Hong Kong Med J 2023 Apr;29(2):165–7 | Epub 3 Apr 2023
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Acute acquired esotropia during the COVID-19 pandemic: four case reports
YH Lau, MB, ChB1,2; Emily WH Tang, FCOphth (HK), FHKAM (Ophthalmology)1,2; Tracy HT Lai, FCOphth (HK), FHKAM (Ophthalmology)1,2; Kenneth KW Li, FRCOphth, FHKAM (Ophthalmology)1,2
1 Department of Ophthalmology, United Christian Hospital and Tseung Kwan O Hospital, Hong Kong SAR, China
2 Department of Ophthalmology, School of Clinical Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong SAR, China
Corresponding author: Dr Kenneth KW Li (lkw856@ha.org.hk)
Case reports
The coronavirus disease 2019 (COVID-19)
pandemic started in 2020. To reduce transmission
of the virus, many schools suspended face-to-face
teaching and moved to online classes. Nonetheless
online teaching impacted the health of children, for
example weight gain, disruption of sleep cycle, and
psychosocial stress.1 As ophthalmologists, we are
particularly concerned about insufficient outdoor
exposure and increased screen time since they are
known to be associated with the development of
myopia.2 In addition to myopia, there have been
reports worldwide of acute acquired esotropia cases
as a result of excessive use of electronic devices.3
A recent study reported a 3.11% prevalence
of strabismus among children in Hong Kong,4
higher than that in other Asian countries including
Singapore and Korea. Acute acquired esotropia is a
rarer type of convergent squint. It is thought to be
related to an inability to maintain balance between
converging and diverging forces of the eyes, and
patients with underlying uncorrected refractive
error or psychosocial stress are more prone to
developing acquired esotropia. This article describes
four patients in Hong Kong who developed acute
acquired esotropia as a result of excessive screen
time during the COVID-19 pandemic.
Case 1
A 10-year-old girl presented to our clinic with a
history of new-onset comitant convergent squint
since September 2020. Old photos taken before
the COVID-19 pandemic showed straight eyes.
The patient reported excessive smartphone use
(continuously for around 8 hours per day) since
the commencement of online classes in 2020. She
had non-accommodative left eye esotropia of 35
prism dioptres (PD) at 1/3 m and 45 PD at 6 m on
prism cover test. Worth’s 4-dot test revealed left
eye suppression. Cycloplegic refraction revealed
hyperopia of +1.00 and +1.75 dioptres in the right
and left eye, respectively. Extraocular movements
were full for both eyes. Magnetic resonance imaging of the brain was unremarkable. The provisional
diagnosis was acute acquired esotropia. The patient
refused to stop using her phone and the condition
did not resolve with conservative management. In
mid-August 2021, 11 months after onset of esotropia,
5.5 to 6 mm bilateral medial rectus recession via a
forniceal approach was performed under general
anaesthesia. There was straight alignment 9 months
postoperatively (Fig 1). The patient was advised to
limit time spent on electronic devices to prevent
recurrence of esotropia.

Figure 1. (a) Self-taken photo by the patient in case 1 before operation showed right esotropia around 30 to 35 prism dioptres with glasses. (b) Straight alignment on day 2 after operation
Case 2
A 12-year-old boy with previously straight eyes
presented with a history of new-onset comitant
convergent squint with horizontal diplopia since
early 2021. He reported unrestrained and excessive
tablet use (8 hours per day) since commencement
of the pandemic. The duration of e-learning had
doubled (to 4-5 hours) since 2020. The esotropic
deviation angle was 50 PD at both 1/3 m and 6 m on
prism cover test with glasses. Cycloplegic refraction
in July 2021 revealed myopia of -4.25 dioptres in
both eyes. Extraocular movements were full for
both eyes. Magnetic resonance imaging of the brain
was unremarkable. Acute acquired esotropia was
diagnosed. Following discussion of treatment options,
the parents opted for conservative management and
agreed to reduce their son’s screen time.
Case 3
An 8-year-old boy presented with new-onset
comitant convergent squint with horizontal diplopia
since early 2021. The patient reported unrestrained
and excessive tablet use (around 7 hours per
day) since the start of the pandemic, with 3 hours
spent on e-learning classes. Cycloplegic refraction
revealed hyperopia of +1.00 and +1.75 dioptres in
the right and left eye, respectively. There was fully
accommodative left esotropia of 50 PD at 1/3 m and
slight left esotropia 6 m without glasses and straight
alignment with glasses. Magnetic resonance imaging
of the brain showed an incidental finding of a 0.4 cm enhancing focus over the right side of the anterior
pituitary gland, unlikely to be related to the acute
esotropia. Acute acquired accommodative esotropia
was diagnosed (Fig 2).
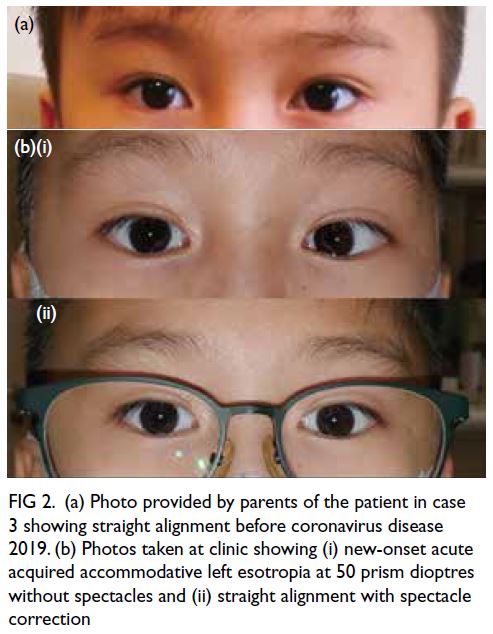
Figure 2. (a) Photo provided by parents of the patient in case 3 showing straight alignment before coronavirus disease 2019. (b) Photos taken at clinic showing (i) new-onset acute acquired accommodative left esotropia at 50 prism dioptres without spectacles and (ii) straight alignment with spectacle correction
Case 4
A 17-year-old girl with previously straight alignment presented with new-onset comitant convergent
squint causing intermittent diplopia around the
beginning of the COVID-19 outbreak. She reported
excessive smartphone use over the last 2 years for around 9 to 10 hours per day with no breaks. On
commencement of online teaching, she claimed to
spend 9 hours every day on online classes. She had
non-accommodative left eye esotropia at 30 PD
at both 1/3 m and 6 m upon prism cover test.
Subjective cycloplegic refraction revealed mild
myopia of -1.75 and -1.5 dioptres in the right and left
eye, respectively. Magnetic resonance imaging of the
brain was unremarkable. The provisional diagnosis
was acute acquired esotropia. Bilateral medial rectus
recession (right eye: 5.5 mm, left eye: 6 mm) via a
forniceal approach was performed under general
anaesthesia. At 6 months postoperatively, the angle
of deviation with glasses was 12 PD esophoria at
1/3 m and 8 PD esophoria at 6 m.
Discussion
We report four cases of acute acquired concomitant
esotropia with onset or which demonstrated
worsening development during the COVID-19
pandemic. All cases were associated with excessive
use of an electronic device corresponding to an
increased amount of time spent on e-learning.
Similar to previous case reports, the surgical
outcome of this condition was good. We believe
the prognosis should be good due to the previously
established binocularity and stereopsis in the
premorbid state and if the patient can comply with
the need to restrict screen time.
Lee et al5 proposed that acute acquired
esotropia may be precipitated by excessive near
work activity. Our cases all spent prolonged time
looking at a screen since the implementation of
online classes due to COVID-19 lockdown. The
diagnosis of acute acquired concomitant esotropia
is one of exclusion. Cycloplegic refraction is
required to exclude any accommodative element
due to refractive error. Comprehensive neurological
examination and imaging is necessary to rule out
any organic cause. Magnetic resonance imaging is
preferred due to its higher resolution for soft tissue
and lack of radiation. Surgical treatment is bilateral
medial rectus recession, titrated according to a table
of surgical numbers derived from Parks’ book6 that
lists how many mm of recession should be done for
different angles of deviation. It has been proposed
that the demand for longer durations of sustained
near viewing, ie, screen time, has increased the
risk of developing acute acquired esotropia. Several
studies worldwide have reported similar cases.1 3
Nonetheless it appears that complete abstinence
with no screen time is not feasible among children
in Hong Kong as most parents in Hong Kong
are working, which makes monitoring the use of
electronic devices at home difficult. Most schools
in Hong Kong now adopt blended online with
face-to-face teaching, even after the relaxation of
lockdown measures, to lower the infection risk for both teachers and students. As per the limitations
of all case reports, we are unable to obtain data for a
control group since e-learning for children in Hong
Kong is unavoidable.
To conclude, it is inevitable that Hong Kong
children will be exposed to excessive electronic device
usage during the worldwide pandemic, predisposing
them to esotropia. Setting a limit on screen time,
taking intermittent eye breaks, and using a larger
screen with high resolution and consequent longer
reading distance should be considered as preventive
measures.
Author contributions
Concept or design: EWH Tang.
Acquisition of data: YH Lau, EWH Tang, THT Lai.
Analysis or interpretation of data: YH Lau, EWH Tang, THT Lai.
Drafting of the manuscript: YH Lau, EWH Tang, THT Lai.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: YH Lau, EWH Tang, THT Lai.
Analysis or interpretation of data: YH Lau, EWH Tang, THT Lai.
Drafting of the manuscript: YH Lau, EWH Tang, THT Lai.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
As an editor of the journal, KKW Li was not involved in the peer review process. Other authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
All patients were treated in accordance with the Declaration of Helsinki. All patients and/or their parent/guardian provided
informed consent for all procedures and for publication.
References
1. Vagge A, Giannaccare G, Scarinci F, et al. Acute acquired concomitant esotropia from excessive application of near vision during the COVID-19 lockdown. J Pediatr Ophthalmol Strabismus 2020;57:e88-91. Crossref
2. Zhang X, Cheung SS, Chan HN, et al. Myopia incidence
and lifestyle changes among school children during the
COVID-19 pandemic: a population-based prospective
study. Br J Ophthalmol 2022;106:1772-8. Crossref
3. Mohan A, Sen P, Mujumdar D, Shah C, Jain E. Series of
cases of acute acquired comitant esotropia in children
associated with excessive online classes on smartphone
during COVID-19 pandemic; digital eye strain among kids
(DESK) study-3. Strabismus 2021;29:163-7. Crossref
4. Zhang XJ, Lau YH, Wang YM, et al. Prevalence of strabismus and its risk factors among school aged children: The Hong Kong Children Eye Study. Sci Rep 2021;11:13820. Crossref
5. Lee HS, Park SW, Heo H. Acute acquired comitant esotropia related to excessive smartphone use. BMC Ophthalmol 2016;16:37. Crossref
6. Parks MM. Atlas of strabismus surgery. Philadelphia (PA): Harper and Row Publishing; 1983.

