© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Challenging surgical management of right
internal jugular vein haemangioma: a case report
Özlem Balcıoğlu, MD1; Serkan Ertugay, MD2; Hakan Posacıoğlu, MD2
1 Cardiovascular Surgery Department, Near East University, Nicosia, Cyprus
2 Cardiovascular Surgery Department, Ege University, Izmir, Turkey
Corresponding author: Dr Özlem Balcıoğlu (balcioglu@neu.edu.tr)
Case report
A 27-year-old female was admitted in January 2021
to the cardiovascular department of Ege University,
Turkey with a history of a gradually enlarging
swelling in the right supraclavicular area. Physical
examination revealed a semi-soft, semi-mobile
and painless mass localised at the bottom third of
the right lower neck, extending to the clavicle with
no distinct inferior border. It appeared to follow
upper mediastinal inflow. The overlying skin was
normal, and no pulsation or thrill was detected.
All laboratory results including infection markers
were within normal limits. Sonographic evaluation
demonstrated a solid, hypoechoic and lobulated
mass with slow flow pattern and slow filling of
the right internal jugular vein (IJV). Computed
tomography scan illustrated a homogenous oval
solid lesion on the right lateral aspect of the neck,
originating from the thyroid level and elongating to
the infraclavicular area. It measured 33 × 51 × 51 mm,
with peripheral interrupted nodules in arterial phase
(Fig 1a). The mass was located 180° to the IJV. The
border could not be differentiated and the trachea
was deviated medially to the left and right common
carotid artery posteriorly. Magnetic resonance
imaging demonstrated intermediate signal intensity
on T1-weighted image (Fig 1b) and very high signal
intensity on T2-weighted image of an enhanced solid
mass (Fig 1c). The clinical diagnosis was vascular
malformation or haemangioma. Surgical excision was
planned. After general anaesthesia and positioning
of the neck, a neck incision was made parallel and
anterior to the right sternocleidomastoid muscle,
similar to that performed for a standard carotid
endarterectomy. Although the incision was extended
through the sternal notch, it was insufficient to enable
complete excision. A right-sided mini ‘J-sternotomy’
was performed subsequently to facilitate complete
visualisation of the brachiocephalic bifurcation.
Exploration and dissection of the mass from
peripheral tissue revealed that it arose from the
distal part of the right IJV and extended through the
brachiocephalic bifurcation.
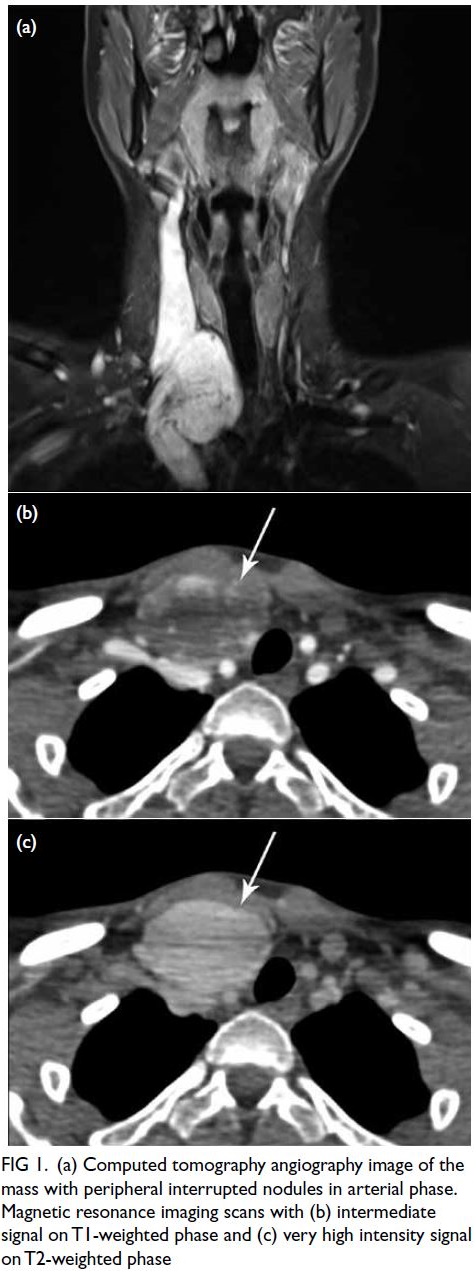
Figure 1. (a) Computed tomography angiography image of the mass with peripheral interrupted nodules in arterial phase. Magnetic resonance imaging scans with (b) intermediate signal on T1-weighted phase and (c) very high intensity signal on T2-weighted phase
The proximal part of the right IJV, right
subclavian vein and distal part of the right innominate vein were explored and controlled by
silicon loop. Following heparin administration, the
proximal right subclavian vein was ligated and all
other vessels clamped. An incision was made and
the mass was observed to extend into the vascular
lumen. It was removed en bloc along with the distal
segment of the right IJV and proximal segment of
the right brachiocephalic vein. Vein reconstruction
was performed to prevent venous hypertension in
the neck. Because of the large diameter of vascular
structures, a synthetic 8-mm polytetrafluoroethylene
self-ringed graft was sutured between the distal
part of the right innominate bifurcation and
right IJV (Fig 2a and 2b). Histopathology revealed
CD34(+), endothelial cell(+) haemangioma. The
patient experienced no postoperative complications.
Both antiaggregant and anticoagulant therapy
were commenced on postoperative day 1 with
acetylsalicylic acid (100 mg/day) and apiksaban
(5 mg/day). Control computed tomography
scan 11 months after surgery revealed excellent
reconstruction with an intact and patent graft (Fig 2c).
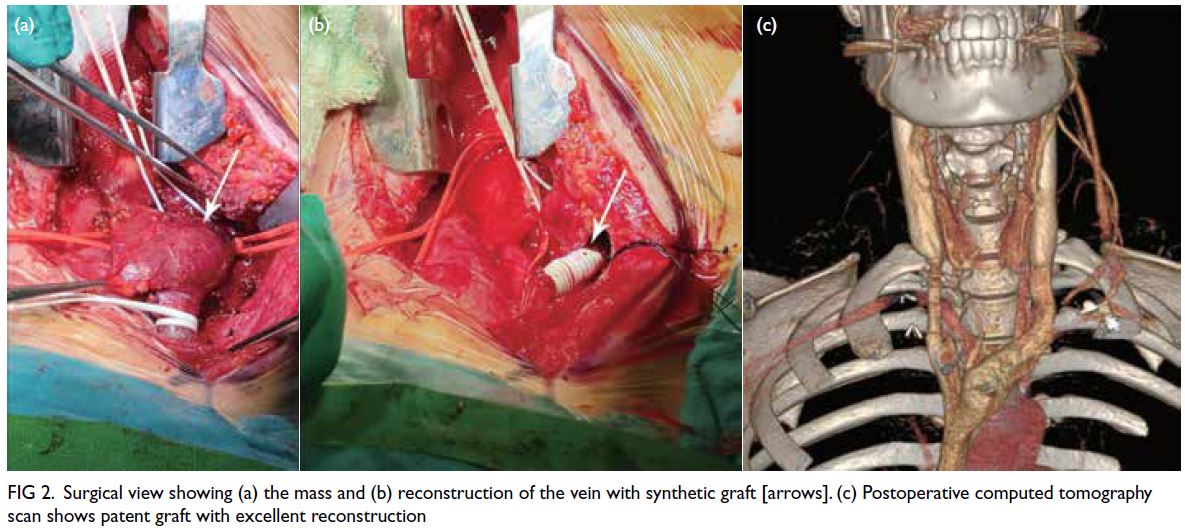
Figure 2. Surgical view showing (a) the mass and (b) reconstruction of the vein with synthetic graft [arrows]. (c) Postoperative computed tomography scan shows patent graft with excellent reconstruction
Discussion
The nomenclature of primary tumours of the
venous system is based on their origin: lipomas,
leiomyomas, haemangiomas, leiomyosarcomas,
and angiosarcomas. Leiomyosarcomas are the most
common tumours with a malignant course. Until
the classification scheme proposed by Mulliken and
Glowacki,1 the terms ‘haemangioma’ and ‘vascular malformation’ were used interchangeably because of
the lack of a standardised nomenclature. Although
they are classified as benign tumours, accurate
diagnosis is possible only by histopathological
evaluation following surgical excision. According to
their classification, haemangiomas are characterised
by rapidly proliferating endothelial cells and
frequent mitosis. They are not usually visible at
birth but become apparent at the neonatal stage
and demonstrate rapid proliferation during the first
2 years, followed by spontaneous involution. In
contrast, vascular malformations possess flattened
endothelial cells and ectatic vessel formation.
Although haemangiomas grow with hyperplasia,
vascular malformations expand by hypertrophy.1
Some authors have noted that trauma, sepsis,
hormonal changes or pressure in the venous system
may cause expansion of the vascular malformation.2
Although cases of external jugular vein
haemangiomas and vascular malformations have
been reported,2 only three cases of IJV haemangioma
have been reported. The exceptions were incidentally
diagnosed asymptomatic cases; these presented with
swelling and may have led to incorrect differential
diagnoses of neck malignancy, infection, lymphoma
or thrombosis. A multidisciplinary approach
with a full physical examination and medical
history is required to reach a definitive diagnosis.
Advanced imaging techniques play an important
role in diagnosis and are helpful when planning
treatment. The sonographic and magnetic resonance
imaging features of vascular malformations and
haemangiomas have been studied and described in detail. In a case series, Ahuja et al3 reported the
radiological features of vascular malformations in
the external jugular vein, aiming to help clinicians
make treatment decisions. Head and neck vascular
malformations typically showed intermediate signal
intensity on T1-weighted images, very high signal
intensity on T2-weighted images and variable
enhancement following intravenous administration
of gadolinium.4 Similar radiological features were
identified in our case. To date, different treatment
modalities such as cryotherapy, laser therapy, and
steroids have been explored. Excision of a benign
vein tumour with the adjacent vein segment en bloc
is the most successful curative treatment and enables
pathological confirmation of the diagnosis.5
In previous case studies of IJV haemangiomas,
a supraclavicular approach was applied to access the
mass and reconstruction not performed following
removal of the vein segment.5 In our challenging case,
the neck incision was extended to the sternal notch
and continued with a right-sided mini ‘J-sternotomy’
to ensure adequate control over the mass. Contrary
to other case reports of IJV haemangioma, we
performed vein reconstruction to prevent venous
hypertension and swelling of the neck. To the best
of our knowledge, this is the first reported case
where vein reconstruction was performed using a
synthetic graft following successful surgical excision
of a haemangioma from the IJV via an extraordinary
approach.
Author contributions
Concept or design: Ö Balcıoğlu, S Ertugay.
Acquisition of data: S Ertugay, H Posacıoğlu.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: Ö Balcıoğlu, S Ertugay.
Critical revision of the manuscript for important intellectual
content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patient was treated in accordance with the Declaration of Helsinki and provided written informed consent for publication of this report.
References
1. Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg 1982;69:412-22. Crossref
2. de Oliveira JC, Barreto FT, Chimelli BC, et al. External jugular vein hemangioma: case report. J Vasc Bras 2019;18:e20180026. Crossref
3. Ahuja AT, Yuen HY, Wong KT, et al. External jugular vein vascular malformation: sonographic and MR imaging appearances. AJNR Am J Neuroradiol 2004;25:338-42.
4. Werner JA, Dünne AA, Folz BJ, et al. Current concepts in the classification, diagnosis and treatment of hemangiomas and vascular malformations of the head and neck. Eur Arch Otorhinolaryngol 2001;258:141-9. Crossref
5. Duggal P, Chaturvedi P, Pai PS, Nair D, Juvekar SL, Rekhi B. Internal jugular vein vascular malformation presenting as mass at root of neck: a case report. BMC Ear Nose Throat Disord 2009;9:5. Crossref

