© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Time for change? Feasibility of introducing micromodules into medical student education: a randomised controlled trial
CF Ng, FRCSEd (Urol), FHKAM (Surgery); Kevin Lim, MB, ChB; CH Yee, FRCSEd (Urol), FHKAM (Surgery); Peter KF Chiu, FRCSEd (Urol), FHKAM (Surgery); Jeremy YC Teoh, FRCSEd (Urol), FHKAM (Surgery); Franco PT Lai, BN
Department of Surgery, SH Ho Urology Centre, The Chinese University of Hong Kong, Hong Kong SAR, China
Corresponding author: Prof CF Ng (ngcf@surgery.cuhk.edu.hk)
Abstract
Introduction: Didactic lectures have been the
foundation of learning for many medical students.
However, in recent years, the flipped classroom
model has become increasingly popular in medical
education. This approach enhances pre-class
learning, allowing the limited contact time between
clinicians and medical students to be focused on
practical issues. This study evaluated the effectiveness
and non-inferiority of online micromodule teaching
in terms of knowledge transfer concerning specific
urology topics.
Methods: Medical students without prior exposure
to the urology subspecialty were enrolled in the study,
then randomised to a traditional didactic lecture
group or an online micromodule group. Knowledge
transfer was assessed by pre-intervention and post-intervention
multiple-choice questions and objective
structured clinical examinations that involved the
acquisition of medical histories from real patients.
Results: In total, 45 medical students were enrolled
(22 in the traditional didactic group and 23 in the
online micromodule group). In terms of knowledge
transfer (assessed by objective structured clinical
examinations), the efficacy of online micromodules
was comparable to traditional didactic lectures, although the difference was not statistically
significant (P=0.823). There were no significant
differences in terms of knowledge acquisition,
retention, or clinical application between the two groups.
Conclusion: terms of acquiring, retaining, and applying foundational urological knowledge, online
micromodules can help medical students to achieve
outcomes comparable with the outcomes of didactic
lectures. Online micromodules may be a viable
alternative to traditional didactic lectures in urology education.
New knowledge added by this study
- Compared with traditional didactic lectures, online micromodules have similar knowledge transfer efficacy in medical student education.
- The flipped classroom model may help to allow the limited contact time between clinicians and medical students to focus on practical training and experience sharing.
- Large-group didactic lectures will likely decline in the future.
- There is an urgent need to develop teaching methods appropriate for the modern era.
- Micromodules may be regarded as a flipped classroom component that can facilitate learning and knowledge transfer.
Introduction
The coronavirus disease 2019 pandemic dramatically
changed modern life. Traditional didactic lecture
methods suddenly became impossible,1 and there
was a need to maintain social distancing. A shift
to online didactic lectures was the most common
solution. However, there is evidence that information
acquisition becomes inefficient beyond the first 10 to
15 minutes of a lecture.2 It may be even more difficult to concentrate in online lectures that lack interaction
between the speaker and audience. Notably, videos
longer than 10 minutes are less likely to be viewed.3 4
Short online video lectures (ie, micromodules), with
or without interactive elements, offer an attractive
alternative. Such micromodules can be incorporated
into the flipped classroom (FC) model, which is a
pedagogical paradigm shift that rearranges how time
is spent in and out of the classroom.5
The FC model is becoming increasingly
popular in medical education. It is attractive to the
current generation of students who are accustomed
to utilising digital media; on average, 70% of students
prefer this learning model.6 Students can learn pre-class
materials at their own pace; they can also
enjoy more in-class active learning and interaction.
Moreover, they can negotiate the FC platform
at their preferred time and in their preferred
place. Instead of passively delivering information
in class, educators can devote valuable contact
time to interactions with students, exploration of
their needs, and discussions of more nuanced and
challenging topics.6 The acquisition of foundational
information becomes an active self-directed process,
outside of the classroom.
Considering the continuous growth of medical
literature, today’s medical students must acquire
an expanded field of knowledge before graduation.
A modern urology clerkship should alleviate the
intense time pressures placed on students by helping
them to effectively and efficiently develop diagnostic
and procedural core competencies. Where possible,
students should be allowed to learn by active
participation, rather than listening and reading,
during the limited available contact time. The FC
model holds great promise in achieving this goal.7
The success of the FC model requires an
efficacious online platform that facilitates self-directed
learning; stringent evaluation of the online
platform is necessary. However, methodologically
rigorous qualitative and quantitative studies and
evidence-based recommendations are scarce.8 Most
published works quote practical wisdom, anecdotes,
and principles of educational theory as the basis for
their recommendations.9
This pilot study was conducted to compare
our institution’s online micromodule platform
with traditional didactic lectures in facilitating the
acquisition of foundational urological knowledge by
medical students.
Methods
This prospective, single-centre, single-blind
randomised controlled trial, performed at a tertiary
academic hospital, investigated whether online
micromodules are non-inferior to traditional
didactic lectures as an instructional medium; this
trial is a component of a larger movement towards
the FC approach in clinical training.
Urology curriculum
The urology clerkship is a surgical subspecialty in our faculty curriculum. All medical students have
1 week of clinical attachment in their final year of
medical clerkship training (Year 6). The standard
curriculum consists of lectures, bedside tutorials, and clinical shadowing. Traditionally, lectures are
delivered to the whole class at the beginning of
the academic year. Students then shadow our team
in small groups on the wards, in clinics, and in the
operating theatre. Teaching is opportunistic, based
on symptoms, signs, investigations, diseases, and
procedures encountered in the clinical setting.
Formal knowledge assessment is conducted during
end-of-year examinations in the form of written
examinations (multiple-choice questions [MCQs]
and short-answer questions), objective structured
clinical examinations (OSCEs), and clinical short
case examinations.
Study intervention
In this study, we selectively assessed knowledge
transfer with regard to two urology topics:
approaches to lower urinary tract symptoms
(LUTS) and haematuria. First, a didactic lecture
on the management of LUTS and haematuria,
along with other topics, was recorded during its
delivery in our routine lecture series for final-year
students. Subsequently, two micromodules were
prepared concerning the management of LUTS and
haematuria; the micromodule content was similar to
the didactic lecture content. The study participants
continued with their scheduled urology training
in Year 6; therefore, the study intervention was
regarded as supplemental curriculum. Because the
participants’ overall learning opportunities were not
affected, we decided to obtain only verbal consent
for inclusion in the study.
Randomisation, allocation concealment, and
blinding of participants
Medical students in Years 4 to 6 with no exposure
to the urology subspecialty rotation were voluntarily
recruited for the study. Participants were randomly
allocated to either traditional didactic lectures or
online micromodules; rigorous proctored tests
were administered in accordance with the schedule
shown in the Figure. Permuted block randomisation
was conducted using a computer program. Random
allocation sequences were placed into identical
sealed and numbered envelopes. Designated
research staff members were responsible for
allocating consecutively numbered envelopes to the
participants.
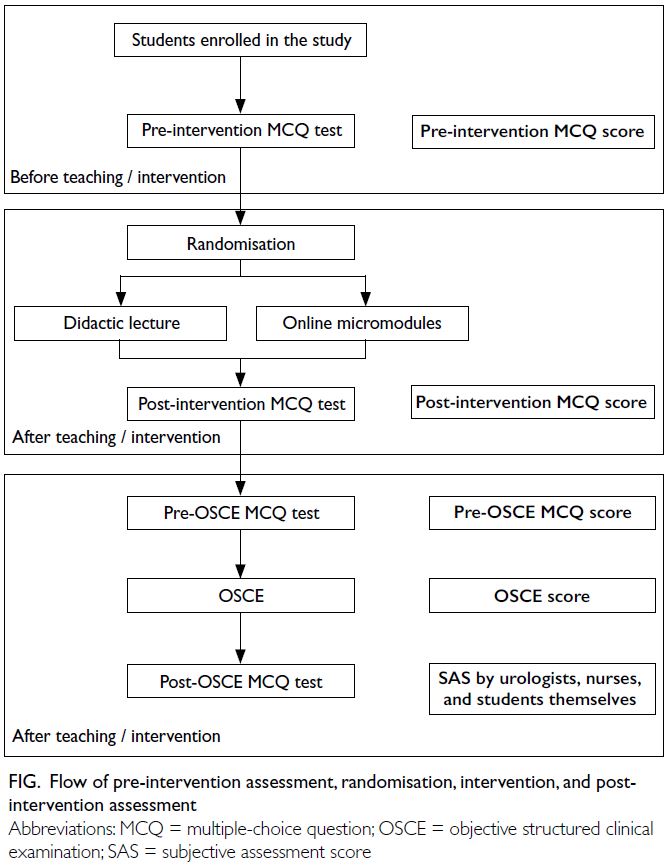
Figure. Flow of pre-intervention assessment, randomisation, intervention, and post-intervention assessment
Students randomised to the traditional didactic
lecture were grouped into a class, which watched
the pre-recorded 45-minute didactic lecture in the
lecture theatre (as if the students were attending a
standard lecture). Students randomised to the online
micromodule group viewed the micromodules on separate computers at their own pace. The total
runtime of these micromodules was 10 minutes each,
and students were expected to explore the content
in its entirety within 45 minutes. The breadth and
depth of topics covered in both interventions were
identical to each other and similar to past lectures;
the only difference was the delivery medium. The
students could not be blinded; however, all outcome
assessors (including content creators) were blinded
to intervention allocation because the didactic
lecture was not delivered live or in person.
Assessment
We used the Kirkpatrick’s four-level training
evaluation model as the basis for evaluations of
instructional effectiveness. In the context of online
learning, Level 1 (reaction) refers to the student’s
affective responses to training quality or relevance,
usually measured by surveys; Level 2 (learning)
refers to knowledge directly obtained from the
online lecture, usually measured by knowledge
tests such as MCQs and true-false questions; Level
3 (behaviour outcomes/transfer of learning) refers
to improvements in the outcomes of tasks not
directly taught in the instructional content, typically
measured through practical or standardised
examinations; and Level 4 (results) refers to the
impact of training on organisational goals (ie, actual
benefit to patients).
Prior to randomisation, a pre-intervention
MCQ test was used to determine participant baseline
knowledge. Immediately after randomisation and
completion of training, participants repeated the
MCQ test to determine the degree of knowledge
acquisition (ie, Kirkpatrick Level 2). Their confidence
in the subject matter was also measured using a 10-point scale (ie, Kirkpatrick Level 1).
After 3 weeks of teaching, each participant
underwent individual assessments in outpatient
clinics. The MCQ test was administered again
to test knowledge retention. Then, an OSCE was
administered to assess the participant’s approach
to a real patient with either LUTS or haematuria. A
nurse was present as a chaperone and third-party
assessor, who gave a subjective assessment score,
measured using a 10-point scale. The participant
then presented the case to a urologist, who assessed
the collected information using a structured marking
scheme. Additionally, the urologist gave a subjective
assessment score, similar to the nursing assessment.
All student assessors were blinded to the allocated
teaching approach. The scores from the nurses and
urologists were used to assess student performance
in the OSCE (ie, Kirkpatrick Level 3); they also were
used to assess the overall effectiveness and safety
of the micromodule teaching approach. Due to the
study design, the impact of training on organisational
goals (ie, Kirkpatrick Level 4) was not assessed.
Statistical analysis
Statistical analysis was performed using SPSS
(Windows version 23.0; IBM Corp, Armonk [NY],
United States). There was no crossover between
treatment arms. Data were analysed using an
intention-to-treat approach. Descriptive statistics
(means, standard deviations, and ranges) were
used for demographic data. Independent samples
t tests or one-way multivariate analysis of variance
were used for parametric continuous variables; the
Mann–Whitney U test was used for non-parametric
continuous variables; and the Chi squared test was
used for categorical variables. P values <0.05 were
considered statistically significant.
Results
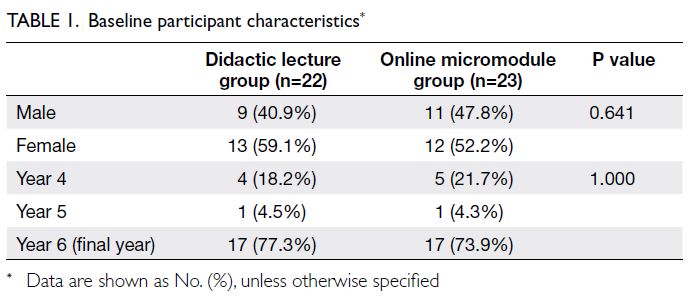
Between 4 December 2017 and 22 January 2018,
45 medical students voluntarily enrolled in this
study at our hospital; 22 students were randomised
to the didactic lecture group and 23 students were
randomised to the online micromodule group. Most
participants (77% and 74%, respectively) were in
their final year of medical education. There were no
significant differences in demographic composition
between the two groups (Table 1). The difference
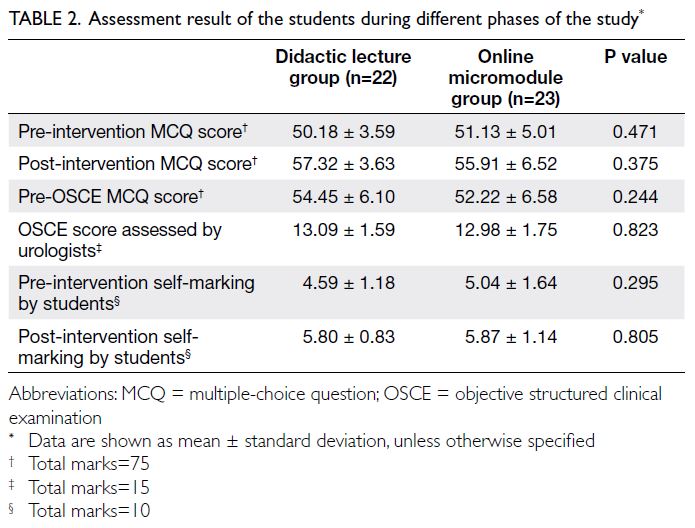
in pre-intervention MCQ scores also was not
statistically significant (P=0.471), indicating that
the participants had similar baseline knowledge
(Table 2).
In this study, the primary outcome was the
difference in OSCE scores between the didactic
lecture and online micromodule groups, as assessed
by the urologists. This outcome corresponds to
Level 3 of the Kirkpatrick model. Three-quarters
of participants assessed real patients with LUTS;
the remaining participants assessed patients with
haematuria. There was no difference in OSCE score
between the groups (13.09 ± 1.59 vs 12.98 ± 1.75,
P=0.823) [Table 2].
The secondary outcome was the difference
in knowledge acquisition and retention between
interventions. Knowledge acquisition was defined
as the difference between pre-intervention and
post-intervention MCQ scores. Knowledge
retention was defined as the difference between
pre-intervention MCQ score and pre-OSCE MCQ
score (taken 3 weeks after the intervention). Both
of these outcomes correspond to Level 2 of the
Kirkpatrick model. There were improvements in
MCQ scores after teaching in both groups, although
not statistically significant. However, there was no
difference in the degree of improvement between
the groups. Therefore, knowledge acquisition for
the two groups were similar. For the assessment of
knowledge retention, one-way multivariate analysis
of variance with adjustment for pre-intervention
MCQ scores revealed no statistically significant difference between post-intervention MCQ score and pre-OSCE MCQ score (Wilks’ Lambda=0.894,
P=0.101, partial η2=0.106).
Finally, subjective assessment of confidence
and competence was conducted; this assessment
corresponds to Kirkpatrick Level 1. There was a
significant improvement in post-intervention self-rated
confidence, but there was no difference in the
degree of improvement between the groups (Table 2). In terms of clinical performance (Kirkpatrick
Level 3), there were no differences between the
groups in terms of subjective assessment score by
the urologists (7.89 ± 0.91 vs 7.70 ± 0.91, P=0.487) or
nurses (8.05 ± 0.72 vs 8.04 ± 0.71, P=0.993).
Discussion
Our results show that both didactic lectures and
online micromodules can help medical students
achieve comparable outcomes in terms of acquiring,
retaining, and applying foundational urological
knowledge. Thus, online learning platforms may be
viable substitutes for didactic lectures in the broader
context of a move towards the FC approach.
In a systematic review of literature concerning
the use of online lectures in undergraduate medical
education,6 45 studies were identified; only 21 (47%)
of those studies had clearly established control and
intervention groups. Among the 21 studies, only six
(29%) assessed learning using an OSCE or equivalent
practical examinations; the remaining studies used
MCQ tests. There was considerable heterogeneity in
the manner by which online lectures were integrated
into existing surgical curricula, which hindered
meta-analysis. However, online lectures generally
tended to be non-inferior to traditional lectures.
Online learning offers many benefits to
educators and students. First, it ensures round-the-clock
access to learning materials. Second, it allows
students to revisit these materials throughout the
curriculum. Third, online learning platforms can
track and verify that students have accessed and
completed specific materials. Fourth, electronic
content can be updated in a convenient manner;
distribution is instantaneous and universal. Fifth,
students have autonomy over the sequence and
pace of learning, as well as the allocation of time;
these aspects allow them to tailor their learning
experience to meet personal objectives. Sixth,
although a higher initial investment may be required,
online learning platforms can be reused, exchanged,
and collaborated on; they offer new economies
of scale.10 11 Finally, the coronavirus disease 2019
pandemic led to concerns about the spread of
infection, such that online micromodules became
an attractive option for medical student education
that permitted social distancing. Notably, online
micromodules represent easily accessible media
that can be used for continuing medical education,
and interactive teaching can be added to enhance
learning experience.
An important limitation of online learning
is that educators may utilise the scheduling
freedom offered by online platforms to overburden
students with learning materials; they may not
consider the large amount of non-classroom time
that may be allocated to other tasks. To avoid this
phenomenon, we established ‘bite-sized’ modules (ie,
micromodules) and ensured that all topics covered
are highly relevant to future clinical practice. Such
short modules also match the students’ attention
spans.2 3 4 However, we acknowledge that educators
may initially expend greater effort in the preparation
of online modules.4
Although there were some improvements in
MCQ scores after the lecture or micromodules, they
were weaker than expected, potentially because the
post-intervention MCQ test occurred immediately
after the lecture and there was insufficient time for
participants to process the lecture content. Another
limitation of the study design was that there were no
tutorials or in-class interactions after the lectures. Thus, the acquired knowledge may not have been
consolidated, resulting in suboptimal knowledge
retention. Nevertheless, this study was designed to
demonstrate non-inferiority between pedagogical
approaches. Educators should remember that online
learning is one component of the overall FC model.
An overhaul of the broader teaching mentality
and existing curriculum is required to realise the
paradigm shift offered by the FC model. Thus, simple
conversion of existing lecture notes to an electronic
format will not effectively facilitate learning. There is
a need for full utilisation of software/technologies to
prepare multimedia/truly interactive micromodules;
this approach is more likely to enhance student
learning experiences. It is also challenging to
develop effective methods for assessment of student
competencies. Educators should support and
collaborate with clinicians in this regard, thereby
complementing each other’s efforts.4 12 13 14 15
In addition to video lectures, online platforms
can be used to deliver diverse educational content,
including interactive multimedia learning modules,
discussion forums, polling, and virtual patients.
We deliberately excluded these materials for the
duration of this study because they represent distinct
instructional configurations in terms of content
and interactivity. The combination of interactive
elements and lecture into a single intervention
group would have confounded and invalidated the
results.6 8 Thus, the video lectures solely consisted of
slide decks, narration, and video. More studies are
needed to determine how to best incorporate these
teaching approaches into the instructional design of
future curricula.11
The present study focused on the transfer of
clinical knowledge and management of common
urological symptoms via micromodules. Future
research should examine whether online lectures
can also effectively transfer practical procedural
skills. Because of time constraints and the
curriculum system, exposure during the clerkship
period is extremely limited. Therefore, the current
instructional approach for physical examination and
basic clinical procedures (eg, insertion of urethral
and central venous catheters) is often informal,
opportunistic, and unstructured. Further studies
may clarify the role of online education in procedural
training.
Conclusion
Online micromodules were non-inferior to a
traditional didactic lecture in terms of knowledge
transfer focused on urology topics. Further
enhancement of the interactive elements of the
instructional medium will improve learning
experience. Micromodule utilisation can be
optimised during the development of the FC model
of teaching. In times such as the recent pandemic era, where social distancing must be maintained
throughout the educational process, there is an
urgent need for curriculum reform that maximises
the use of technology to enhance medical student
learning.
Author contributions
Concept or design: CF Ng.
Acquisition of data: CH Yee, PKF Chiu, JYC Teoh, FPT Lai.
Analysis or interpretation of data: K Lim.
Drafting of the manuscript: K Lim, CF Ng.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: CH Yee, PKF Chiu, JYC Teoh, FPT Lai.
Analysis or interpretation of data: K Lim.
Drafting of the manuscript: K Lim, CF Ng.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
As editors of the journal, CF Ng and JYC Teoh were not involved in the peer review process. Other authors have
disclosed no conflicts of interest.
Funding/support
This research received support from the Micro-Module Courseware Development Grant Scheme of The Chinese
University of Hong Kong, Hong Kong (Ref No.: 3210817).
Ethics approval
This research aimed to improve instruction through the use of educational tests administered to the participants. All
participants provided informed consent without the collection
of personal or sensitive data.
References
1. Al Samaraee A. The impact of the COVID-19 pandemic on medical education. Br J Hosp Med (Lond) 2020;81:1-4. Crossref
2. Mehanna WN. e-Pedagogy: the pedagogies of e-learning. Res in Learn Technol 2004;12:279-93. Crossref
3. Stuart J, Rutherford RJ. Medical student concentration during lectures. Lancet 1978;2:514-6. Crossref
4. Koo CL, Demps EL, Farris C, Bowman JD, Panahi L, Boyle P. Impact of flipped classroom design on student
performance and perceptions in a pharmacotherapy
course. Am J Pharm Educ 2016;80:33. Crossref
5. Rotellar C, Cain J. Research, perspectives, and recommendations on implementing the flipped classroom.
Am J Pharm Educ 2016;80:34. Crossref
6. Cook DA, McDonald FS. E-learning: is there anything special about the “E”? Perspect Biol Med 2008;51:5-21. Crossref
7. Johnson L, Becker S, Estrada V, Freeman A. NMC horizon report: 2014 higher education edition. Austin (Texas): The New Media Consortium. Available from: https://www.learntechlib.org/p/130341/. Accessed 10 Mar 2020.
8. Sinclair PM, Kable A, Levett-Jones T, Booth D. The effectiveness of Internet-based e-learning on clinician
behaviour and patient outcomes: a systematic review. Int J
Nurs Stud 2016;57:70-81. Crossref
9. Cook DA. The research we still are not doing: an agenda for the study of computer-based learning. Acad Med 2005;80:541-8. Crossref
10. Tang B, Coret A, Qureshi A, Barron H, Ayala AP, Law M. Online lectures in undergraduate medical education:
scoping review. JMIR Med Educ 2018;4:e11. Crossref
11. Cook DA, Levinson AJ, Garside S, Dupras DM, Erwin PJ, Montori VM. Internet-based learning in the health
professions: a meta-analysis. JAMA 2008;300:1181-96. Crossref
12. AAMC Institute for Improving Medical Education. Effective
use of educational technology in medical education.
Colloquium on educational technology: recommendations
and guidelines for medical educators. 2007. Available from: https://store.aamc.org/downloadable/download/sample/sample_id/111/. Accessed 10 Mar 2020.
13. Sezer B, Abay E. Looking at the impact of the flipped classroom model in medical education. Scand J Educ Res 2019;63:853-68. Crossref
14. Hurtubise L, Hall E, Sheridan L, Han H. The flipped classroom in medical education: engaging students to build competency. J Med Educ Curric Dev 2015;2:35-43. Crossref
15. Hew KF, Lo CK. Flipped classroom improves student learning in health professions education: a meta-analysis. BMC Med Educ 2018;18:38. Crossref