Hong Kong Med J 2023 Apr;29(2):178–80 | Epub 12 Apr 2023
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
LETTERS TO THE EDITOR
Better preparation for intubation
Daniel KK Ng, MB, BS, MD1; Cynthia Cheung2; WY Wu, MNurs3
1 Department of Paediatrics, Hong Kong Sanatorium & Hospital, Hong Kong SAR, China
2 Department of Paediatrics, The Chinese University of Hong Kong, Hong Kong SAR, China
3 Research Department, Hong Kong Sanatorium & Hospital, Hong Kong SAR, China
Corresponding author: Dr Daniel KK Ng (daniel.kk.ng@hksh.com)
To the Editor—We read with interest the article by Cheng et al1 who reported a child with peritonsillar
abscess and impending airway obstruction who
underwent two failed attempts at intubation with
consequent rapid desaturation down to an oxygen
saturation (SpO2) level of 50% to 60%, requiring
insertion of a laryngeal mask to maintain ventilation
before successful intubation. In the same issue, a
standard protocol for intubation was suggested
by Leung et al.2 They describe the rescue plan for
intubation, alluding to the need for pre-oxygenation
for 3 to 5 minutes prior to rapid sequence induction.
These articles highlight the need to increase the
arterial oxygen reserve to avoid rapid desaturation
with all its dire consequences.
We would like to remind readers about a recent
technological development that enables measurement
and monitoring of the oxygen reserve index (ORI),
the increase in arterial oxygen pressure (PaO2) in real
time. As shown by the oxygen dissociation curve,
desaturation would be delayed if PaO2 could be
increased from 100 mmHg to say 200 mmHg.3 Oxygen
reserve index is a proprietary technology available
using the Masimo pulse oximeter with a range
from 0 to 1. When SpO2 reaches 100%, any further
increase is reflected in the ORI that will rise above
0. We suggest that attending doctors pre-oxygenate
to an ORI well above 0 to achieve a greater oxygen
reserve and prevent the rapid desaturation reported
by Cheng et al.1 We also suggest provision of pre-oxygenation
via heated humidified high-flow (HHHF)
oxygen with fraction of inspired oxygen (FiO2) up
to 1. Nonetheless, the other end of the spectrum to
hypoxaemia is hyperoxia, less obviously harmful but
still to be avoided with excessive oxygenation leading
to atelectasis.4 5 To prevent severe hyperoxia, ORI
should be maintained at around 0.5. Monitoring the
ORI and titrating FiO2 such that the ORI is maintained
above 0 may help prevent both a hypoxic state during
intubation and hyperoxia. During intubation, ORI
should also be continuously monitored along with
SpO2 since it can predict a decline in SpO2.
Pre-oxygenation by HHHF followed by
continuous HHHF during intubation is also
beneficial, even in the presence of paralysis that
occurs during rapid sequence induction. Continuous
removal of oxygen by red blood cells flowing through
the capillaries abutting the alveoli leads to a negative
pressure that draws in air from the atmosphere only
if the whole airway is patent. This phenomenon is
called apnoea oxygenation.6 Nonetheless classic
apnoeic oxygenation in the absence of high flow provides little clearance of carbon dioxide and may
lead to progressive respiratory acidosis. The impact
of adding high flow on CO2 clearance is controversial,
with CO2 rising at a much lower rate of 0.15 kPa/min
in adults6 compared with only classic apnoeic
oxygenation and a reported rate of 0.45 kPa/min.7
Nonetheless CO2 clearance is reported to be lower
in children at 0.32 kPa/min.8 In a single case report,
the end-tidal CO2 was reported to be only 9.1 kPa
at the end of apnoea of 46 minutes, much lower
than the expected rise to >10 kPa in the absence
of ventilation.9 Fortunately, PaCO2 up to 13.3 kPa
is not reported to be associated with adverse
outcome.10 Continuing HHHF during intubation not
only facilitates oxygenation, but it also potentially
improves CO2 clearance by flushing of the dead
space, hence lowering the risk of CO2 toxicity.6
Since HHHF can be administered during intubation
without obstructing the procedure, its use should be
continued during the intubation process.
Leung et al2 also mentioned cricoid pressure
as an essential step in rapid sequence induction
although recent evidence has cast doubt on its
effectiveness in preventing aspiration and the
potential distortion of anatomy making intubation
more difficult.11 We suggest that cricoid pressure
be applied only if deemed essential by the attending
team. It should not be performed routinely during
rapid sequence induction.
In conclusion, administration of HHHF with
enriched oxygen should be incorporated into the
standard protocol for pre-oxygenation and used
continuously during intubation. Oxygen reserve
index should be continuously monitored to achieve
mild hyperoxia to prevent rapid desaturation by a
timely increase of FiO2 or flow or chin lift/jaw thrust
to establish upper airway patency. This index is also
useful to avoid severe hyperoxia and consequent
atelectasis.
Author contributions
All authors contributed to the drafting of the letter and critical revision for important intellectual content. All
authors approved the final version for publication and take
responsibility for its accuracy and integrity.
Conflicts of interest
The authors have no conflicts of interest to disclose.
Funding/support
This letter received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
1. Cheng GC, Wong JW. Managing limitations of the LMA Classic laryngeal mask as a conduit for tracheal intubation
in impending paediatric airway obstruction: a case report.
Hong Kong Med J 2022;28:321-3. Crossref
2. Leung KK, Ku SW, Fung RC, et al. Airway management in children with COVID-19. Hong Kong Med J 2022;28:315-20. Crossref
3. Scheeren TW, Belda FJ, Perel A. The oxygen reserve index (ORI): a new tool to monitor oxygen therapy. J Clin Monit Comput 2018;32:379-89. Crossref
4. Koo CH, Park EY, Lee SY, Ryu JH. The effects of intraoperative inspired oxygen fraction on postoperative pulmonary parameters in patients with general anaesthesia: a systemic review and meta-analysis. J Clin Med 2019;8:583. Crossref
5. Staehr-Rye AK, Meyhoff CS, Scheffenbichler FT, et al. High intraoperative inspiratory oxygen fraction and risk of major
respiratory complications. Br J Anaesth 2017;119:140-9. Crossref
6. Patel A, Nouraei SA. Transnasal humidified rapid-insufflation ventilatory exchange (THRIVE): a physiological method of increasing apnoea time in patients with difficult airways. Anaesthesia 2015;70:323-9. Crossref
7. Frumin MJ, Epstein RM, Cohen G. Apneic oxygenation in man. Anesthesiology 1959;20:789-98. Crossref
8. Humphreys S, Rosen D, Housden T, Taylor J, Schibler A. Nasal high-flow oxygen delivery in children with abnormal
airways. Pediatr Anaesth 2017;27:616-20. Crossref
9. Ng LY, Chan AK, Lam TW. The use of high-flow nasal oxygen during airway management in a child with epidermolysis bullosa dystrophica and a difficult airway. Anaesth Rep 2019;7:96-9. Crossref
10. Cheng Q, Zhang J, Wang H, Zhang R, Yue Y, Li L. Effect of acute hypercapnia on outcomes and predictive factors for complications among patients receiving bronchoscopic interventions under general anesthesia. PLoS One 2015;10:e0130771. Crossref
11. Erley CL. Cricoid pressure during induction for tracheal intubation in critically ill children: a report from National Emergency Airway Registry for Children. J Emerg Med 2018;55:737. Crossref
Authors' reply
Karen KY Leung, MB, BS, MRCPCH1; SW Ku, MB, BS, MRCP1; Ronald CM Fung, MB, ChB, MRCPCH1; WF Hui, MB, ChB, MRCPCH1; CC Au, MB, BS, MRCPCH1; WL Cheung, MB, BS, MRCPCH1; WH Szeto, BNurs, MNurs1; Jeff CP Wong, MB, BS, MRCPCH1; KF Kwan, MB, BS, MRCP (Irel)2; KL Hon, MB, BS, MD1
1 Paediatric Intensive Care Unit, Department of Paediatrics and Adolescent Medicine, Hong Kong Children’s Hospital, Hong Kong SAR, China
2 Department of Paediatrics and Adolescent Medicine, Hong Kong Children’s Hospital, Hong Kong SAR, China
Corresponding author: Dr KL Hon (ehon@hotmail.com)
We thank the authors for pointing out the importance
of increasing arterial oxygen reserve to avoid rapid
desaturation with all its dire consequences.1 In this regard, we would like to address aspects related to intubation, oxygenation, ventilation and perfusion.
This is even more important in conditions such
as status asthmaticus, raised intracranial pressure,
and pulmonary hypertension. In these scenarios,
rapid sequence intubation might be a misnomer.
The patient should be allowed an adequate period of 3 to 5 minutes of pre-oxygenation to prevent desaturation during the intubation process.2 3
The oxygen reserve index is a great suggestion
if oximeter with this function is available. In an
emergency, ensuring oxygen saturation remains well
above 90% may be the most we can achieve before
attempting intubation with an endotracheal tube or
laryngeal mask airway. During an emergency, most
of us will probably rely on hearing the beeping and
seeing the screen of the oxygen saturation monitor
instead of carefully oxygenating until oxygen reserve
index is above 0.5.
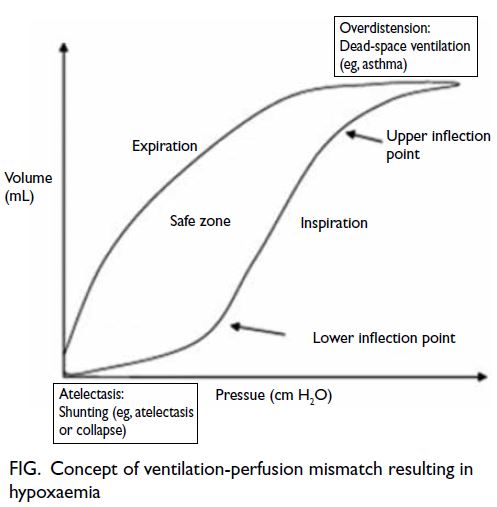
Understanding the oxygen saturation curve,
the pressure-volume curve, and the pathophysiology
of hypoxaemia and ventilation/perfusion mismatch
is another fundamental mental process that care
providers must continuously go through even during
the critical moment of resuscitation, with atelectatic
shunting and dead-space ventilation being problems
at the two extremes of the pressure-volume curve.
The concept of ventilation/perfusion mismatch
leading to hypoxaemia is fundamental, with
overdistention leading to dead-space ventilation as in
critical asthma syndrome and collapse or atelectasis
leading to shunting in collapse of a large segment of
the lung (Fig).4
Issues with hypercapnia and hypocapnia are
also important in cardiac and cerebral pathologies,
and we agree with the authors’ comments about CO2
clearance. Continuous monitoring of arterial CO2
partial pressure and end-tidal CO2 prior to securing
an airway in an emergency remains challenging and
may be impossible.
Last, in emergency situations, the use of
a laryngeal mask airway and the use of video laryngoscopes to improve glottic visualisation are all important routine methods to avoid hypoxaemia and ensure good oxygenation during emergency resuscitation.
Author contributions
Concept or design: KL Hon.
Acquisition of data: KL Hon, KKY Leung.
Analysis or interpretation of data: KL Hon, KKY Leung.
Drafting of the reply: KL Hon, KKY Leung.
Critical revision of the reply for important intellectual content: All authors.
Acquisition of data: KL Hon, KKY Leung.
Analysis or interpretation of data: KL Hon, KKY Leung.
Drafting of the reply: KL Hon, KKY Leung.
Critical revision of the reply for important intellectual content: All authors.
All authors had full access to the data, contributed to the reply, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
As an editor of the journal, KL Hon was excluded from the review process for this reply. Other authors have disclosed no
conflicts of interest.
Funding/support
This reply received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
1. Ng D, Cheung C, Wu WY. Better preparation for intubation. Hong Kong Med J 2023;29:178-9. Crossref
2. Mace SE. Challenges and advances in intubation: rapid sequence intubation. Emerg Med Clin North Am 2008;26:1043-68. Crossref
3. Leung KK, Ku SW, Fung RC, et al. Airway management in children with COVID-19. Hong Kong Med J 2022;28:315-20. Crossref
4. Hon KL, Leung AK. Medications and recent patents for status asthmaticus in children. Recent Pat Inflamm Allergy Drug Discov 2017;11:12-21. Crossref