Hong Kong Med J 2023 Aug;29(4):295–300 | Epub 27 Jul 2023
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE CME
Risk factors for postpartum haemorrhage in twin pregnancies and haemorrhage severity
CW Kong, William WK To
Department Obstetrics and Gynaecology, United Christian Hospital, Hong Kong SAR, China
Corresponding author: Dr CW Kong (melizakong@gmail.com)
Abstract
Introduction: This study evaluated risk factors for
postpartum haemorrhage (PPH) in twin pregnancies,
particularly factors associated with major PPH
(blood loss of >1000 mL), to facilitate identification
of high-risk twin pregnancies.
Methods: This retrospective cohort study included
all women with twin pregnancies who delivered at
a tertiary obstetric unit in Hong Kong from 2009 to
2018 and experienced PPH (blood loss of ≥500 mL).
Postpartum haemorrhage was classified using three
thresholds for blood loss volume: ≥500 mL (all PPH),
>1000 mL (major PPH), and >1500 mL (severe PPH).
Risk factors for each threshold of PPH were analysed.
Results: In total, there were 680 twin pregnancies. The
overall incidence of all PPH (≥500 mL) in this cohort
was 27.8%, including minor PPH (500-1000 mL,
20.1%), major but not severe PPH (1001-1500 mL,
4.4%), and severe PPH (>1500 mL, 3.2%). Logistic
regression analysis showed that general anaesthesia
and the use of oxytocin were significant risk factors
for all PPH (≥500 mL); general anaesthesia, in vitro fertilisation, antepartum haemorrhage, placental
abruption, and placenta praevia were significant
risk factors for major PPH (>1000 mL); in vitro
fertilisation, placenta praevia, and obesity were
significant risk factors for severe PPH (>1500 mL).
Conclusion: Women with twin pregnancies who
have obesity, conception by in vitro fertilisation,
or placenta praevia exhibit a high risk of severe
PPH. They should deliver in obstetric units with
readily available blood product transfusions and the
appropriate expertise for prompt management of
severe PPH.
New knowledge added by this study
- Risk factors for severe postpartum haemorrhage differ between twin pregnancies and singleton pregnancies.
- Women with twin pregnancies who have obesity, conception by in vitro fertilisation, or placenta praevia exhibit a high risk of severe postpartum haemorrhage.
- Women with twin pregnancies who have obesity, conception by in vitro fertilisation, or placenta praevia should deliver in obstetric units with readily available blood product transfusions and the appropriate expertise for prompt management of severe postpartum haemorrhage.
- The delivery of twin pregnancies with the above risk factors should involve a multidisciplinary team of experienced obstetricians, anaesthetists, interventional radiologists, and haematologists.
Introduction
In many developed countries, the incidence
of twin pregnancies is rising because of the
increase in maternal age and increasing use of
assisted reproductive procedures.1 2 Postpartum
haemorrhage (PPH) is more common in twin
pregnancies than in singleton pregnancies; this is
usually attributed to substantial distension of the
uterus in twin pregnancies, which leads to uterine
atony after delivery.3 4 Risk factors for severe PPH
in singleton pregnancies include hypertensive
disorders, failure to progress during the second stage
of labour, oxytocin augmentation, instrumental
delivery, and fetal macrosomia.5 However, there have
been few studies concerning specific risk factors for PPH in twin pregnancies because twin pregnancy
itself is considered a risk factor for PPH. This study
evaluated risk factors for PPH in twin pregnancies,
particularly factors associated with major PPH, to
facilitate identification of high-risk twin pregnancies.
Better preparation for peripartum management
of these high-risk twin pregnancies should allow a
multidisciplinary approach involving experienced
obstetricians, anaesthetists, haematologists, and
radiologists to reduce maternal morbidity and
mortality associated with massive haemorrhage.
Methods
This retrospective study included all women with
twin pregnancies who delivered at >24 weeks of gestation in a single tertiary obstetric training unit
from 2009 to 2018 (10-year period) and experienced
PPH (blood loss of ≥500 mL). Obstetric data for
these women were identified using a comprehensive
obstetric database; their electronic and paper
records were then carefully reviewed. Various
maternal demographic and clinical characteristics
(eg, maternal age, parity, method of conception,
body mass index, mode of delivery, cause of PPH,
and antenatal complications such as gestational
diabetes and pre-eclampsia) were compared between
women with and without PPH to identify possible
risk factors. Postpartum haemorrhage was classified
using three thresholds for blood loss volume:
≥500 mL (all PPH), >1000 mL (major PPH), and
>1500 mL (severe PPH). Risk factors for each
threshold of PPH were analysed. Women with
intrauterine fetal death of one or both twins were
excluded from analysis.
In our unit, PPH was managed using a standard
protocol, which began with various oxytocic agents
including oxytocin/ergometrine, oxytocin bolus
and infusion, and carboprost injections. If medical
treatment was unable to control haemorrhage,
second-line conservative procedures involving either
intrauterine balloon tamponade or compression
sutures were used depending on the clinical
situation, as well as the attending obstetrician’s
clinical judgement.
Data entry and analysis were performed using
SPSS (Windows version 24.0; IBM Corp, Armonk
[NY], United States). Possible risk factors were
analysed by the Chi squared test or Fisher’s exact
test, as appropriate. P values <0.05 were considered
statistically significant. Logistic regression analysis
was conducted to identify significant risk factors for
PPH in twin pregnancies. Statistically significant risk
factors identified in univariate analysis were entered
into a stepwise logistic regression model. Odds
ratios and corresponding 95% confidence intervals
were calculated.
Results
In total, there were 47 076 deliveries during the
study period, including 686 deliveries of multiple
pregnancies (680 twin pregnancies and six triplet
pregnancies); only twin pregnancies were included in
the final analysis. Concerning the mode of delivery,
99 women (14.6%) had normal vaginal delivery of
both twins, 67 women (9.9%) had instrumental or
vaginal breech delivery of one or both twins, and 514
women (75.6%) had caesarean delivery of one or both
twins, of which 17 women had combined deliveries
(the first twin was delivered vaginally and the second
twin was delivered by caesarean section). The overall
incidence of all PPH (≥500 mL) in this cohort of
twin pregnancies was 27.8% (189/680), including
minor PPH (500-1000 mL, 137/680 [20.1%]), major
but not severe PPH (1001-1500 mL, 30/680 [4.4%]),
and severe PPH (>1500 mL, 22/680 [3.2%]). In our
database, the overall incidence of all PPH (27.8%
vs 5.7% [2649/46 390]), as well as the incidences of
major PPH [>1000 mL; including severe PPH] (7.6%
vs 0.86% [397/46 390]) and severe PPH [>1500 mL]
(3.2% vs. 0.44% [204/46 390]), were all significantly
higher in twin pregnancies than in singleton
pregnancies during the study period (P<0.001). Most
instances of PPH in twin pregnancies (147/189,
77.8%) were caused by uterine atony; other causes
were placenta praevia or accreta (34/189, 18.0%) and
genital tract trauma (8/189, 4.2%). Although most
instances of PPH in twin pregnancies were caused
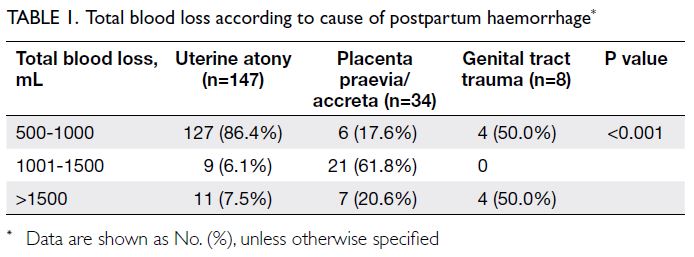
by uterine atony, 86.4% of women with uterine atony
had only minor PPH (500-1000 mL); in contrast,
82.4% of women with placenta praevia had major
PPH >1000 mL (Table 1).
Concerning the treatment of PPH in this cohort, 89.4% of women (169/189) had a successful
outcome with medical treatment alone. In 20
patients, medical treatment was insufficient and
second-line procedures were required: 12 patients
received intrauterine balloon tamponade, four
patients received compression sutures, and four
patients underwent uterine artery embolisation. Three of the 20 patients subsequently required
hysterectomy despite medical treatment and second-line
procedures; the peripartum hysterectomy rate
was 0.4% (3/680). There were no maternal deaths in
this cohort.
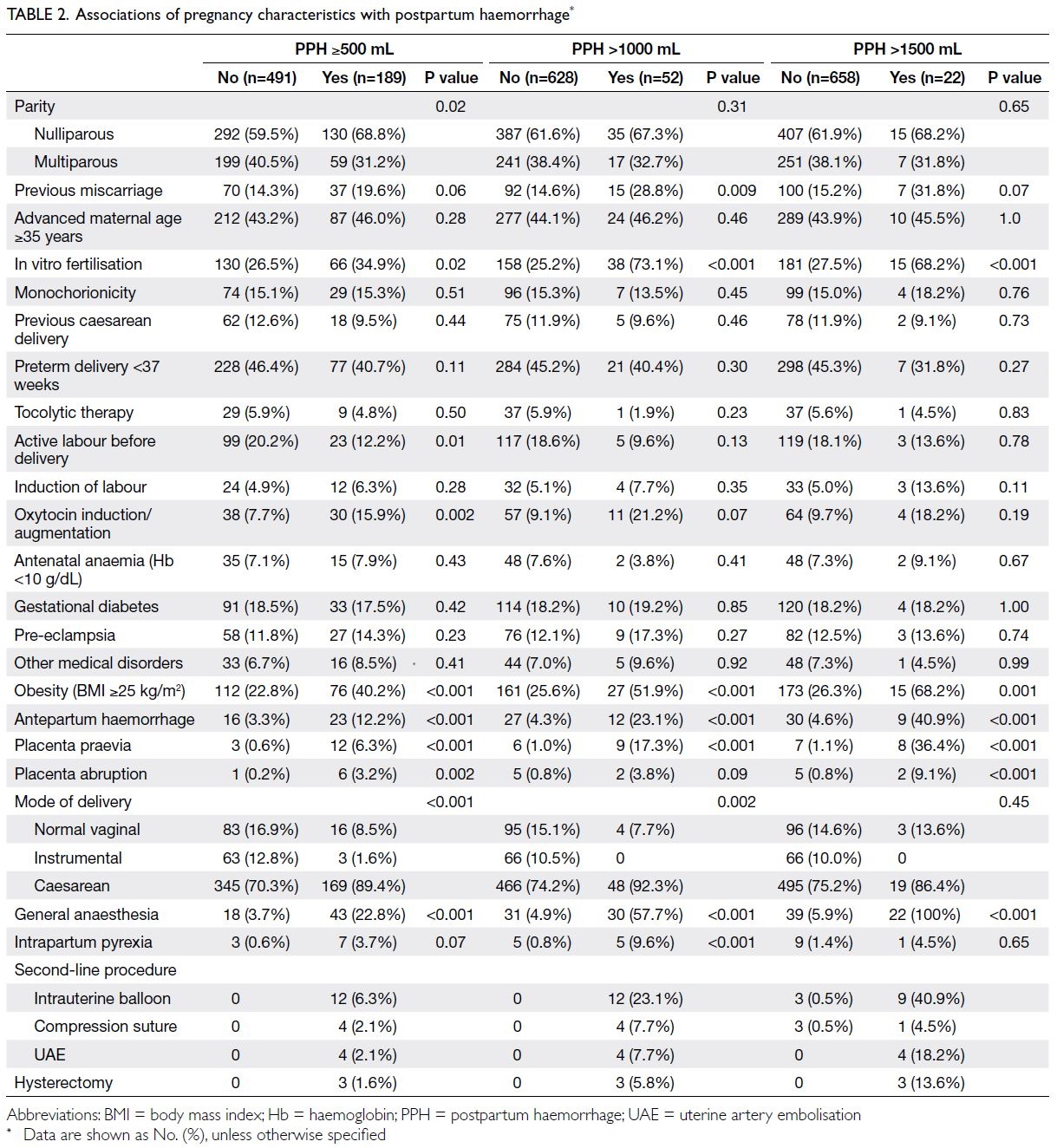
Maternal characteristics and their associations
with each type of PPH are shown in Table 2. Nulliparity and the use of oxytocin were significantly
associated with all PPH ≥500 mL but not major PPH
>1000 mL or severe PPH >1500 mL. Univariate
analysis showed that in vitro fertilisation, maternal
obesity, antepartum haemorrhage, placenta
praevia, placental abruption, caesarean delivery,
general anaesthesia, and intrapartum pyrexia were
significantly associated with various types of PPH.
Logistic regression analysis revealed that general
anaesthesia and the use of oxytocin were significant
risk factors for all PPH ≥500 mL; general anaesthesia,
in vitro fertilisation, antepartum haemorrhage,
placental abruption, and placenta praevia were
significant risk factors for major PPH >1000 mL; in
vitro fertilisation, placenta praevia, and obesity were
significant risk factors for severe PPH >1500 mL
(Table 3).
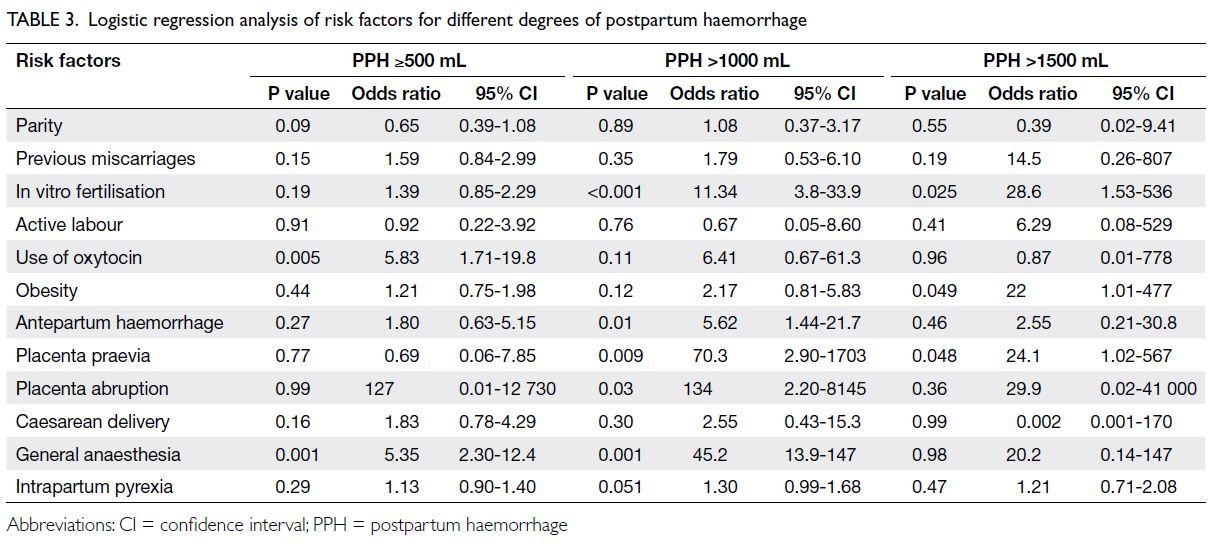
Table 3. Logistic regression analysis of risk factors for different degrees of postpartum haemorrhage
Discussion
Incidence and cause of postpartum haemorrhage in twin pregnancies
This cohort study showed that the incidence of PPH
was significantly higher in twin pregnancies than in
singleton pregnancies. More than one in four of all
twin pregnancies (27.8%) had PPH, compared with
only about one in 20 (5.7%) singleton pregnancies.
Uterine atony caused most instances of PPH (77.8%)
in our cohort of twin pregnancies. There has been
speculation that because the uterus is more distended
in twin pregnancies than in singleton pregnancies,
uterine muscle contraction and retraction is weaker
after delivery, leading to an increased incidence of
uterine atony.6 However, we found that most cases
of uterine atony–related PPH (86.4%) were mild,
with blood loss of 500-1000 mL; morbidity from minor PPH is expected to be low. In contrast, the
incidence of major PPH (>1000 mL; including severe
PPH) was 7.6%; more than one-third (20/52) of the
affected women required second-line procedures
or hysterectomy. A previous study showed that
blood loss of >1000 mL occurred in 24% of twin
pregnancies6; another study revealed that the
incidence of blood loss of >1500 mL was 3.9%.7
Although the incidence of major PPH varies among
studies, it is clear that the potential for morbidity
related to major or severe PPH requires specific
attention to this high-risk group. Postpartum
haemorrhage ≥500 mL remains a useful threshold for
attention from frontline staff8; however, we suggest
modifying the definition for PPH in twin pregnancies
to >1000 mL regardless of the mode of delivery, rather
than the threshold of ≥500 mL used for singleton
pregnancies. Because many twin pregnancies involve
only minor PPH that can be managed with basic
measures, a blood loss threshold of >1000 mL would
be a more effective criterion for identifying high-risk
women who will require more advanced management
such as blood product transfusions or second-line
uterine-sparing procedures.
Risk factors for postpartum haemorrhage in
twin pregnancies
Efforts to identify risk factors for severe PPH
in twin pregnancies may allow evaluation of
available interventions to reduce such risks; they
may also enable advance recognition of high-risk
pregnancies, thereby facilitating staff and resource
allocation during delivery to optimise peripartum
management and reduce morbidity from maternal
haemorrhage. In a retrospective cohort study of 1081 twin pregnancies in the United States, logistic
regression analysis revealed that risk factors for
PPH requiring blood transfusion were nulliparity,
diabetes, intrapartum use of magnesium sulphate,
low haematocrit level, low platelet count, and
administration of general anaesthesia.7 A study
of 171 twin pregnancies in Japan investigated risk
factors for major PPH >1000 mL after vaginal
delivery; gestational age ≥39 weeks, combined
birth weight >5500 g, induction of labour, oxytocin
administration during labour, and prolonged labour
were identified as significant risk factors.6 Our study
showed that the use of oxytocin and administration
of anaesthesia were risk factors for PPH ≥500 mL
in twin pregnancies. However, in contrast to the
previous studies, diabetes and pre-eclampsia were
not risk factors for PPH in our cohort. Although
univariate analysis indicated that nulliparity was a
significant risk factor for PPH ≥500 mL, it did not
remain significant in logistic regression analysis.
In vitro fertilisation
In the present study, logistic regression analysis
indicated that in vitro fertilisation was a significant
risk factor for major PPH >1000 mL and severe
PPH >1500 mL. To our knowledge, few studies have
specifically investigated the relationship between
assisted reproductive technology and PPH. Two
retrospective cohort studies of singleton births
after assisted reproductive technology revealed that
in vitro fertilisation was significantly associated
with a higher incidence of PPH, compared
with spontaneous conception (odds ratios=1.3-1.46).9 10 However, published literature has shown
inconsistent results regarding the relationship
between assisted reproductive technology and PPH
in twin pregnancies. A prospective cohort study of
400 dichorionic twin pregnancies did not identify
differences in PPH incidence between women who
conceived by in vitro fertilisation and women who
conceived spontaneously.11 However, the authors did
not report the definition for PPH used in their study. A
retrospective cohort study of 1239 twin pregnancies
by Bamberg et al12 revealed no difference in PPH
incidence (defined as blood loss of ≥500 mL combined
with haemoglobin level <10 mg/dL) between
women who conceived by artificial reproductive
technologies (eg, hormonal stimulation, intrauterine
insemination, or in vitro fertilisation) and women
who conceived spontaneously. A case-control
study of >3000 women in Norway demonstrated an
increased risk of severe PPH (>1500 mL) in singleton
pregnancies conceived by in vitro fertilisation
compared with controls; it also showed that the
effect of in vitro fertilisation on severe PPH was
more pronounced in multiple pregnancies. After
controlling for maternal factors and pregnancy
complications, the adjusted odds ratios for severe PPH after in vitro fertilisation were 1.6 in singleton
pregnancies and 7.0 in multiple pregnancies.13 Direct
inter-study comparisons of the effect of in vitro
fertilisation on PPH in twin pregnancies are hindered
by inconsistent PPH definitions and the involvement
of various assisted reproductive techniques. In our
study, we strictly defined in vitro fertilisation as
assisted reproduction; we found that this risk factor
was associated with major PPH and severe PPH but
not minor PPH. Overall, in vitro fertilisation appears
to be more frequently associated with severe PPH
rather than minor PPH. There is speculation that
in vitro fertilisation interferes with the formation of
the maternal-fetal interface during the early stages
of implantation, thereby causing early placental
separation and uterine atony that result in PPH.10 14
Although the confounding effects of placenta praevia
and in vitro fertilisation on severe PPH remain
controversial,13 an increased incidence of placenta
praevia has been associated with in vitro fertilisation;
this use of in vitro fertilisation may contribute to
the increased risk of PPH.15 In our study, logistic
regression analysis indicated that placenta praevia
and in vitro fertilisation were significant factors for
major PPH >1000 mL and severe PPH >1500 mL.
Therefore, we suspect that in vitro fertilisation
increases the incidence of PPH by increasing the
incidence of placenta praevia; however, in vitro
fertilisation itself is also an independent risk factor
for PPH. Considering the possible increased risk
of major PPH in multiple pregnancies conceived
by assisted reproductive technology, single embryo
transfer should be recommended during in vitro
fertilisation to reduce maternal morbidity from
major haemorrhage.
General anaesthesia and obesity
In our study, logistic regression analysis revealed
that general anaesthesia was a significant risk factor
for minor and major PPH, but not severe PPH.
Although general anaesthesia may be an independent
risk factor for all types of PPH, its relationship
with severe PPH could be masked by confounding
factors such as placenta praevia—in our centre, most
women with placenta praevia deliver under general
anaesthesia. There is conflicting evidence regarding
the association of obesity with severe PPH. A recent
study of risk factors for severe PPH demonstrated
that obesity was significantly associated with
severe PPH (>1500 mL) in pregnant women (both
singleton and multiple pregnancies), but the
finding was not supported by other epidemiological
analyses.16 Another cohort study indicated that
obesity only slightly increased the risk of PPH; the
authors speculated that this result was related to the
increasing rate of caesarean delivery among women
with obesity.17 However, a large cohort study of
11 363 singleton pregnancies showed an approximate twofold increase in the risk of major PPH (>1000 mL)
among women with obesity, independent of the
mode of delivery.18 The authors found that the
higher rates of PPH in women with obesity could
not be attributed to either major perineal trauma
or retained placenta; they suggested that the
increased rate of PPH in women with obesity was
related to uterine atony.18 However, our study was
not sufficiently powered to analyse the relationship
between obesity and uterine atony.
Limitations
Limitations of this study include its retrospective
design and the high rate of caesarean delivery in our
cohort (75.6%). The high rate of caesarean delivery
in twin pregnancies overall may have introduced
sufficient bias that caesarean delivery itself was
identified as a risk factor for PPH, as demonstrated
in our univariate analyses for minor PPH and major
PPH. Units with lower caesarean delivery rates in
twin pregnancies may have findings that considerably
differ from our results. Nevertheless, we believe that
other risk factors for major and severe PPH remain
valid regardless of the caesarean delivery rate.
Conclusion
Risk factors for severe PPH in twin pregnancies
considerably differed from the risk factors identified
in singleton pregnancies. In vitro fertilisation,
placenta praevia, and maternal obesity were
significant risk factors for severe PPH in twin
pregnancies. Women with twin pregnancies who
have obesity, conception by in vitro fertilisation, or
placenta praevia should deliver in obstetric units
with readily available blood product transfusions and
the appropriate expertise for prompt management
of severe PPH by a multidisciplinary team that
includes experienced obstetricians, anaesthetists,
interventional radiologists, and haematologists.
Author contributions
Concept or design: Both authors.
Acquisition of data: WWK To.
Analysis or interpretation of data: Both authors.
Drafting of the manuscript: CW Kong.
Critical revision of the manuscript for important intellectual content: WWK To.
Acquisition of data: WWK To.
Analysis or interpretation of data: Both authors.
Drafting of the manuscript: CW Kong.
Critical revision of the manuscript for important intellectual content: WWK To.
Both authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
Both authors have disclosed no conflicts of interest.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
Formal ethics approval for this research was granted by the Kowloon Central/Kowloon East Research Ethics Committee
of Hospital Authority, Hong Kong (Ref No.: KC/KE-17-0065/ER-1). Because this was a retrospective study, the requirement
for patient consent was waived by the Committee.
References
1. Eriksson AW, Fellman J. Temporal trends in the rates of multiple maternities in England and Wales. Twin Res Hum Genet 2007;10:626-32. Crossref
2. Ananth CV, Chauhan SP. Epidemiology of twinning in developed countries. Semin Perinatol 2012;36:156-61. Crossref
3. Kramer MS, Berg C, Abenhaim H, et al. Incidence, risk factors, and temporal trends in severe postpartum hemorrhage. Am J Obstet Gynecol 2013;209:449.e1-7. Crossref
4. Conde-Agudelo A, Belizán JM, Lindmark G. Maternal morbidity and mortality associated with multiple gestations. Obstet Gynecol 2000;95:899-904. Crossref
5. Sheiner E, Sarid L, Levy A, Seidman DS, Hallak M. Obstetric risk factors and outcome of pregnancies complicated with early postpartum hemorrhage: a population-based study. J Matern Fetal Neonatal Med 2005;18:149-54. Crossref
6. Suzuki S, Kikuchi F, Ouchi N, et al. Risk factors for postpartum hemorrhage after vaginal delivery of twins. J Nippon Med Sch 2007;74:414-7. Crossref
7. Blitz MJ, Yukhayev A, Pachtman SL, et al. Twin pregnancy and risk of postpartum hemorrhage. J Matern Fetal Neonatal Med 2020;33:3740-5. Crossref
8. Prevention and management of postpartum haemorrhage: Green-top Guideline No.52 [editorial]. BJOG 2017;124:e106-49. Crossref
9. Healy DL, Breheny S, Halliday J, et al. Prevalence and risk factors for obstetric haemorrhage in 6730 singleton births after assisted reproductive technology in Victoria Australia. Hum Reprod 2010;25:265-74. Crossref
10. Hayashi M, Nakai A, Satoh S, Matsuda Y. Adverse obstetric and perinatal outcomes of singleton pregnancies may be related to maternal factors associated with infertility rather than the type of assisted reproductive technology procedure used. Fertil Steril 2012;98:922-8. Crossref
11. Moini A, Shiva M, Arabipoor A, Hosseini R, Chehrazi M, Sadeghi M. Obstetric and neonatal outcomes of twin pregnancies conceived by assisted reproductive technology compared with twin pregnancies conceived spontaneously: a prospective follow-up study. Eur J Obstet Gynecol Reprod Biol 2012;165:29-32. Crossref
12. Bamberg C, Fotopoulou C, Neissner P, et al. Maternal characteristics and twin gestation outcomes over 10 years: impact of conception methods. Fertil Steril 2012;98:95-101. Crossref
13. Nyfløt LT, Sandven I, Oldereid NB, Stray-Pedersen B, Vangen S. Assisted reproductive technology and severe
postpartum haemorrhage: a case-control study. BJOG
2017;124:1198-205. Crossref
14. Sacha CR, Mortimer RM, James K, et al. Placental pathology
of term singleton live births conceived with fresh embryo
transfer compared with those conceived without assisted
reproductive technology. Fertil Steril 2022;117:758-68. Crossref
15. Romundstad LB, Romundstad PR, Sunde A, von Düring V,
Skjaerven R, Vatten LJ. Increased risk of placenta previa in
pregnancies following IVF/ICSI; a comparison of ART and
non-ART pregnancies in the same mother. Hum Reprod 2006;21:2353-8. Crossref
16. Siddiqui A, Azria E, Howell EA, Deneux-Tharaux C;
EPIMOMS Study Group. Associations between maternal
obesity and severe maternal morbidity: findings from
the French EPIMOMS population-based study. Paediatr
Perinat Epidemiol 2019;33:7-16. Crossref
17. Butwick AJ, Abreo A, Bateman BT, et al. Effect of maternal body mass index on postpartum hemorrhage.
Anesthesiology 2018;128:774-83. Crossref
18. Fyfe EM, Thompson JM, Anderson NH, Groom KM,
McCowan LM. Maternal obesity and postpartum
haemorrhage after vaginal and caesarean delivery among
nulliparous women at term: a retrospective cohort study.
BMC Pregnancy Childbirth 2012;12:112. Crossref