© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Squamous cell carcinoma of the colon: a case
report
July L Lee, LMCHK; Tommy CH Man, MB, BS, FHKAM (Surgery)
Department of Surgery, Caritas Medical Centre, Hong Kong SAR, China
Corresponding author: Dr July L Lee (lj541@ha.org.hk)
Case report
A 71-year-old man, chronic smoker and drinker,
presented to the Accident and Emergency
Department of our institution in February 2021 with
a history of abdominal pain and per rectal bleeding
for 1 day. He also reported a weight loss of 15 kg over
1 month. On physical examination he was tachycardic
and febrile; an abdominal mass was palpable over
the right lower quadrant with localised peritoneal
signs. Abdominal computed tomography revealed a
10 cm×9 cm×7.5 cm mass arising from the ascending
colon with wall thickening of the caecum and ileum.
There was also thickening of the perirenal fascia and
a small amount of free fluid (Fig). Carcinoembryonic
antigen (CEA) level was elevated (33 μg/L).
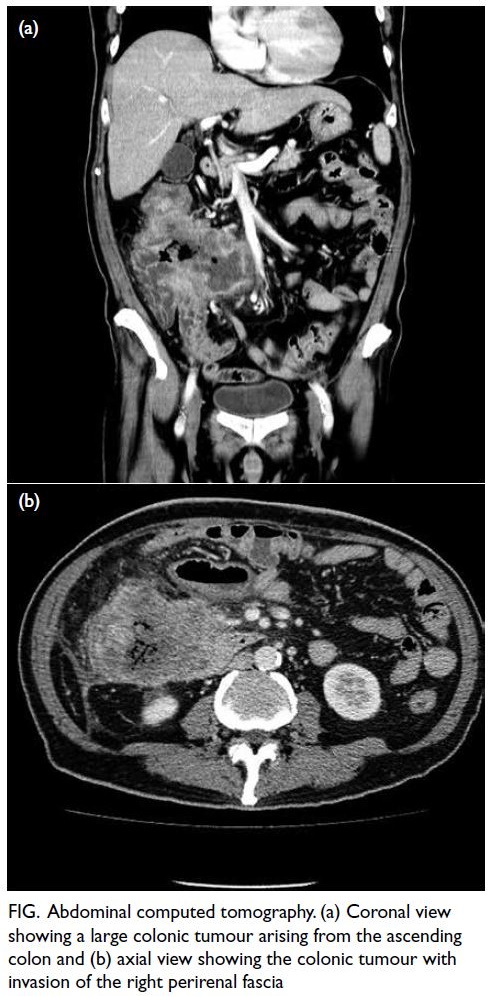
Figure. Abdominal computed tomography. (a) Coronal view showing a large colonic tumour arising from the ascending colon and (b) axial view showing the colonic tumour with invasion of the right perirenal fascia
Laparotomy revealed an 8 cm×9 cm fungating
tumour with circumferential involvement arising
from the ascending colon. The tumour invaded the
second and third portion of the duodenum, the right
retroperitoneal space, ileocecal valve, and terminal
ileum. It also presented with a concealed perforation
sealed-off by the distal ileum without evidence of
faecal contamination. There were no palpable liver
masses and no signs of peritoneal deposits. Surgical
excision of the tumour was performed to offer the
best chance of survival. A right hemicolectomy
with en bloc resection of the invaded structures
was performed and a Roux-en-Y duodenojejunal
anastomosis and end-to-end ileocolic anastomosis
were fashioned.
The patient had a satisfactory postoperative
recovery and was discharged from hospital under
the care of our cancer care programme that included
monitoring of CEA levels and annual colonoscopy
and computed tomography of the abdomen and
pelvis.
Interestingly, the histological examination
revealed a carcinoma with squamous differentiation.
Extensive sampling failed to reveal any glandular
component. The final staging using TMN
classification was Stage IIB (pT4bN0) and Dukes’
stage B. Due to the aggressive nature of the tumour,
adjuvant chemotherapy was planned.
Soon after surgery, a lung mass was seen on
chest X-ray and CEA level showed a rising trend. A
positron emission tomography scan revealed multiple deposits over the abdominal cavity and a 2-cm right
lung mass with mediastinal and right supraclavicular
lymph node metastasis. An excisional biopsy of the
supraclavicular lymph node was consistent with
metastatic squamous cell carcinoma (SCC).
In view of the presence of multiple metastases
the patient was commenced palliative chemotherapy
for disease control with gemcitabine and carboplatin.
Serial tomography also showed progression of the
abdominal, lung and lymph node metastasis. His
condition further deteriorated and he succumbed 7
months after the initial diagnosis.
Discussion
Colorectal cancer (CRC) is the third most common
cancer worldwide.1 In Hong Kong it is the second most common cancer and the second leading cause
of cancer deaths.2
Most CRCs are adenocarcinomas and account
for 95% of all cases. The remainder have non-epithelial
histology such as carcinoid tumours,
sarcomas, and lymphoid tumours. Squamous cell
carcinoma accounts for only 0.1% to 0.5% of all types
of CRC cases.3
The first case of SCC was reported in 1919 by
Schmidtmann. The majority of the data available
comes from individual case reports with only about
100 cases reported worldwide.3
The mean age at presentation is 55 to 60 years
old with no gender or ethnic predilection. The
most common sites are the rectum, right colon,
and sigmoid. The clinical presentation is similar
to that of colonic adenocarcinoma, such as altered
bowel habit, rectal bleeding, abdominal pain, weight
loss, anaemia, and palpable abdominal mass. The
duration of symptoms ranges from several weeks to
months. Lymphatic spread follows the same route as
adenocarcinomas with similar metastatic sites such
as the liver, peritoneum, lung, and bone.
Squamous cell carcinoma of the colon has
been associated with ulcerative colitis, infection
with human immunodeficiency virus, human
papillomavirus, infestation with schistosomiasis,
Entamoeba histolytica, history of previous surgical
procedures, and radiotherapy.3 Nonetheless many reported cases have coexisting conditions.
The aetiology is unclear. There are three
proposed pathogenic pathways, namely: (1) SCC
arising from squamous differentiation from stem
cells; (2) squamous metaplasia that undergoes
malignant transformation; and (3) squamous
differentiation from existing adenocarcinomas.4 The last pathway is supported by Williams et al4 who described squamous differentiation in three of 750 adenomas.
Miyamoto et al5 proposed a four-criteria
selection for diagnosis: (1) metastasis from other
sites must be excluded; (2) a squamous-lined
fistulous tract must not involve the affected bowel;
(3) SCC of the anus with proximal extension must be
excluded; and (4) histological analysis must confirm
the SCC.
Colorectal SCCs are more locally invasive
and carry a worse prognosis than their common
counterpart. Most cases are diagnosed at a late
disease stage, often presenting as complications
such as bowel obstruction or perforation. The overall
5-year survival of SCC of the colon is 35%, with 52%
mortality within the first year, compared with the
overall 60% 5-year survival of adenocarcinomas.3 Frizelle et al6 found that early stages of SCC had a similar prognosis to adenocarcinomas after evaluating 52 patients from the Mayo Clinic tissue
registry in 2001. Nonetheless metastasis was present
in 49% of these patients.
There is no current standard treatment. Most
cases are managed following the guidelines for
adenocarcinomas. The crucial steps are a complete
surgical excision with negative margins, and
aggressive chemotherapy. Various chemotherapy
regimens have been proposed using 5-fluorouracil,
capecitabine and gemcitabine.7 For SCC located in
the rectum, chemoradiotherapy has demonstrated
good success for local control, similar to anal SCC.
The most important prognostic predictor is cancer
stage. Factors associated with poor prognosis are
a right-sided location and ulcerated or annular
carcinomas.
Considering only 10% to 20% of all CRC cases
present with local invasion, this feature should
alert surgeons to this form of aggressive CRC. The
timing of post-treatment surveillance (serial CEA
and annual tomography and colonoscopy) can be
adjusted considering the higher mortality and worse
prognosis. Systemic staging investigations such as
computed tomography thorax or positron emission
tomography scan can be regularly implemented in
view of the higher rate of metastasis.
Author contributions
Both authors contributed to the concept or design of the study, acquisition of data, analysis or interpretation of data, drafting of the manuscript, and critical revision of the manuscript for
important intellectual content. Both authors had full access to
the data, contributed to the study, approved the final version
for publication, and take responsibility for its accuracy and
integrity.
Conflicts of interest
Both authors have no conflicts of interest to disclose.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patient was treated in accordance with the Declaration of Helsinki and provided informed consent for the treatment/procedures and verbal consent for publication.
References
1. World Health Organization. Colorectal cancer. 2020. Available from: https://www.iarc.who.int/cancer-type/colorectal-cancer/. Accessed 5 Jun 2023.
2. Hong Kong Cancer Registry. Top ten cancers. 2020. Available from: https://www3.ha.org.hk/cancereg/topten.html. Accessed 5 Jun 2023.
3. Linardoutsos D, Frountzas M, Feakins RM, Patel NH, Simanskaite V, Patel H. Primary colonic squamous cell
carcinoma: a case report and review of the literature. Ann
R Coll Surg Engl 2020;102:e1-7. Crossref
4. Williams GT, Blackshaw AJ, Morson BC. Squamous carcinoma of the colorectum and its genesis. J Pathol
1979;129:139-47. Crossref
5. Miyamoto H, Nishioka M, Kurita N, et al. Squamous cell carcinoma of the descending colon: report of a case and
literature review. Case Rep Gastroenterol 2007;1:77-83. Crossref
6. Frizelle FA, Hobday KS, Batts KP, Nelson H. Adenosquamous and squamous carcinoma of the colon and upper rectum: a clinical and histopathologic study. Dis Colon Rectum 2001;44:341-6. Crossref
7. Wang ML, Heriot A, Leong T, Ngan SY. Chemoradiotherapy in the management of primary squamous-cell carcinoma of the rectum. Colorectal Dis 2011;13:296-301. Crossref

