© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
REMINISCENCE: ARTEFACTS FROM THE HONG KONG MUSEUM OF MEDICAL SCIENCES
Analysis of visual fields: history, advances and
importance in the management of glaucoma
Nancy SY Yuen, MB, BS(HK), FHKAM (Ophthalmology)
Guest author, Education and Research Committee, Hong Kong Museum of Medical Sciences Society
Most people are familiar with the assessment of
visual acuities, in which a patient’s ability to read
and recognise distant objects is measured by a
standardised, objective method, such as a Snellen
chart. Visual acuity is commonly measured by
optometrists to provide people with an eyeglass
prescription for refractive errors. However, visual
acuity only describes the most acute vision of
the central macula of our eyes. There are various
ophthalmological and neurological diseases that may
affect the field of vision, and yet patients with such
diseases can perform well in tests of visual acuity.
The visual field refers to how wide of an area one’s
eye can see when one focuses on a central point.
Visual field testing is one method that clinicians and
ophthalmologists use to measure how much vision
one has in either eye and how much vision loss may
have occurred over time.1
Evaluation of peripheral visual field was first
performed more than 2000 years ago, whereas
quantitative measurement of the visual field has
been utilised for around 200 years. One of the first
accounts of peripheral visual field evaluation was by
Hippocrates, from around the late fifth century BC,
when he described hemianopia. A further attempt to
map a patient’s visual field defect was made by Ptolemy
in 150 BC. These documented early evaluations of
the visual field were mostly qualitative, and it was
not until 1856 when Albrecht von Graefe developed
quantitative visual field measurements, where he
presented visual field loss that was characteristic
of glaucoma. von Graefe also published examples
of visual field losses associated with many other
ophthalmic or neurological diseases.
Jannik Bjerrum popularised perimetry (ie,
testing of visual field) using a tangent screen with a
standardised target size and background illumination.
One of the most important contributions to modern
perimetry was the work of Hans Goldmann in 1945.
He developed a hemispherical bowl perimeter
that provided a uniform background illumination
and a moving optical projection system that could
superimpose stimuli on the background. Static and
kinetic perimetry can be performed by using the
Goldmann perimeter with a variety of targets of
varying sizes, luminance, and colour characteristics.
Goldmann’s work also further described evaluation
of normal controls and patients with glaucoma and
other diseases affecting the visual pathways.
Friedmann created the first central field
analyser model in 1966, which contained a patient
chin and head rest and a source of illumination for
the stimulus patterns, with a total of 46 stimuli. The
donated Friedmann Visual Field Analyser Mark II
is a model used in the 1970s, with improvements
that included 99 stimuli and more automation (Fig).
To perform the visual field assessment, the patient
rested his or her head on the chin and head rest.
Each eye was tested individually, with the patient
instructed to look at a central fixation point in the
machine as stimuli were generated automatically; a
technician then manually recorded the results on a
chart printout provided by Friedmann.
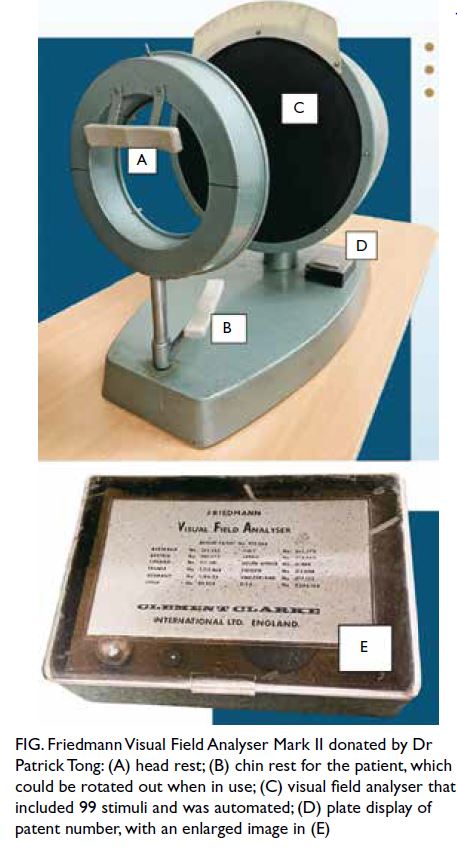
Figure. Friedmann Visual Field Analyser Mark II donated by Dr Patrick Tong: (A) head rest; (B) chin rest for the patient, which could be rotated out when in use; (C) visual field analyser that included 99 stimuli and was automated; (D) plate display of patent number, with an enlarged image in (E)
In the early 1970s, Drs John Lynn and George
Tate developed one of the first automated perimeters,
although Dr Franz Fankhauser is widely considered
the foremost expert in this field who produced and
popularised the first automated perimeter known
as the Octopus. Many other automated or semi-automated
perimetry devices followed, including the
Fieldmaster, DICON, Humphrey Field Analyzer, and
Easyfield (Oculus).2
Clinicians and scientists are working to refine
the test for the patient to detect small targets on a
uniform background, so as to quantitatively evaluate
and document the functional status of the peripheral
field of view for diagnosis and follow-up of many
ophthalmological or neurological diseases.
Some common clinical conditions that require
visual field assessment are listed as follows:
More recently in the development of automated
visual field testing, advances have been made to
make these tests and procedures more standardised,
automated, accurate, precise, efficient, quantitative,
repeatable, statistically reliable, and easy to use.
There has been further software development over
the years for the analysis of glaucoma progression—the most prevalent and important long-term blinding
eye disease.
The changes in visual field or progression
of defects caused by chronic glaucoma are very
subtle. Together with the fact that individual test
result reliability relies heavily on physical status and
consistent performance of the patient, visual field
testing continues to be perceived by many patients
as one of the most demanding tests.
Clinicians now use standard automated
perimetry for the diagnosis and management of
glaucoma throughout the world. Various testing
paradigms and analytic methods have been
developed to simplify the diagnosis of glaucoma
and the interpretation of its progression. Glaucoma
detection and progression analyses are also
incorporating more information and will be improved
further as deep-learning strategies are applied.
With advancing technology, besides the use
of visual field testing for monitoring the functional
changes of the optic nerve in patients with glaucoma,
ophthalmologists also closely monitor the structure
of the optic nerve by means of structural scanning
using optical coherence tomography. Furthermore,
perimetric and structural testing will likely become
more closely intertwined as testing platforms and
progression analysis incorporate these measures.3
With an ageing population, glaucoma has
become the most important and prevalent chronic
blinding eye disease in Hong Kong. Additionally,
with the increasing prevalence of normal-tension
glaucoma (patients with glaucoma who do not have
high eye pressure), which constitutes up to 30%
of all glaucoma cases, monitoring requires ever
more detail and cannot rely solely on eye-pressure
monitoring.
Many of these patients require systemic
investigations, which include blood tests for common
cardiovascular risk factors, imaging of the brain in
suspicious cases, and sleep study. There are many
reports of a higher risk of glaucoma among patients
with sleep apnoea, and a higher prevalence of sleep
apnoea in patients with glaucoma. This is especially
true for patients with normal-tension glaucoma. In
this group, treatment of the sleep apnoea will help to
stop the deterioration and further loss of optic nerve
fibres and visual field.4 5 6
1. Simpson DA, Crompton JL. The visual fields: an interdisciplinary history II. Neurosurgeons and quantitative
perimetry. J Clin Neurosci 2008;15:229-36. Crossref
2. Johnson CA, Wall M, Thompson HS. A history of perimetry and visual field testing. Optom Vis Sci 2011;88:E8-E15. Crossref
3. Camp AS, Weinreb RN. Will perimetry be performed to monitor glaucoma in 2025? Ophthalmology 2017;124:S71-S75. Crossref
4. Chuang LH, Koh YY, Chen HS, et al. Normal tension glaucoma in obstructive sleep apnea syndrome: a structural and
functional study. Medicine (Baltimore) 2020;99:e19468. Crossref
5. Garcia-Villanueva C, Milla E, Bolarin JM, et al. Impact of systemic comorbidities on ocular hypertension and open-angle
glaucoma, in a population from Spain and Portugal. J Clin Med 2022;11:5649. Crossref
6. Lin PW, Friedman M, Lin HC, Chang HW, Wilson M, Lin MC. Normal tension glaucoma in patients with obstructive
sleep apnea/hypopnea syndrome. J Glaucoma 2011;20:553-8. Crossref

