Hong Kong Med J 2022;28(6):430-7 | Epub 29 Nov 2022
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Neonatal mortality in singleton pregnancies: a 20-year retrospective study from a tertiary perinatal unit in Hong Kong
Genevieve PG Fung, MB BChir, MRCPCH1; SL Lau, MB, ChB, MRCOG2; Annie SY Hui, MB, ChB, MRCOG2; Sani TK Wong, MB, ChB2; WT Tse, MB, ChB, MRCOG2; PC Ng, MD, FRCPCH1; DS Sahota, PhD2; HS Lam, MD, FRCPCH1; TY Leung, MD, FRCOG2
1 Department of Paediatrics, The Chinese University of Hong Kong, Hong Kong
2 Department of Obstetrics and Gynaecology, The Chinese University of Hong Kong, Hong Kong
Corresponding author: Prof TY Leung (tyleung@cuhk.edu.hk)
Abstract
Introduction: The global neonatal death (NND) rate
has been declining in recent decades, but there are no
comprehensive data concerning the characteristics
of NNDs in Hong Kong. This study investigated the
trends and aetiologies of NNDs among singleton
pregnancies in Hong Kong.
Methods: This study included all cases of NND
from singleton pregnancies in a tertiary hospital
in Hong Kong between 2000 and 2019. The rates,
clinical characteristics, and aetiologies of NND were
compared between the first (2000-2009) and the
second (2010-2019) decades.
Results: The NND rate decreased from 1.66/1000
livebirths (97 cases) in the first decade to 1.32/1000
livebirths (87 cases) in the second decade. Congenital
or genetic abnormalities (82 cases) caused 44.6%
of all NNDs. There was a significant reduction
from 0.82/1000 livebirths in the first decade to
0.52/1000 livebirths in the second decade (P=0.037).
Other causes of NND were prematurity (69 cases;
37.5%), sepsis (16 cases; 8.7%), hypoxic-ischaemic
encephalopathy (15 cases; 8.2%), and sudden infant
death syndrome (2 cases; 1.1%). Gestational age-specific
neonatal mortality for moderately preterm
neonates (31-33 weeks of gestation) significantly
decreased from 34.73/1000 in 2000-2009 to 8.63/1000 in 2010-2019 (P=0.001), but there were no
significant changes in neonatal mortality for other
gestations.
Conclusions: The NND rate in Hong Kong is among
the lowest worldwide. Neonatal deaths in our centre
declined over the past two decades, mainly because
of improvements in the prenatal diagnosis and
treatment of congenital or genetic abnormalities, as
well as an improved survival rate among moderately
preterm neonates.
New knowledge added by this study
- The rate of neonatal mortality among singleton pregnancies in Hong Kong decreased from 1.66/1000 livebirths in 2000-2009 to 1.32/1000 livebirths in 2010-2019.
- The decline in the neonatal mortality rate mainly resulted from improvements in the prenatal diagnosis and treatment of congenital or genetic abnormalities, as well as an improved survival rate among moderately preterm neonates (31-33 weeks of gestation).
- Future improvements in the neonatal mortality rate should focus on in utero treatment, expanded carrier screening of genetic abnormalities, and the prevention of preterm birth and pre-eclampsia.
Introduction
Perinatal and neonatal mortality rates are important
measures of the quality of medical care during
pregnancy, childbirth, and the neonatal period.
Although the global neonatal death (NND) rate has
demonstrated a decreasing trend over the past 30
years, from 37/1000 livebirths to 17/1000 livebirths
between 1990 and 2020,1 NND rates considerably
vary among regions. According to the 2020 report by the World Health Organization, the NND rates
were the highest in Africa (27/1000 livebirths),
Eastern Mediterranean (25/1000 livebirths) and
South-East Asia (18/1000 livebirths); the NND rates
were the lowest in Americas (7/1000 livebirths),
Western Pacific (5/1000 livebirths) and Europe
(4/1000 livebirths).1 In Hong Kong, territory-wide
statistics indicated NND rates of 1.2/1000 and
1.0/1000 livebirths in 2004 and 2014, respectively2; these rates are lower than the rates in most regions,
according to the above report by the World Health
Organization. However, there have been few in-depth
studies concerning the trends and underlying
causes of NND in Hong Kong. Our group recently
published two epidemiological studies regarding
singleton pregnancies in Hong Kong, which revealed
a decreasing trend in the rate of stillbirths among
singleton pregnancies from 3.61/1000 in 2000-2009
to 3.09/1000 in 2010-2019.3 The rate of perinatal
mortality in multiple pregnancies also decreased
from 5.52/1000 to 4.59/1000 during the same
period.4 These improvements in mortality rates have
mainly occurred because of advances in the prenatal
diagnosis and management of fetal malformations
and genetic diseases, as well as improvements in
the antenatal management of multiple pregnancies.
The present study investigated the trends of NNDs
among singleton pregnancies in the largest tertiary
perinatal centre in Hong Kong, as well as changes
in the characteristics and aetiologies of NND over
the past two decades, with the goal of improving
perinatal care in Hong Kong.
Methods
Study setting
This retrospective study included all singleton pregnancies that delivered at the Prince of Wales
Hospital from 1 January 2000 to 31 December 2019.
The STROBE reporting guideline was followed
when writing this manuscript. The Prince of Wales
Hospital is affiliated with The Chinese University
of Hong Kong and serves a large population of
1.7 million in the New Territories East region of
Hong Kong; the hospital’s annual delivery rate is
6000 to 7000 (approximately one-sixth of the total
births in all public hospitals in Hong Kong, and one-ninth
of the total births in Hong Kong). Both the
obstetric unit and the neonatal unit are the largest
in Hong Kong. The neonatal unit is a Level III centre
that consists of a 22-bed neonatal intensive care unit
(NICU). The staff of the neonatal unit worked closely
with the staff of the obstetric unit to manage high-risk
deliveries from complicated pregnancies, as well
as pregnancies that required fetal intervention after
referral from other hospitals.
Perinatal and neonatal management
Complicated pregnancies were discussed in weekly
perinatal meetings attended by the staff of both the
obstetric unit and the neonatal unit; discussions
of these pregnancies focused on management
plans and the optimal timing of delivery. Relevant
disciplines (eg, paediatric surgery, cardiology,
neurosurgery, radiology, or otolaryngology) were
included as appropriate. In cases where a specialist
service outside of Prince of Wales Hospital (eg,
cardiothoracic surgery) was anticipated after
delivery, specialists from other centres were invited
to participate in management planning. Active
resuscitation was provided for all viable neonates
delivered at ≥24 weeks. For extremely premature
neonates with borderline viability (ie, delivered
at 22-23 weeks of gestation), considering the
high risks of mortality and long-term morbidity,
comprehensive counselling was provided to
affected families, which allowed them to select
active resuscitation or no resuscitation at birth. In
accordance with the departmental protocol, the
paediatric unit was requested to prepare for rapid
management of deliveries that involved specific
maternal or fetal conditions (eg, prematurity, fetal
distress, instrumental deliveries, and antenatally
diagnosed severe congenital abnormalities).
Neonates were managed in the NICU in accordance
with the standard unit protocols and guidelines.
These protocols were updated regularly according
to the latest evidence-based consensus guidelines
and recommendations established by clinicians
in Hong Kong and other nations. In accordance
with departmental guidelines, comprehensive
investigations were performed to determine the
cause of death in all cases of NND. All NNDs were
referred for autopsy unless the cause of death was
clearly identified (eg, trisomy 13 or 18 confirmed by genetic tests). If the cause of NND could not be
identified, the case was reported to the coroner. If
NND was caused by multiple pathologies, the most
clinically significant pathology that contributed to
death was selected for analysis.
Data collection and analysis
All cases of NND in livebirths of singleton
pregnancies during the study period were retrieved
using the Hospital Authority’s Clinical Data
Analysis and Reporting System. Cases of NND in
livebirths of multiple pregnancies were excluded.
The included cases of NND were divided into two
groups according to the decade of birth. The first
group (ie, first decade) included cases of NND
among singleton pregnancies that delivered between
1 January 2000 and 31 December 2009. The second
group (ie, second decade) included cases of NND
among singleton pregnancies that delivered between
1 January 2010 and 31 December 2019. Obstetric
data including maternal demographics (maternal
age, maternal illnesses, antenatal complications,
and treatment) and birth history (gestation, mode of
delivery, sex, birth weight, Apgar scores, and neonatal
resuscitation) were collected from the Obstetric
Specialty Clinical Information System. Neonatal
data comprising neonatal diagnoses, interventions,
and length of survival were retrieved from the
Hospital Authority’s Clinical Management System.
When further details were needed, individual case
records were retrieved for analysis.
All NNDs were categorised as early NND
(within 7 days after birth) or late NND (within
8-28 days after birth). Early, late, and total rates
of NND, as well as baseline demographics, were
compared between the two groups. Causes of death
were divided into four main categories: prematurity,
hypoxic-ischaemic encephalopathy (HIE), congenital
abnormalities, and sepsis. Congenital abnormalities
were defined by characteristic features on physical
examination, confirmed by either genetic tests,
diagnostic investigations, or autopsy. Sepsis was
defined on the basis of positive cultures established
using samples of blood, urine, cerebrospinal fluid, or
tissue from the affected neonate. Hypoxic-ischaemic
encephalopathy was diagnosed in accordance with
criteria derived from international guidelines.5
Statistical analysis
The analysis was performed using data that
overlapped with a previous study.3 Categorical
variables were compared by the Chi squared test
or Fisher’s exact test. The threshold of statistical
significance was defined as a two-sided P value of
<0.05. Data analysis was performed with the SPSS
software (Windows version 22.0; IBM Corp, Armonk
[NY], United States).
Results
Overall and gestational age-specific neonatal
mortality
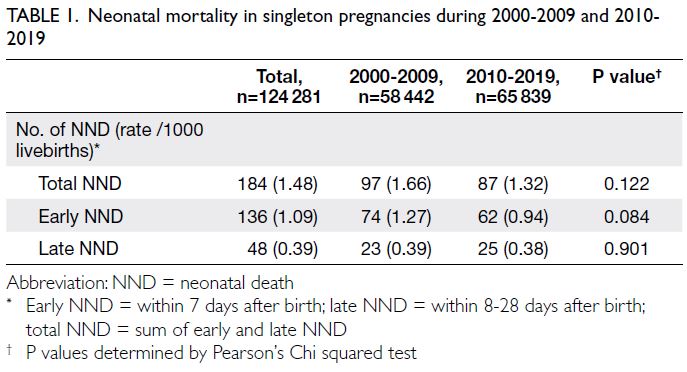
There were 124 281 livebirths from singleton
pregnancies between 2000 and 2019 (Table 1). The
number of livebirths increased by 12.7% from 58 442
in the first decade (2000-2009) to 65 839 in the
second decade (2010-2019). There were 184 NNDs
(1.48/1000 livebirths) between 2000 and 2019,
including 97 in the first decade (1.66/1000 livebirths)
and 87 in the second decade (1.32/1000 livebirths).
Overall, there were 136 cases (73.9%) of early NND
and 48 cases (26.1%) of late NND.
The maternal demographic characteristics of all
singleton pregnancies during the study period were
reported in our previous paper.3 The distribution of
gestational age among all livebirths did not differ
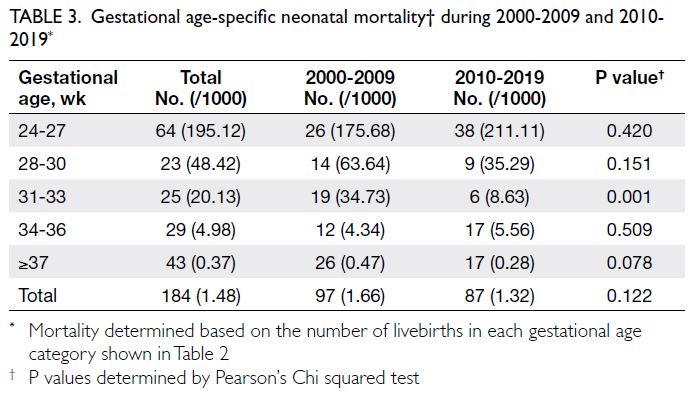
between the two decades (P=0.237) [Table 2]. The
highest rate of NND (195.12/1000 livebirths) was
observed in extremely preterm neonates (≤27 weeks
of gestation) [Table 3]. The rate of NND decreased
with increasing gestational age, such that NND
rates were 48.42/1000, 20.13/1000, 4.98/1000, and
0.37/1000 for neonates delivered at gestational ages
of 28-30 weeks, 31-33 weeks, 34-36 weeks, and
≥37 weeks, respectively. Compared with the first decade, there was a significant reduction (75.2%)
in the rate of NND among neonates delivered at
31-33 weeks of gestation during the second decade
(34.73/1000 vs 8.63/1000; P=0.001); however, there
were no significant differences in the rates of NND
among neonates in other gestational groups.
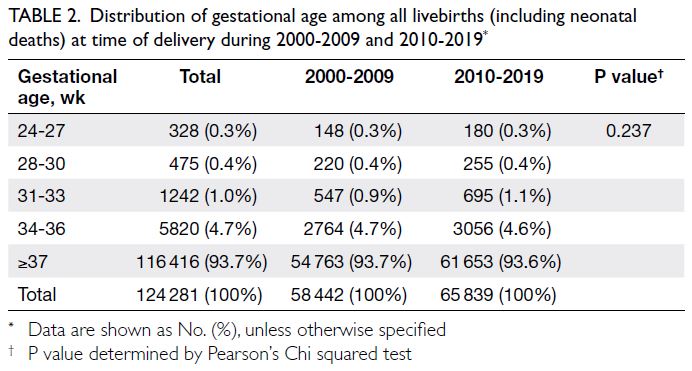
Table 2. Distribution of gestational age among all livebirths (including neonatal deaths) at time of delivery during 2000-2009 and 2010-2019
Causes of neonatal death
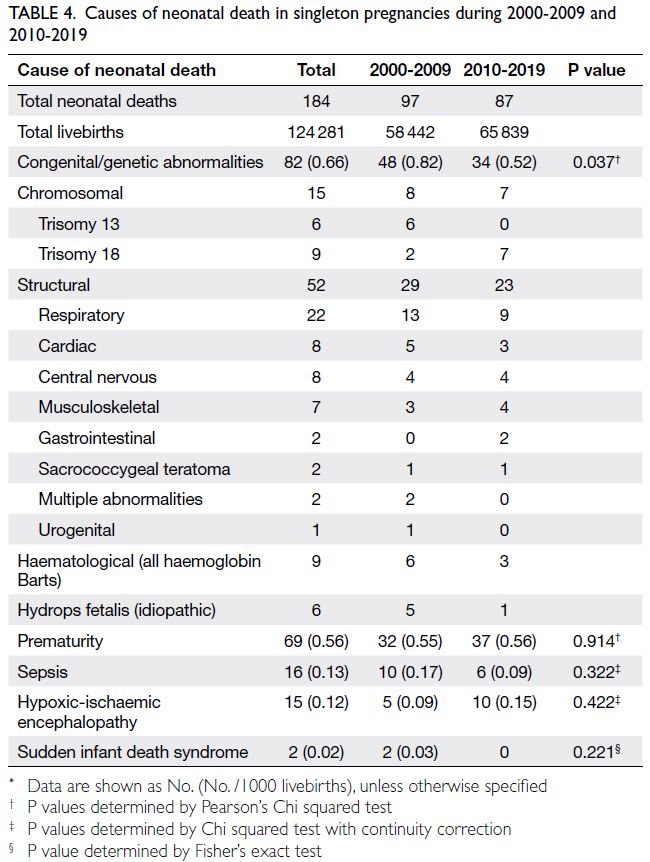
The primary causes of NND in the two decades
are shown in Table 4. Congenital or genetic
abnormalities was the most common cause of NND
(82 of 184; 44.6%) during the 20-year study period.
Other common causes of NND were prematurity
(69 cases; 37.5%), sepsis (16 cases; 8.7%), and HIE
(15 cases; 8.2%) [Supplementary Fig].
Chromosomal abnormalities caused 18.3%
(15 of 82) of NNDs related to congenital or genetic
abnormalities; all of these abnormalities were trisomy
13 or 18. Structural abnormalities caused 63.4%
(52 of 82) of NNDs related to congenital or genetic
abnormalities, and respiratory system abnormalities
were the most common causes in both decades
(22 cases). These respiratory system abnormalities
included congenital diaphragmatic hernia (13 cases),
pulmonary hypoplasia (5 cases), alveolar capillary
dysplasia (2 cases), and tracheal stenosis or atresia
(2 cases). The next most common causes were
congenital cardiac abnormalities (8 cases), including
transposition of the great arteries (2 cases), total
anomalous pulmonary venous drainage (2 cases),
endocardial cushion defect (2 cases), hypoplastic
left heart syndrome (1 case), and congenital heart
block (1 case); central nervous system abnormalities
(8 cases), including anencephaly (3 cases), central
nervous system malformation (4 cases), and brain
tumour (1 case); and musculoskeletal abnormalities
(7 cases), including fetal akinesia syndrome with
arthrogryposis (3 cases), spinal muscular atrophy
(2 cases), and skeletal dysplasia (2 cases). There were
two cases of gastrointestinal abnormalities (volvulus
and bowel atresia with meconium peritonitis), two
cases of sacrococcygeal teratoma, two cases of
multiple abnormalities, and one case of bilateral
renal agenesis (a urogenital abnormality). There
were also nine cases of haemoglobin Barts disease
and six cases of idiopathic hydrops. There was a
statistically significant decline in the rate of NND
caused by congenital or genetic abnormalities, from
0.82/1000 livebirths in the first decade to 0.52/1000
livebirths in the second decade (P=0.037).
There were no significant differences in the
rates of NND caused by prematurity, sepsis, or HIE
between the two decades. Cases of NND due to
sepsis were mainly caused by Group B Streptococcus
in the first decade and Escherichia coli in the second
decade. The majority of HIE cases (67.7%) were
related to acute intrapartum events, including
placenta abruption (5 cases), uterine rupture (2 cases),
vasa praevia (1 case), cord accident (1 case), and
chorioamnionitis (1 case).
Discussion
The NND rate in our tertiary centre is consistent with the rate of 1.2/1000 livebirths in the territory-wide
report2 and lower than the rates in many developed countries (eg, the United States, Australia, and
nations located in Europe; neonatal mortality rates
of 2-3/1000 livebirths).1 2 The global NND rate has
been decreasing over the past two decades because
of advances in perinatal care.2 Our overall NND rate
decreased by 20%, from 1.66/1000 in the first decade
to 1.32/1000 in the second decade. This decrease is
mainly the result of a decrease in NNDs related to
congenital or genetic disorders, as well as a decrease
in NNDs among neonates delivered at 31-33 weeks
of gestation.
Neonatal death due to congenital abnormalities
Similar to our previous report, which showed
a reduction in the rate of congenital or genetic
abnormality-related stillbirths,3 the present study
showed that the rate of congenital or genetic
abnormality-related NNDs decreased from
0.82/1000 livebirths in the first decade to 0.52/1000
livebirths in the second decade. This decline was
presumably because of improvements in antenatal
screening and the early detection of lethal congenital
abnormalities, which resulted in termination of
pregnancy before 24 weeks of gestation. Universal first
trimester combined screening for Down syndrome
was implemented by the Hospital Authority in
2010.6 In 2011, non-invasive cell-free fetal DNA
tests for common trisomies, as well as chromosomal
microarrays for the diagnosis of chromosomal
microdeletion syndromes, became available in the
private sector.7 8 Expanded antenatal screening of
inborn errors of metabolism was launched in the
private sector in 2013; this expanded screening has
gradually become available in the public sector since
2018.9 Although we expected a decline in the rate
of trisomy-related NNDs after universal aneuploidy
screening became available in 2011, there was an
increase in the rate of trisomy 18–related NNDs
(from 2 cases to 7 cases). A review of the individual
cases revealed that the rate of trisomy 13–related
NNDs decreased from six cases in the first decade
to none in the second decade. Conversely, five of the
seven cases of trisomy 18–related NND in the second
decade were in pregnancies that had not received
any screening; all of these five cases occurred
during the period from 2010 to 2013. The other two
cases of trisomy 18–related NND were diagnosed
during prenatal screening, but the parents chose
conservative management rather than termination
of pregnancy. To further reduce mortality associated
with hereditary genetic disorders such as spinal
muscular atrophy and fetal akinesia syndrome (which
caused NND in 5 cases), there is a need for expanded
carrier screening of parents, particularly in families
with a history of consanguineous marriage.10 11
The other main congenital abnormalities that
caused NND in our cohort were cardiorespiratory and neuromusculoskeletal disorders, among
which congenital diaphragmatic hernia was the
most common. Although survival was common
among neonates with mild to moderate congenital
diaphragmatic hernia, neonates with severe
congenital diaphragmatic hernia had a survival rate
of 10% to 20% because of pulmonary hypoplasia.
A recent large randomised controlled trial showed
that fetoscopic endoluminal tracheal occlusion
can improve the survival rate to 40% to 50%.12
In our unit, a baby survived after treatment with
fetoscopic endoluminal tracheal occlusion in 2020.13
Pulmonary hypoplasia caused by hydrothorax
or lung tumours can also be effectively and
safely treated before birth with newly designed
instruments such as the Somatex® shunt for pleuro-amniotic
shunting, and radiofrequency ablation
of the tumour feeding artery, respectively.14 15
Fetal tumours such as sacrococcygeal teratoma,
placental chorioangioma, and lung tumours remain
challenging to manage because the rapid growth of
tumours in utero increases the risk of preterm birth
and leads to impaired neonatal cardiac function.
We have demonstrated improvements in survival
after in utero embolisation of chorioangioma using
cyanoacrylate, and after in utero radiofrequency
ablation of lung sequestration.15 16 Although spinal
muscular atrophy has no cure, it can be prevented
by accurate parental carrier screening using genomic
technology and prenatal diagnosis.10
Neonatal death due to hydrops fetalis
The rate of idiopathic hydrops fetalis–related NND
decreased from 5.2% in the first decade to 1.1% in
the second decade. Advances in antenatal diagnostic
techniques in recent years have identified the
underlying causes of many conditions which may
have previously been regarded as ‘idiopathic hydrops
fetalis’.17 The early diagnosis of treatable conditions
in the antenatal period can prevent the development
of severe hydrops fetalis and subsequent NND.17 18
Intrauterine blood transfusion for fetal anaemia
and anti-arrhythmic treatment19 has significantly
reduced the rate of hydrops fetalis, resulting in
improved survival and long-term outcomes.
Neonatal death due to prematurity
Our study showed a significant (75.2%) decrease
in the rate of NND among moderately preterm
neonates (31-33 weeks of gestation) from 34.73/1000
in 2000-2009 to 8.63/1000 in 2010-2019; however,
the rate of NND did not change in other gestational
groups (Table 3). The decrease in mortality among
moderately preterm neonates could be attributed
to the implementation of multiple approaches
for the management of such neonates since 2010,
including improved ventilation strategies with
early extubation to non-invasive ventilation, new methods for surfactant administration (eg, the ‘less
invasive surfactant administration’ method), and
improvements in NICU care through continuous
quality improvement programmes. The rate of NND
among extremely preterm neonates (24-27 weeks of
gestation) was 175-211/1000, which is comparable
with the rates in other developed countries (139-326/1000).20 It is difficult to reduce the rate of NND
among extremely preterm neonates. Research is
ongoing regarding artificial placenta and womb
technology, and the results may improve the survival
of extremely preterm neonates in the future.21
The rate of prematurity-related NND can be
reduced by preventing preterm delivery; however,
this prevention remains a challenging goal. Although
our overall preterm delivery rate of 7% is lower
than the rates in other developed countries,1 22 it
has remained at this level for the past two decades,
and there has been no variations in gestation
age-specific neonatal mortality among preterm
categories. In a previous study, we demonstrated
that measurements of cervical length can help to
identify pregnant women who are at higher risk
of preterm delivery, although the risk prediction
values for Chinese women in Hong Kong are lower
than the corresponding values for women in non-Asian countries.23 Additional methods to predict the
onset of labour (eg, cervical elastography, immune
markers, and genetic markers) should be explored
to improve accuracy.24 25 Prophylactic progesterone
is effective in reducing the risk of preterm delivery
among women who have a short cervix.26 Although
the use of a cervical ring pessary reportedly had a
similar effect in a Spanish study,27 this result was
not confirmed by a randomised controlled trial
in Hong Kong28 or by subsequent meta-analysis.29
Pre-eclampsia is a common complication that
requires medically induced preterm delivery. First
trimester screening of pre-eclampsia, followed by
prophylactic aspirin treatment in high-risk cases, is a
proven strategy to effectively delay the onset of pre-eclampsia
and the associated preterm births.29 Our
recent study confirmed the accuracy of a screening
programme for pre-eclampsia.30 Reductions in pre-eclampsia–related preterm births and mortality may
be achieved by the implementation of a universal
screening programme in the future.
Neonatal death due to hypoxic ischaemic
encephalopathy
Despite advances in NICU management of HIE and
the use of therapeutic hypothermia since 2011, the
rate of HIE-related NND did not improve during
the study period. Approximately 67% of HIE-related
NNDs were caused by acute and unpredictable
perinatal events such as cord prolapse, uterine
rupture, vasa praevia, or placental abruption. We
previously reported an infant death secondary to severe cerebral palsy as a result of prolonged
shoulder dystocia, which occurred during the first
study decade.31 Therefore, team-based training for
the above perinatal events is needed to ensure that
the obstetric team can respond appropriately and
efficiently so that the risk of HIE and associated
perinatal mortality can be reduced. During these
situations that involved irreversible peripartum
hypoxia, we showed that umbilical cord arterial pH
decreased as the length of the bradycardia-to-delivery
interval increased.31 32 33 With appropriate training,
we were able to achieve a median bradycardia-to-delivery interval of 10 minutes and a median
decision-to-delivery interval of 11 minutes,32 which
was effective in preventing peripartum mortality.
Furthermore, we showed that during umbilical
cord prolapse, the knee-chest position is the most
effective approach for relieving fetal compression
of the prolapsed cord34; we also formulated an
algorithm for acute resolution of cord prolapse.35
Shoulder dystocia is associated with macrosomia,
but the optimal fetal weight cut-off for prophylactic
elective caesarean delivery has not been established.
Our previous study suggested a cut-off of 4.2 kg may
help to prevent shoulder dystocia.36 With effective
training and correct use of manoeuvres such as
posterior arm delivery, we recently showed that the
head-to-delivery interval can be shortened and the
Apgar scores can be improved.37 38 We also proposed
a modified posterior axillary sling technique to
relieve severe shoulder dystocia.39
Neonatal death due to sepsis
The rate of severe sepsis-related NND is low and has
been decreasing over the past two decades. Since the
implementation of universal Group B Streptococcus
screening and peripartum antibiotic prophylaxis in
2012, the rate of early onset Group B Streptococcus
infection has significantly decreased from 1/1000
to 0.24/1000 births.40 Despite the reduced risk of
neonatal Group B Streptococcus infection, recent
reports have shown an increase in Escherichia coli–related early-onset neonatal sepsis.41 Clinicians
should remain vigilant concerning the presence of
chorioamnionitis and risk factors for sepsis.
To our knowledge, this is the largest and most
comprehensive analysis of neonatal mortality during
a 20-year period in Hong Kong. Nevertheless, there
were a few limitations in this study. First, it was
performed in a single large centre, rather than in
a large segment of the population. Because the
Prince of Wales Hospital is the main centre for
fetal intervention in Hong Kong, many high-risk
pregnancies are referred from adjacent hospitals,
which may have led to an over-representation of
complex cases and a bias towards worse outcomes.
Second, some case details were not available for
analysis because of the retrospective nature of the study. Third, our study excluded cases of NND among
neonates with borderline viability (gestational age:
22-23 weeks and 6 days) because such NNDs are
regarded as miscarriages based on the legal definition
in Hong Kong. Although some parents of neonates
with borderline viability requested resuscitation, the
survival rate in this small group was zero according
to a recent study in our centre.42 Finally, because the
rate of NND is very low in Hong Kong, this study
could have been strengthened by including data
regarding the rates of major morbidities (eg, cerebral
palsy). Nonetheless, our findings provide a basis for
future territory-wide reviews of perinatal outcomes.
Conclusion
Hong Kong has one of the lowest rates of NND
worldwide. The neonatal mortality in our centre has
decreased from 1.66/1000 livebirths to 1.32/1000
livebirths over the past two decades, mainly because
of improvements in the prenatal diagnosis and
treatment of congenital or genetic abnormalities, as
well as an improved survival rate among moderately
preterm neonates. Future improvements should
focus on in utero treatment, expanded carrier
screening for genetic abnormalities, and the
prevention of preterm birth and pre-eclampsia.
Author contributions
Concept or design: GPG Fung, TY Leung.
Acquisition of data: All authors.
Analysis or interpretation of data: GPG Fung, TY Leung.
Drafting of the manuscript: GPG Fung, TY Leung.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: GPG Fung, TY Leung.
Drafting of the manuscript: GPG Fung, TY Leung.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
Ethical approval was obtained from the Joint Chinese
University of Hong Kong–New Territories East Cluster
Clinical Research Ethics Committee (Ref No.: CRE 2017.442).
References
1. World Health Organization. Neonatal mortality rate (0
to 27 days per 1000 live births) (SDG 3.2.2). Available from: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/67. Accessed 5 Oct 2022.
2. Hong Kong College of Obstetricians & Gynaecologists. Territory-wide audit in obstetrics & gynaecology 2014. Available from: https://www.hkcog.org.hk/hkcog/Download/Territory-wide_Audit_in_Obstetrics_Gynaecology_2014.pdf. Accessed 15 Jun 2022.
3. Wong ST, Tse WT, Lau SL, Sahota DS, Leung TY. Stillbirth
rate in singleton pregnancies: a 20-year retrospective study
from a public obstetric unit in Hong Kong. Hong Kong
Med J 2022;28:285-3. Crossref
4. Lau SL, Wong ST, Tse WT, et al. Perinatal mortality rate in
multiple pregnancies: a 20-year retrospective study from
a tertiary obstetric unit in Hong Kong. Hong Kong Med J
2022;28:347-56. Crossref
5. Executive summary: Neonatal encephalopathy and neurologic outcome, second edition. Report of the
American College of Obstetricians and Gynecologists’
Task Force on Neonatal Encephalopathy [editorial]. Obstet
Gynecol 2014;123:896-901. Crossref
6. Sahota DS, Leung WC, Chan WP, To WW, Lau ET, Leung TY. Prospective assessment of the Hong Kong
Hospital Authority universal Down syndrome screening
programme. Hong Kong Med J 2013;19:101-8.
7. Chan YK, Leung WC, Leung TY, et al. Women’s preference
for non-invasive prenatal DNA testing versus chromosomal
microarray after screening for Down syndrome: a
prospective study. BJOG 2018;125:451-9. Crossref
8. Hui AS, Chau MH, Chan YM, et al. The role of chromosomal
microarray analysis among fetuses with normal karyotype
and single system anomaly or nonspecific sonographic
findings. Acta Obstet Gynecol Scand 2021;100:235-43. Crossref
9. Chong SC, Law LK, Hui J, Lai CY, Leung TY, Yuen YP.
Expanded newborn metabolic screening programme
in Hong Kong: a three-year journey. Hong Kong Med J
2017;23:489-96. Crossref
10. Chan OY, Leung TY, Cao Y, et al. Expanded carrier
screening using next-generation sequencing of 123 Hong
Kong Chinese families: a pilot study. Hong Kong Med J
2021;27:177-83. Crossref
11. Siong KH, Au Yeung SK, Leung TY. Parental consanguinity
in Hong Kong. Hong Kong Med J 2019;25:192-200. Crossref
12. Deprest JA, Nicolaides KH, Benachi A, et al. Randomized
trial of fetal surgery for severe left diaphragmatic hernia. N
Engl J Med 2021;385:107-18. Crossref
13. TOPick. 3次流產40歲婦終懷孕胎兒27周時橫膈膜穿洞威爾斯婦產科團隊施宮內手術力保胎兒順利出世. Available
from: https://topick.hket.com/article/2757416. Accessed
15 Jun 2022.
14. Chung MY, Leung WC, Tse WT, et al. The use of Somatex Shunt for fetal pleural effusion: a cohort of 8 procedures.
Fetal Diagn Ther 2021;48:440-7. Crossref
15. Tse WT, Poon LC, Wah YM, Hui AS, Ting YH, Leung TY.
Bronchopulmonary sequestration successfully treated with
prenatal radiofrequency ablation of the feeding artery.
Ultrasound Obstet Gynecol 2021;58:325-7. Crossref
16. Cheng YK, Yu SC, So PL, Leung TY. Ultrasound-guided
percutaneous embolisation of placental chorioangioma
using cyanoacrylate. Fetal Diagn Ther 2017;41:76-9. Crossref
17. Swearingen C, Colvin ZA, Leuthner SR. Nonimmune hydrops fetalis. Clin Perinatol 2020;47:105-21. Crossref
18. Songdej D, Babbs C, Higgs DR; BHFS International Consortium. An international registry of survivors with
Hb Bart’s hydrops fetalis syndrome. Blood 2017;129:1251-9. Crossref
19. Donofrio MT, Moon-Grady AJ, Hornberger LK, et al. Diagnosis and treatment of fetal cardiac disease: a scientific statement from the American Heart Association.
Circulation 2014;129:2183-242. Crossref
20. Ancel PY, Goffinet F; EPIPAGE-2 Writing Group, et al.
Survival and morbidity of preterm children born at 22
through 34 weeks’ gestation in France in 2011: results of
the EPIPAGE-2 cohort study. JAMA Pediatr 2015;169:230-8. Crossref
21. De Bie FR, Davey MG, Larson AC, Deprest J, Flake AW.
Artificial placenta and womb technology: past, current,
and future challenges towards clinical translation. Prenat
Diagn 2021;41:145-58. Crossref
22. Hui AS, Lao TT, Leung TY, Schaaf JM, Sahota DS. Trends
in preterm birth in singleton deliveries in a Hong Kong
population. Int J Gynaecol Obstet 2014;127:248-53. Crossref
23. Leung TN, Pang MW, Leung TY, Poon CF, Wong SM,
Lau TK. Cervical length at 18-22 weeks of gestation for the
prediction of spontaneous preterm delivery in Hong Kong
Chinese women. Ultrasound Obstet Gynecol 2005;25:713-7. Crossref
24. Feng Q, Chaemsaithong P, Duan H, et al. Screening for
spontaneous preterm birth by cervical length and shear-wave
elastography in the first trimester of pregnancy. Am J
Obstet Gynecol 2022;227:500.e1-14. Crossref
25. Chim SS, Lee WS, Ting YH, Chan OK, Lee SW, Leung TY.
Systematic identification of spontaneous preterm birth-associated
RNA transcripts in maternal plasma. PLoS One
2012;7:e34328. Crossref
26. Romero R, Nicolaides KH, Conde-Agudelo A, et al.
Vaginal progesterone decreases preterm birth ≤34 weeks
of gestation in women with a singleton pregnancy and a
short cervix: an updated meta-analysis including data
from the OPPTIMUM study. Ultrasound Obstet Gynecol
2016;48:308-17. Crossref
27. Goya M, Pratcorona L, Merced C, et al. Cervical pessary
in pregnant women with a short cervix (PECEP): an open-label
randomised controlled trial. Lancet 2012;379:1800-6. Crossref
28. Hui SY, Chor CM, Lau TK, Lao TT, Leung TY. Cerclage
pessary for preventing preterm birth in women with a
singleton pregnancy and a short cervix at 20 to 24 weeks: a
randomized controlled trial. Am J Perinatol 2013;30:283-8. Crossref
29. Conde-Agudelo A, Romero R, Nicolaides KH. Cervical
pessary to prevent preterm birth in asymptomatic high-risk
women: a systematic review and meta-analysis. Am J
Obstet Gynecol 2020;223:42-65.e2. Crossref
30. Chaemsaithong P, Pooh RK, Zheng M, et al. Prospective
evaluation of screening performance of first trimester prediction models for preterm preeclampsia in Asian
population. Am J Obstet Gynecol 2019;221:650.e1-16. Crossref
31. Leung TY, Stuart O, Sahota DS, Suen SS, Lau TK, Lao TT.
Head-to-body delivery interval and risk of fetal acidosis and
hypoxic ischaemic encephalopathy in shoulder dystocia: a
retrospective review. BJOG 2011;118:474-9. Crossref
32. Leung TY, Chung PW, Rogers MS, Sahota DS, Lao TT,
Chung TK. Urgent cesarean delivery for fetal bradycardia.
Obstet Gynecol 2009;114:1023-8. Crossref
33. Wong L, Tse WT, Lai CY et al. Bradycardia-to-delivery
interval and fetal outcomes in umbilical cord prolapse.
Acta Obstet Gynecol Scand 2021;100:170-7. Crossref
34. Kwan AH, Chaemsaithong P, Wong L, et al. Transperineal
ultrasound assessment of fetal head elevation by maneuvers
used for managing umbilical cord prolapse. Ultrasound
Obstet Gynecol 2021;58:603-8. Crossref
35. Wong L, Kwan AH, Lau SL, Sin WT, Leung TY. Umbilical
cord prolapse: revisiting its definition and management.
Am J Obstet Gynecol 2021;225:357-66. Crossref
36. Cheng YK, Lao TT, Sahota DS, Leung VK, Leung TY. Use
of birth weight threshold for macrosomia to identify fetuses
at risk of shoulder dystocia among Chinese populations.
Int J Gynaecol Obstet 2013;120:249-53. Crossref
37. Chan EH, Lau SL, Leung TY. Changes in the incidence
and management of shoulder dystocia over 20 years from
a tertiary obstetric unit in Hong Kong. Hong Kong Med J. In press.
38. Leung TY, Stuart O, Suen SS, Sahota DS, Lau TK, Lao TT.
Comparison of perinatal outcomes of shoulder dystocia
alleviated by different type and sequence of manoeuvres: a
retrospective review. BJOG 2011;118:985-90. Crossref
39. Kwan AH, Hui AS, Lee JH, Leung TY. Intrauterine fetal
death followed by shoulder dystocia and birth by modified
posterior axillary sling method: a case report. BMC
Pregnancy Childbirth 2021;21:672. Crossref
40. Ma TW, Chan V, So CH, et al. Prevention of early onset
group B streptococcal disease by universal antenatal
culture-based screening in all public hospitals in Hong
Kong. J Matern Fetal Neonatal Med 2018;31:881-7. Crossref
41. Stoll BJ, Puopolo KM, Hansen NI, et al. Early-onset
neonatal sepsis 2015 to 2017, the rise of Escherichia coli,
and the need for novel prevention strategies. JAMA Pediatr
2020;174:e200593. Crossref
42. Hon KL, Liu S, Chow JC, et al. Mortality and morbidity
of extremely low birth weight infants in Hong Kong,
2010-2017: a single-centre review. Hong Kong Med J
2018;24:460-5. Crossref