Hong Kong Med J 2022 Oct;28(5):411-2 | Epub 30 Jun 2022
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
COMMENTARY
Helping a patient with suicidal ideation: an
ethical perspective
Season HL Ho, BSc Applied Sciences (Health Studies); Ben YF Fong, MPH (Syd), FHKAM (Community Medicine)
Division of Science, Engineering and Health Studies, College of Professional and Continuing Education, The Hong Kong Polytechnic University, Hong Kong
Corresponding author: Ms Season HL Ho (hiulamseasonho@gmail.com)
“To be or not to be” is a well-known monologue from Shakespeare’s play Hamlet. The monologue
reflects the internal mental conflicts that many
people face in complex situations. Although we
are not all protagonists of a play, everyone faces
plenty of ethical dilemmas in their daily life. Ethical
dilemma occurs when a moral problem involving
two or more mutually exclusive, morally correct
actions.1 Indeed, healthcare practitioners also face
plenty of ethical dilemmas in practice. It is crucial
for healthcare practitioners to have a mindset that
is legal, ethical, and socially responsible,2 because
their decisions influence the outcome. Very often
healthcare practitioners and patients have different
perspectives of views on the same issue. Bioethics
is a set of moral principles that practitioners should
follow, but these principles can conflict with patient
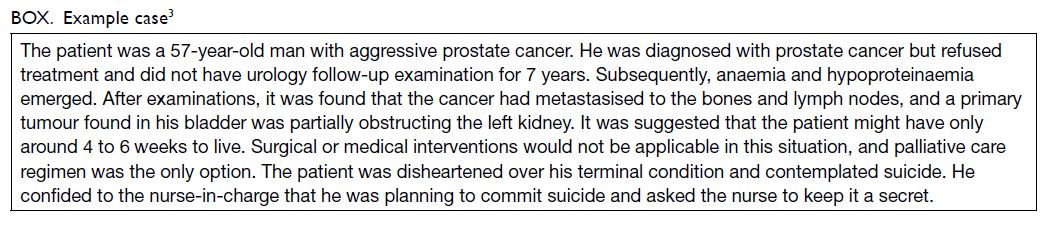
autonomy. An example case3 has been selected from
the literature because it provides an example of a
common encounter of ethical dilemma in clinical
practice (Box).
Autonomy or beneficence
The patient in this example (Mr X) unintentionally
placed the nurse in an ethical dilemma. When Mr
X disclosed the suicidal ideation (SI), the nurse had
two morally correct choices: conceal the truth or
report the SI. Concealing the truth would respect the
patient’s autonomy; however, this violates the code
of ethics for nurses. Reporting the SI to members
of the team not providing direct care to the patient
would comply with the beneficence principle, or
‘duty to warn’. This principle is an obligation for
healthcare practitioners to warn the potential victim if a patient reports an intention to cause imminent
danger or harm. However, reporting the SI would
violate the patient’s autonomy and breach patient
confidentiality, and this is particularly so in the
Hong Kong setting. The dichotomy between patient
autonomy and beneficence leads to a dilemma.
Neither can be chosen without violating the other.
Autonomy refers to the right of the patient
to make independent decisions for their care.
Healthcare professionals should respect patient
decisions without influencing or interrupting.4
Beneficence is the obligation of healthcare
professionals to act for the benefit of the patient
and to remove conditions that cause harm,5 and to
enhance patient health and well-being. In addition
to these two principles, non-maleficence should also
be considered. Non-maleficence is the obligation
of healthcare professionals to ‘do no harm’ to the
patient through negligence.6
It is a sophisticated decision to choose between
autonomy and the beneficence. Placing a priority on
identifying whether Mr X had the ability to make
an appropriate decision was required. Patients
with cancer are more likely to have very strong
psychological reactions, including suicide attempts7
or making “irresponsible” decisions that induce
severe consequences. In this situation, healthcare
professionals must override patient autonomy.8
Mental assessment and physical examination can
identify whether the patient can make informed
and appropriate decisions. If mental disorders
or unstable emotional conditions are diagnosed,
practitioners must guide them back to the right track
by good clinical practice and offer coordinated care.
To avoid unnecessary harm, the nurse should pick beneficence and non-maleficence in this situation.
Choosing to conceal the secret would satisfy
Mr X but could lead to traumatic consequences for
Mr X’s family and potentially even the healthcare
providers involved. Choosing to tell the truth would
satisfy his family and healthcare providers. The
family members could spend more time with Mr X,
and the healthcare providers could fulfil their duty.
Therefore, reporting the secret is considered the
more ethical choice, despite going against the wishes
of the patient.
Evaluation and treatment of
patients with suicidal ideation
Some patients with terminal illnesses have the desire for hastened death, and some request assisted suicide
or exhibit signs of suicidal ideation (SI).9 Suicidal
ideation is correlated with psychiatric disorders
that adversely affect the patient’s emotional and
psychological behaviour.10 Patients with cancer have
higher prevalence of psychiatric disorders.11 Despite
the high prevalence, <50% of cancer patients with
psychiatric disorders are identified and assigned
the appropriate care.11 Thus, it was fortunate that
Mr X was willing to express SI to the nurse. Symptom
assessments and psychological care in palliative care
are warranted. The patient’s psychiatric symptoms or
stressors should be identified before they manifest.
Patients with end-of-life illnesses often
experience severe pain and anxiety, leading to
psychological distress. However, psychological
support is insufficient in most cases. Under the
intense working environment in the medical ward,
medical practitioners often focus more on clinical
treatments rather than supportive care such as
recognising the patient’s needs and relieving the
anxiety of the patient and their family. Furthermore,
management and training in palliative care and end-of-life care are often neglected in medical education,12
and this remains the case in Hong Kong. Psychiatric
symptoms or even SI are often overlooked.
There are noticeable differences between
common clinical care and palliative care, which
is more holistic. In addition to the traditional
components of clinical assessment, palliative
care includes four unique domains: physical,
psychological, social and family, and spiritual.
Clinical knowledge and skills are the focus of medical
training programmes, but the beliefs and values that
underpin professional medical practice are seldom
addressed. Owing to societal norms in Hong Kong,
patients are reluctant to discuss the topic of “dying”
openly with their physicians. Gaps are found in
medical assessment in palliative care patients.13 To
alleviate the issue, more training in palliative care,
end-of-life issues, and ethical principles, should be
included in the curriculum for medical training.
Palliative care is patient- and family-centred care.14 Families and family caregivers can play a significant role in providing support
and encouragement. This can help the patients
to redefine themselves, and eventually improve
their physical status and intrapersonal features.
Furthermore, patients are more willing to talk with
family members instead of practitioners, improving
the possibility of identifying any abnormalities in the
patient’s mental and physical condition.
Conclusion
Practitioners’ decisions and actions affect patients’ lives and care. It is important for practitioners to assess which action is most appropriate for
the situation, even where there are two or more
morally correct approaches. Practitioners must be
responsible for the choices they make, and should
refer the patient to relevant services to support their
decisions. They should refer to and analyse the code
of ethics and related literature before making ethical
decisions.
Author contributions
Concept or design: Both authors.
Acquisition of data: SHL Ho.
Analysis or interpretation of data: Both authors.
Drafting of the manuscript: SHL Ho.
Critical revision of the manuscript for important intellectual content: Both authors.
Acquisition of data: SHL Ho.
Analysis or interpretation of data: Both authors.
Drafting of the manuscript: SHL Ho.
Critical revision of the manuscript for important intellectual content: Both authors.
Both authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
Both authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
1. Chandra S, Mohammadnezhad M, Ward P. Trust and communication in a doctor- patient relationship: a
literature review. J Healthc Commun 2018;3:36. Crossref
2. Mujtaba BG, Cavico FJ, Nonet G, Rimanoczy I, Samuel M. Developing a legal, ethical, and socially responsible mindset for business leadership. Adv Soc Sci Res J 2015;2:9-26. Crossref
3. Jie L. The patient suicide attempt—an ethical dilemma case study. Int J Nurs Sci 2015;2:408-13. Crossref
4. Varkey B. Principles of clinical ethics and their application to practice. Med Princ Pract 2021;30:17-28. Crossref
5. Pandit MS, Pandit S. Medical negligence: coverage of the profession, duties, ethics, case law, and enlightened defense—a legal perspective. Indian J Urol 2009;25:372-8. Crossref
6. Southern New Hampshire University. Why ethics in
nursing matters. Available from: https://www.snhu.edu/about-us/newsroom/2018/05/ethics-in-nursing. Accessed 21 Sep 2021.
7. Howard OM, Fairclough DL, Daniels ER, Emanuel EJ. Physician desire for euthanasia and assisted suicide:
would physicians practice what they preach? J Clin Oncol
1997;15:428-32. Crossref
8. Loewy EH. Beneficence in trust. Hastings Cent Rep 1989;19:42-3. Crossref
9. Goelitz A. Suicidal ideation at end-of-life: the palliative care team’s role. Palliat Support Care 2003;1:275-8. Crossref
10. Salters-Pedneault K. Types of psychiatric disorders.
Available from: https://www.verywellmind.com/psychiatric-disorder-definition-425317. Accessed 21 Sep
2021.
11. Rivest J, Levenson J. Clinical features and diagnosis of psychiatric disorders in patients with cancer: overview. Available from: https://www.uptodate.com/contents/clinical-features-and-diagnosis-of-psychiatric-disorders-in-patients-with-cancer-overview. Accessed 21 Sep 2021.
12. Woo JA, Maytal G, Stern TA. Clinical challenges to the delivery of end-of-life care. Prim Care Companion J Clin Psychiatry 2006;8:367-72.
13. Lam WM. Palliative care in Hong Kong—past, present and future. HK Pract 2019;41:39-46.
14. Steele R, Davies B. Supporting families in palliative
care. Oxford Medicine Online. Available from:
https://oxfordmedicine.com/view/10.1093/med/9780190244132.001.0001/med-9780190244132-chapter-3. Accessed 21 Sep 2021.