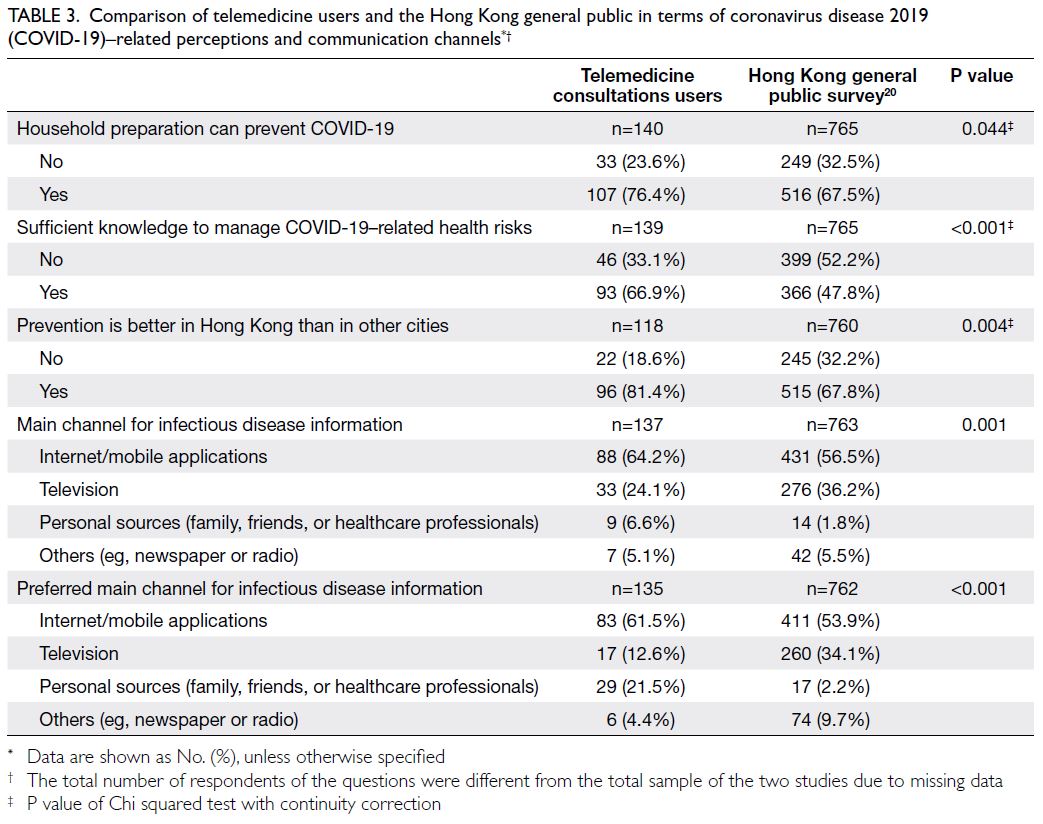
Table 3. Comparison of telemedicine users and the Hong Kong general public in terms of coronavirus disease 2019 (COVID-19)–related perceptions and communication channels
Regarding their main channel for infectious
disease information, approximately 64% of
participants were using the internet or mobile
applications, whereas 24% were using television;
these percentages differed from the Hong Kong
general public telephone survey, in which 56.5% of
respondents used the internet or mobile applications
and 36.2% used television20 (P<0.001). Overall,
telemedicine users preferred their main channel for
infectious disease information to be the internet or
mobile applications and personal sources (eg, family,
friends, or healthcare professionals).
Discussion
This study demonstrated high satisfaction with
telemedicine consultations among users and
revealed that users considered telemedicine to
be appropriate during the COVID-19 pandemic.
Despite the perception that telemedicine users
have sufficient knowledge to manage health risks
from COVID-19, when responses were compared
between telemedicine users and the Hong Kong
general public, we found that household preventative
measures were inadequate among telemedicine
users.
Acceptance of telemedicine
Most of our telemedicine users did not agree
that quality was identical between telemedicine
consultations and in-person consultations. This
perspective possibly resulted from the provision of
telemedicine consultations via telephone without
a video component; moreover, the users might not
have been familiar with the concept of telemedicine
consultation. Indeed, a 2014 nationwide survey in
the US revealed that only 15% of family physicians
reported using telemedicine in the previous
year; barriers included a lack of training, a lack of
reimbursement, the cost of equipment, and potential
liability issues.21 Furthermore, Schwamm22 has
described telemedicine as a disruptive technology
that may threaten traditional healthcare delivery.
Obstacles to the expansion of telemedicine in the US
include state-level statutes that require the clinician
to be located in the same state as the patient and to
have previously completed an in-person consultation
with that patient.23 Similar regulatory requirements exist in Hong Kong.24
Various studies in the US have detected
increasing uptake of telemedicine, particularly in
primary care.25 26 27 28 29 A study of telemedicine users in
a large commercially insured population in the US
from 2005 to 2017 showed that the mean age was
38.3 years; on average, users of primary care
telemedicine were younger than users of telemental
healthcare and more likely to reside in urban areas.25
A study regarding Teladoc, one of the largest telemedicine providers in the US, revealed that
Teladoc users were younger and less likely to have
used healthcare before the introduction of Teladoc;
they were also less likely to have a follow-up visit
in any setting, compared with patients who visited
a clinic for a similar condition.26 These findings
are consistent with our observations that most
telemedicine users were young; they also suggest
that the use of telemedicine services can provide
opportunities for healthcare access that are not
otherwise available.
Household preparations for coronavirus
disease 2019
Intriguingly, although more telemedicine users
agreed that household preparation could prevent
COVID-19, they were less likely to believe that their
household preventative measures were adequate,
compared with respondents in the Hong Kong
general public telephone survey.20 This disparity
may be attributed to differences in participant
characteristics: telemedicine users in this study were
younger (51% aged 18-24 years, vs 9% in the Hong
Kong general public20), were male (56% vs 47%20),
and were living in the New Territories (65% vs
51%20). Telemedicine users were also more likely to
use the internet (64% vs 57%20) as the main channel
for infectious disease information and to prefer
using the internet for such information (62% vs
54%20). These findings have important implications
for the use of telemedicine to fill gaps in health
promotion and disease prevention. Wu et al30 found
that secondary cases from household transmission
of COVID-19 were common in Zhuhai, China,
and one-third of these secondary cases were
asymptomatic. Sufficient household preparation
measures are needed to limit the spread of
COVID-19.31
Future use of telemedicine in Hong Kong
Telemedicine in Hong Kong had a ‘late start’ (in 1994);
in 1998, Hjelm32 predicted that the telemedicine would
be rapidly implemented in Hong Kong. However, in
the December 2019 version of the Ethical Guidelines
on Practice of Telemedicine by the Medical Council
of Hong Kong, it was noted that telemedicine in Hong
Kong has not fully developed.24 Despite the obvious
convenience benefit and reduced risk of COVID-19
transmission, the guidelines remind practitioners
that they remain fully responsible for legal and ethical
obligations during telemedicine consultations.24
Furthermore, the guidelines mention that standards
of care to protect patients are applicable during in-person
and telemedicine consultations; practitioners
should familiarise themselves with the World
Medical Association Statement on the Ethics of
Telemedicine.33
Training and patient assessment guidelines
for healthcare practitioners are urgently needed,
considering the unique circumstances surrounding
the use of telemedicine, such as technology (eg,
technical limitations of virtual consultations,
including assessments), patient education and
informed consent, cybersecurity, and other
concerns.6 These guidelines would ensure that the
same standards of telemedicine consultations can be
implemented, as described by the Medical Council
of Hong Kong.
Limitations
The present study focused on 141 telemedicine
users of a single private clinic providing deep
throat saliva polymerase chain reaction tests for
detection of severe acute respiratory syndrome
coronavirus 2; thus, the study participants may
not be representative of all telemedicine users in
Hong Kong. Responder bias may have affected the
results (the response rate was 75.4%), but it was not
possible to compare participants with individuals
who refused to participate. Furthermore, the recent
experience of a telemedicine consultation may
have biased participants’ responses in favour of
telemedicine.
Concerning the comparison of COVID-19
risk perception and preparedness measures,
methodological discrepancies between the online
survey of telemedicine users and the telephone
survey of the Hong Kong general public may have led
to differences in responses, particularly with respect
to including younger and more computer-literate
individuals in the online survey. Although the present
study was conducted from 6 April to 11 May 2020
(after a surge of COVID-19 cases in Hong Kong), the
Hong Kong general public telephone survey used
for comparison was conducted from 22 March to
1 April 2020 (during a surge in COVID-19 cases).20
The difference in data collection periods may have
contributed to different perceptions of COVID-19
preparedness. Various physical distancing measures
were implemented during the COVID-19 surge
(from late March to early April), which may also have
contributed to differences between the telephone
survey and online survey cohorts.
Finally, because of sample size limitations
and problems with representativeness, the findings
of the study may be restricted to understanding
views regarding telemedicine consultations among
participants in the present study. However, factors
such as young age, residence in private housing,
and residence in the New Territories may have
contributed to response bias; because no information
was collected concerning occupation, education
level, income, or ethnicity, we could not control for
bias related to these factors.
Conclusion
In this study, telemedicine users in Hong Kong
agreed that telemedicine consultations were
appropriate during the COVID-19 pandemic.
Participants agreed that telemedicine consultations
could perform the functions of health protection,
promotion, disease prevention, and diagnosis.
The use of telemedicine for screening and patient
education can be encouraged during the COVID-19
pandemic in Hong Kong.
Author contributions
Concept or design: KKC Hung, EYY Chan, JCY Wu.
Acquisition of data: KKC Hung, JCY Wu, CA Graham.
Analysis or interpretation of data: KKC Hung, EYY Chan, ESK Lo, Z Huang.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: KKC Hung.
Acquisition of data: KKC Hung, JCY Wu, CA Graham.
Analysis or interpretation of data: KKC Hung, EYY Chan, ESK Lo, Z Huang.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: KKC Hung.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This research did not receive any specific grant from funding
agencies in the public, commercial, or not-for-profit sectors.
Ethics approval
This research was approved by the Survey and Behavioural
Research Ethics Committee of The Chinese University of
Hong Kong (Ref No.: SBRE-19-730). Patients were treated
in accordance with the tenets of the Declaration of Helsinki
and provided written informed consent for all treatments and
procedures, as well as publication of their anonymised data.
References
1. Hollander JE, Carr BG. Virtually perfect? Telemedicine for
COVID-19. N Engl J Med 2020;382:1679-81. Crossref
2. World Health Organization. Rapid assessment of service
delivery for NCDs during the COVID-19 pandemic.
Available from: https://www.who.int/publications/m/item/rapid-assessment-of-service-delivery-for-ncds-during-the-covid-19-pandemic. Accessed 10 Aug 2020.
3. Peine A, Paffenholz P, Martin L, Dohmen S, Marx G,
Loosen SH. Telemedicine in Germany during the
COVID-19 pandemic: multi-professional national survey. J
Med Internet Res 2020;22:e19745. Crossref
4. Ford D, Harvey JB, McElligott J, et al. Leveraging health
system telehealth and informatics infrastructure to create
a continuum of services for COVID-19 screening, testing,
and treatment. J Am Med Inform Assoc 2020;27:1871-7. Crossref
5. Gong K, Xu Z, Cai Z, Chen Y, Wang Z. Internet hospitals
help prevent and control the epidemic of COVID-19 in
China: multicenter user profiling study. J Med Internet Res
2020;22:e18908. Crossref
6. Kung K, Wong HF, Chen JY. An exploratory qualitative study on patients’ views of medical e-consultation in a public primary care setting. Hong Kong Pract 2016;38:120-7.
7. Greenhalgh T, Koh GC, Car J. COVID-19: a remote assessment in primary care. BMJ 2020;368:m1182. Crossref
8. Fagherazzi G, Goetzinger C, Rashid MA, Aguayo GA,
Huiart L. Digital health strategies to fight COVID-19
worldwide: challenges, recommendations, and a call for
papers. J Med Internet Res 2020;22:e19284. Crossref
9. World Health Organization. A health telematics policy in
support of WHO’s Health-for-all strategy for global health
development: report of the WHO Group Consultation
on Health Telematics, 11-16 December, Geneva,
1997. 1998. Available from: https://apps.who.int/iris/handle/10665/63857. Accessed 7 Sep 2023.
10. McLean S, Sheikh A, Cresswell K, et al. The impact of
telehealthcare on the quality and safety of care: a systematic
overview. PLoS One 2013;8:e71238. Crossref
11. Wootton R. Twenty years of telemedicine in chronic
disease management—an evidence synthesis. J Telemed
Telecare 2012;18:211-20. Crossref
12. Flodgren G, Rachas A, Farmer AJ, Inzitari M, Shepperd S.
Interactive telemedicine: effects on professional practice
and health care outcomes. Cochrane Database Syst Rev
2015;2015:CD002098. Crossref
13. Ekeland AG, Bowes A, Flottorp S. Effectiveness of
telemedicine: a systematic review of reviews. Int J Med
Inform 2010;79:736-71. Crossref
14. Eze ND, Mateus C, Cravo Oliveira Hashiguchi T.
Telemedicine in the OECD: an umbrella review of
clinical and cost-effectiveness, patient experience and
implementation. PLoS One 2020;15:e0237585. Crossref
15. Hung KK, Walline JH, Graham CA. COVID-19: emergency
medicine perspectives from Hong Kong. Eur J Emerg Med
2020;27:163-4. Crossref
16. Hung KK, Walline JH, Chan EY, et al. Health service
utilization in Hong Kong during the COVID-19
pandemic—a cross-sectional public survey. Int J Health
Policy Manag 2022;11:508-13. Crossref
17. Auener S, Kroon D, Wackers E, Dulmen SV, Jeurissen P.
COVID-19: a window of opportunity for positive healthcare
reforms. Int J Health Policy Manag 2020;9:419-22. Crossref
18. Sheng OR, Hu PJ, Chau PY, et al. A survey of physicians’
acceptance of telemedicine. J Telemed Telecare 1998;4
Suppl 1:100-2. Crossref
19. CUHK Medical Clinic. COVID-19 Testing Service
(Company/Groups). Available from: https://cuclinic.hk/programmes/covid-19-testing-service/covid-19-testing-testing-service-company-group. Accessed 30 Jul 2020.
20. Chan EY, Huang Z, Lo ES, Hung KK, Wong EL, Wong SY.
Sociodemographic predictors of health risk perception,
attitude and behavior practices associated with Health-Emergency Disaster Risk Management for biological
hazards: the case of COVID-19 pandemic in Hong Kong,
SAR China. Int J Environ Res Public Health 2020;17:3869. Crossref
21. Moore MA, Coffman M, Jetty A, Petterson S, Bazemore A.
Only 15% of FPs report using telehealth; training and lack
of reimbursement are top barriers. Am Fam Physician
2016;93:101.
22. Schwamm LH. Telehealth: seven strategies to successfully
implement disruptive technology and transform health
care. Health Aff (Millwood) 2014;33:200-6. Crossref
23. Pearl R. Kaiser Permanente Northern California: current
experiences with internet, mobile, and video technologies.
Health Aff (Millwood) 2014;33:251-7. Crossref
24. The Medical Council of Hong Kong. Guidelines for all
registered medical practitioners. Available from: https://www.mchk.org.hk/files/newsletter-26th.pdf. Accessed 30 Jul 2020.
25. Barnett ML, Ray KN, Souza J, Mehrotra A. Trends in telemedicine use in a large commercially insured population, 2005-2017. JAMA 2018;320:2147-9. Crossref
26. Uscher-Pines L, Mehrotra A. Analysis of Teladoc use seems
to indicate expanded access to care for patients without
prior connection to a provider. Health Aff (Millwood)
2014;33:258-64. Crossref
27. Neufeld JD, Doarn CR. Telemedicine spending by
Medicare: a snapshot from 2012. Telemed J E Health
2015;21:686-93. Crossref
28. Mehrotra, A. The convenience revolution for treatment of
low-acuity conditions. JAMA 2013;310:35-6. Crossref
29. Courneya PT, Palattao KJ, Gallagher JM. HealthPartners’
online clinic for simple conditions delivers savings of
$88 per episode and high patient approval. Health Aff
(Millwood) 2013;32:385-92. Crossref
30. Wu J, Huang Y, Tu C, et al. Household transmission
of SARS-CoV-2, Zhuhai, China, 2020. Clin Infect Dis
2020;71:2099-108. Crossref
31. Chan EY, Gobat N, Kim JH, et al. Informal home care
providers: the forgotten health-care workers during the
COVID-19 pandemic. Lancet 2020;395:1957-9. Crossref
32. Hjelm NM. Telemedicine: academic and professional
aspects. Hong Kong Med J 1998;4:289-92.
33. World Medical Association. WMA Statement on the
Ethics of Telemedicine. Available from: https://www.wma.net/policies-post/wma-statement-on-the-ethics-of-telemedicine/. Accessed 15 Apr 2021.