Hong Kong Med J 2022 Oct;28(5):347-56 | Epub 5 Sep 2022
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE CME
Perinatal mortality rate in multiple pregnancies:
a 20-year retrospective study from a tertiary obstetric unit in Hong Kong
SL Lau, MB, ChB, MRCOG1; Sani TK Wong, MB, ChB1; WT Tse, MB, ChB, MRCOG1; Genevieve PG Fung, MB BChir, MRCPCH2; Hugh Simon Lam, MD, FRCPCH2; Daljit Singh Sahota, PhD; TY Leung, MD, FRCOG1
1 Department of Obstetrics and Gynaecology, The Chinese University of Hong Kong, Hong Kong
2 Department of Paediatrics, The Chinese University of Hong Kong, Hong Kong
Corresponding author: Prof TY Leung (tyleung@cuhk.edu.hk)
Abstract
Introduction: Multiple pregnancies have become
more common, but their perinatal mortality rate
remains higher than the rate among singleton
pregnancies. This retrospective study investigated
the prevalence and causes of perinatal mortality
among multiple pregnancies in Hong Kong.
Methods: All multiple pregnancies in a university
tertiary obstetric unit between 2000 and 2019
were reviewed, and the medical records of cases
complicated by stillbirth and neonatal death were
identified. The causes of perinatal mortality were
determined based on clinical assessment and
laboratory results, then compared between the first
(2000-2009) and second (2010-2019) decades.
Results: The prevalence of multiple pregnancies
increased from 1.41% in the first decade to 1.91%
in the second decade (P<0.001). Compared with the
first decade, the second decade had a lower stillbirth
rate (14.72 vs 7.68 [both per 1000 births]; P=0.026),
late neonatal death rate (4.78 vs 1.16 [both per
1000 livebirths]; P=0.030), and total mortality rate
(25.32 vs 13.82 [both per 1000 births]; P=0.006). The
decline in stillbirth rate was related to improvements
in antenatal care and treatment. The decline in the late neonatal death rate was related to a reduction
in preterm birth before 34 weeks (18.5% vs 15.2%;
P=0.006), as well as an improvement in the mortality
rate in the subgroup of 31-33 weeks (19.23 vs 0 [both
per 1000 livebirths]; P=0.035).
Conclusion: Although the prevalence of multiple pregnancies increased during the study period,
the corresponding total perinatal mortality rate improved by 45.4%.
New knowledge added by this study
- The prevalence of multiple pregnancies increased from 1.41% in 2000-2009 to 1.91% in 2010-2019, but the total perinatal mortality rate decreased by 45.4% (from 25.32 per 1000 births to 13.82 per 1000 births).
- The stillbirth rate decreased from 14.72 per 1000 births to 7.68 per 1000 births because of close antenatal ultrasonographic monitoring, as well as fetal intervention including fetoscopic laser coagulation.
- The late neonatal death rate decreased from 4.78 per 1000 births to 1.16 per 1000 births because of a reduction in the rate of preterm deliveries before 34 weeks of gestation, as well as improvements in intensive neonatal care that increased the survival rate for babies delivered at 31-33 weeks of gestation.
- Designated regular ultrasonography examinations and antenatal clinical examinations, beginning in the first trimester, are essential for reducing perinatal mortality in multiple pregnancies (particularly when a monochorionic placenta is present).
- Territory-wide monitoring of perinatal mortality is needed to maintain the standard of perinatal care in Hong Kong.
Introduction
The global prevalence of multiple pregnancies has been increasing since the introduction of assisted
reproductive technology in 1978.1 However, the
risk of perinatal mortality is four-fold to seven-fold
higher in twin pregnancies than in singleton
pregnancies; this risk is further increased in triplet and quadruplet pregnancies.2 3 In particular, multiple
pregnancies with a monochorionic (MC) component
are at greater risk, compared with multiple
pregnancies that lack a MC component.4 5 Preterm
deliveries, selective fetal growth restriction, twin-to-twin
transfusion syndrome (TTTS), and congenital
anomalies are responsible for the higher rate of perinatal mortality in multiple pregnancies.2 6 7 8 In
the UK, the Confidential Enquiry into Maternal and
Child Health and Perinatal Mortality Surveillance
Report for Births showed that the stillbirth (SB)
rate for twin pregnancies had decreased from 17.58
per 1000 total births in 2000 to 6.16 per 1000 total
births in 2016, whereas the SB rate for singleton
pregnancies remained unchanged. Moreover, the
neonatal mortality for twin pregnancies decreased
from 23.2 to 5.34 per 1000 livebirths for the same
period of time.9 10 These changes can presumably be
attributed to the 2011 implementation of national
guidelines in the UK11 concerning structured and
more intensive antenatal monitoring; the guidelines
emphasise the use of ultrasonography to determine
chorioamnionicity and clarify the gestational
age prior to delivery in uncomplicated multiple
pregnancies.12
To our knowledge, no Hong Kong–specific
data are available regarding the trends and causes
of perinatal mortality in multiple pregnancies. We
recently reported the improvement of perinatal
mortality in singleton pregnancies at a tertiary
centre in Hong Kong between 2000 and 2019.13
In the present study, we aimed to assess changes
in the rates of perinatal mortality in multiple
pregnancies, their underlying causes, and trends
between 2000 and 2019 in the same obstetric unit,
which is a referral centre for complicated multiple
pregnancies.
Methods
Study setting
This study comprised a sub-analysis of our
retrospective investigation of perinatal mortality in
Prince of Wales Hospital, Hong Kong, over a 20-year
period from 1 January 2000 to 31 December 2019,
with a focus on multiple pregnancies. The hospital
serves a population of approximately 1.7 million
in the New Territories East region of Hong Kong,
with an annual delivery rate of around 6000-7000
(approximately one-sixth of all births in all public
hospitals, and one-ninth of all births in Hong Kong).
Furthermore, the obstetric unit is a tertiary centre
that receives complicated multiple pregnancies
referred from other hospitals; it also serves as a
maternal fetal medicine training centre accredited
by both The Royal College of Obstetricians and
Gynaecologists (RCOG; https://www.rcog.org.uk)
and The Hong Kong College of Obstetricians and
Gynaecologists (HKCOG; www.hkcog.org.hk). The
STROBE reporting guideline was followed when
writing this manuscript.
Data collection and analysis
Records of all multiple pregnancies delivered at the study hospital were retrieved from the hospital
database. Multiple pregnancies were defined as
pregnancies in which >1 fetus remained alive in utero
by 24 weeks of gestation. Thus, the final pregnancy
order was defined according to the number of live
fetuses at 24 weeks. For example, if a twin was lost
before 24 weeks of gestation because of spontaneous
in utero death or fetal reduction, such that only one
fetus remained alive at 24 weeks, the pregnancy was
considered singleton. In contrast, if a twin was lost at
26 weeks of gestation and the co-twin was delivered
at 37 weeks, the pregnancy was considered a twin
pregnancy with one in utero fetal death. Because the
delivery of a dead fetus might have been deferred
until the delivery of its live co-fetus, the definition
of the time of in utero fetal death or SB was based
on the timing of death, rather than the timing of
delivery. Stillbirth was defined as fetal death that
occurred at or after 24 weeks of gestation; late SB
was defined as fetal death that occurred at or after
28 weeks. Neonatal death (NND) was defined as
the death of a livebirth and was subcategorised into
early (death within 7 days after birth) and late (death
between 8 and 28 days after birth).
Statistical analysis
The SB rate was calculated as the number of SBs divided by the total number of births (SBs and
livebirths after 24 weeks). Early, late, and total
(early plus late) NND rates were calculated as the
number of NNDs in a specific period divided by
the total number of livebirths (excluding SBs). The perinatal mortality rate was calculated as the sum
of SBs and early NNDs divided by the total number
of births. Continuous variables were compared by
independent samples t tests or the Mann-Whitney
U test for parametric and non-parametric data,
respectively. For comparisons of risk factors, 95%
confidence intervals of the differences or odds
ratios were included. Categorical variables were
compared by the Chi squared test or Fisher’s exact
test, as appropriate. The level of significance was set
at a two-sided P value of <0.05. Data analysis was
performed with SPSS (Windows version 22.0; IBM
Corp, Armonk [NY], United States).
Results
Multiple pregnancy types, prevalences, and
mortalities
During the 20-year study period, there were 2126
multiple pregnancies, including 2077 (97.7%) twin
pregnancies, 48 (2.26%) triplet pregnancies, and
one (0.05%) quadruplet pregnancy; the quadruplet
pregnancy was quadrachorionic quadra-amniotic.
Among the twin pregnancies, 1377 (66.3%)
were dichorionic-diamniotic, 670 (32.3%) were
monochorionic-diamniotic, and 21 (1.0%) were
monochorionic-monoamniotic; chorioamnionicity
in the remaining nine (0.4%) was unknown. Among
the triplet pregnancies, 25 (52.1%) were trichorionic-triamniotic;
the remaining 23 (47.9%) triplet
pregnancies had ≥1 MC component, including 14
dichorionic-triamniotic, seven monochorionic-triamniotic,
one monochorionic-diamniotic, and
one dichorionic-diamniotic. Thus, among 4302 total
births from multiple pregnancies, 1451 (33.7%) were
from 714 pregnancies with a MC component, 2833
(65.9%) [including the quadruplets] were from 1403
pregnancies without a MC component, and 18 (0.4%)
were from the nine twin pregnancies of uncertain chorioamnionicity.
The prevalence of multiple pregnancies
increased from 1.41% (837 per 59 469 pregnancies)
in the first decade to 1.91% (1289 per 67 316
pregnancies) in the second decade (P<0.001). This
change was caused by increases in both MC multiple
pregnancies (from 309 [0.52%] to 405 [0.60%]) and
non-MC multiple pregnancies (from 519 [0.87%] to
884 [1.31%]) between the first and second decades;
the increase in non-MC multiple pregnancies was
greater. The nine twin pregnancies with unknown
chorioamnionicity were all delivered in the first
decade.
Overall, there were 45 SBs, 23 early NNDs,
and 11 late NNDs during the study period (Table 1).
Among the 45 SBs in multiple pregnancies, 21
(46.7%) occurred between 24 and 27 weeks of
gestation, whereas 24 (53.3%) occurred thereafter;
the late SB rate was 5.71 per 1000 births. Forty-three
SBs (10.35 per 1000 births) occurred in twin
pregnancies (including five double SBs: four pairs
of monochorionic-diamniotic twins and one pair
of dichorionic diamniotic twins), whereas two
SBs (13.89 per 1000 births) occurred in triplet
pregnancies; these SB rates did not significantly
differ. Furthermore, there were 28 NNDs (6.81 per
1000 births) in twin pregnancies and six NNDs
(42.25 per 1000 births) in triplet pregnancies;
the NND rate was significantly higher in triplet
pregnancies (P=0.001). Therefore, the total mortality
rate (17.09 per 1000 births vs 55.56 per 1000 births;
P=0.005) and the perinatal mortality rate (14.93 per
1000 births vs 41.67 per 1000 births; P=0.025) were
both higher in triplet pregnancies (Table 1). There
were no instances of perinatal mortality in the only
case of quadruplet pregnancy or in the nine twin
pregnancies of unknown chorioamnionicity.
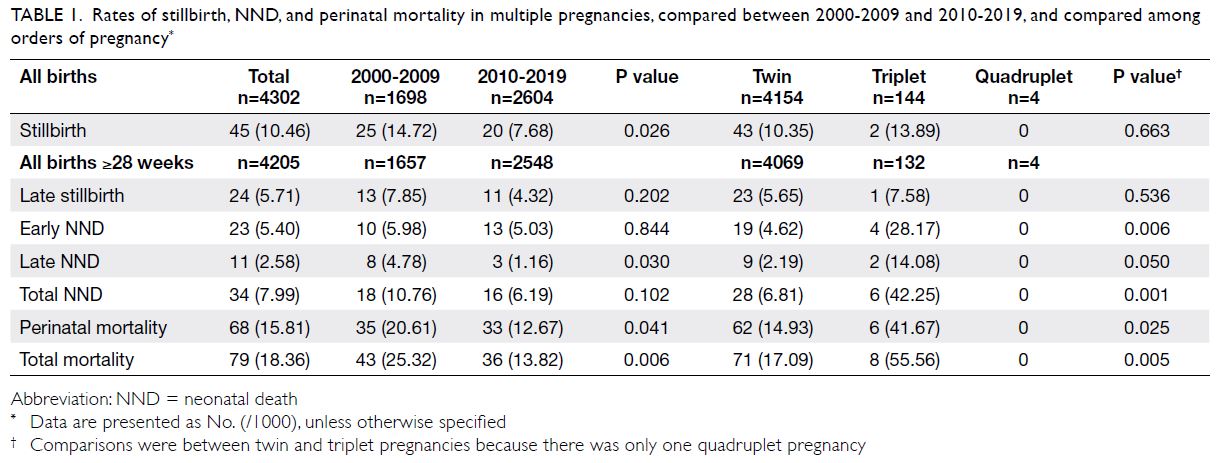
Table 1. Rates of stillbirth, NND, and perinatal mortality in multiple pregnancies, compared between 2000-2009 and 2010-2019, and compared among orders of pregnancy
Among the twin pregnancies, the MC group
had significantly higher rates of SB (18.81 per 1000 births vs 6.17 per 1000 births; P<0.001) compared
with the non-MC group, but the early, late and total
NND rates did not differ between groups. Overall,
the MC twin group had higher rates of total mortality
(28.94 per 1000 births vs 11.26 per 1000 births;
P<0.001) and perinatal mortality (24.60 per 1000
births vs 10.17 per 1000 births; P<0.001), compared
with the non-MC twin group. Among the triplet
pregnancies, the MC group also had significantly
higher rates of total NND (88.24 per 1000 births vs 0;
P=0.011) and total mortality (101.45 per 1000 births
vs 13.33 per 1000 births; P=0.028) [Table 2].
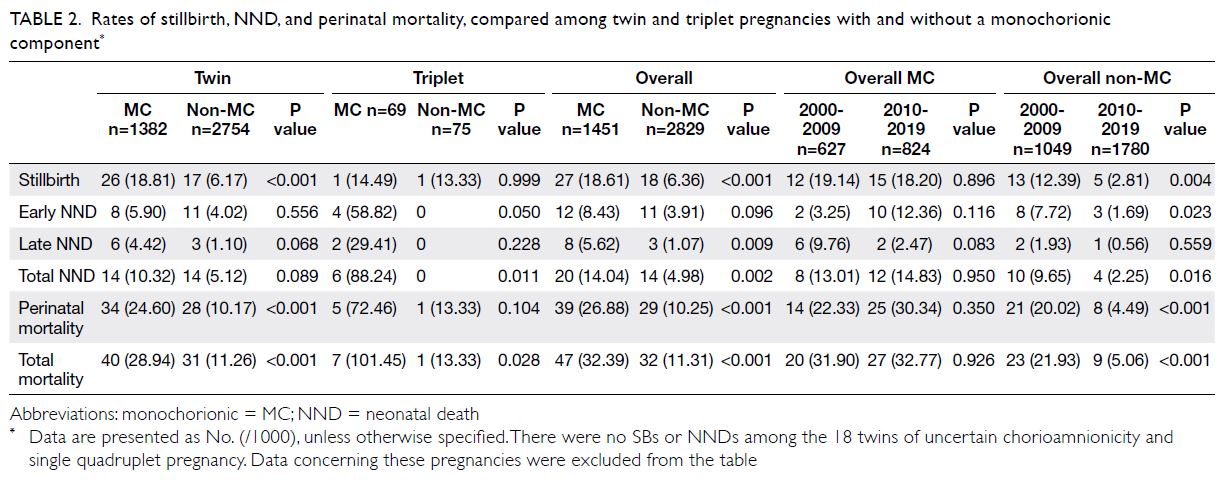
Table 2. Rates of stillbirth, NND, and perinatal mortality, compared among twin and triplet pregnancies with and without a monochorionic component
Changes in stillbirth and neonatal death rates
during the study period
The following rates were significantly lower in the
second decade, compared with the first decade:
overall SB (14.72 per 1000 births vs 7.68 per 1000
births; P=0.026), late NND (4.78 per 1000 births vs
1.16 per 1000 births; P=0.030), perinatal mortality
(20.61 per 1000 births vs 12.67 per 1000 births;
P=0.041) and total mortality (25.32 per 1000 births
vs 13.82 per 1000 births; P=0.006) [Table 1]. Notably,
the rates of early NND and total NND did not
significantly differ between decades. In the non-MC
group, the following rates were significantly lower in
the second decade: overall SB (12.39 per 1000 births
vs 2.81 per 1000 births; P=0.004), early NND (7.72
per 1000 births vs 1.69 per 1000 births; P=0.023),
and total NND (9.65 per 1000 births vs 2.25 per 1000
births; P=0.016). No differences between decades
were observed in the MC group (Table 2).
Details of stillbirths in multiple pregnancies
The maternal characteristics associated with SBs in
multiple pregnancies are shown in Supplementary
Table 1 of the Appendix. Compared with the
livebirth group (excluding cases with NND), mothers in the SB group were significantly younger
(30.3 ± 6.6 years vs 32.7 ± 5.3 years; P=0.004) and
the proportion of mothers aged ≥35 years was lower
(17.5% vs 38.5%; P=0.007). Maternal characteristics
were comparable between the two groups in terms
of ethnicity, booking status, parity, and body mass
index. The prevalences of all medical diseases were
also comparable.
Table 3 and the Supplementary Figure a show
the respective incidences and distribution of the
causes of SB among multiple pregnancies. The most
common cause was fetal growth restriction (13;
28.9%), followed by TTTS [7; 15.5%]. Other causes of
SB included pre-eclampsia/hypertension (3; 6.7%),
congenital and genetic abnormalities (3; 6.7%),
chorioamnionitis (3; 6.7%), other maternal medical
diseases (2; 4.4%), cord-related pathology/accident
(1; 2.2%), and placental pathologies (1; 2.2%). There
were 12 (26.7%) unexplained SBs throughout the
study period, although the rate was significantly
lower in the second decade (2; 10%) than in the first
decade (10; 40%, P=0.002); otherwise, there were
no other substantial differences in the causes of SB
between the first and second decades. The causes of
SB differed between MC and non-MC groups: fetal
growth restriction (9; 33.3%) [P=0.014] and TTTS (7;
25.9%) [P=0.001] were the two most common causes
of SB in MC multiple pregnancies. Whereas one-third
of SBs in the non-MC group were unexplained,
fetal growth restriction (4; 22.2%), congenital and
genetic abnormalities (2; 11.1%), chorioamnionitis
(2; 11.1%), and pre-eclampsia/hypertension (2;
11.1%) were common causes in the non-MC group.
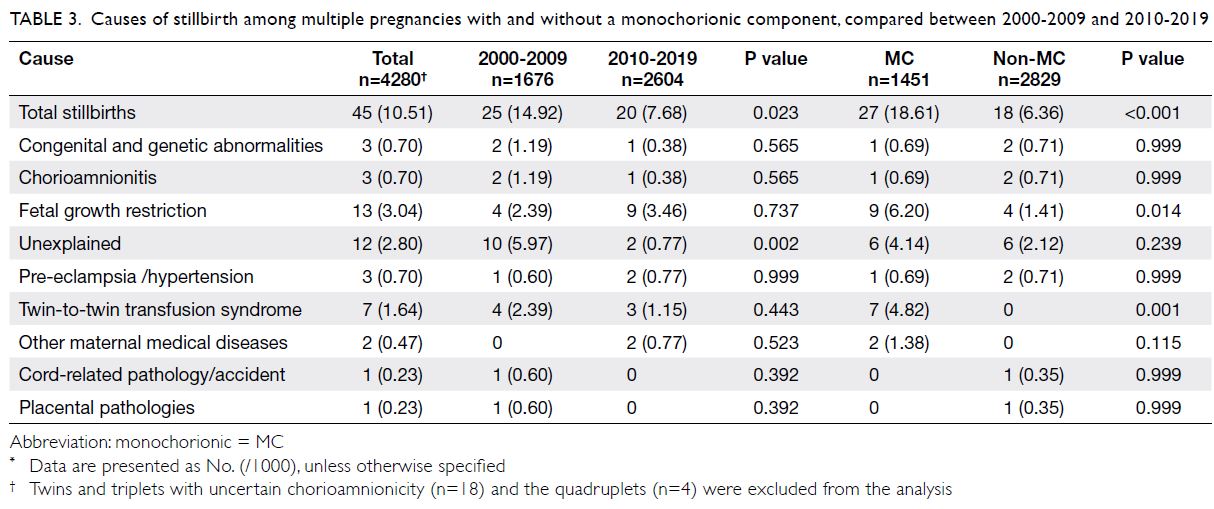
Table 3. Causes of stillbirth among multiple pregnancies with and without a monochorionic component, compared between 2000-2009 and 2010-2019
Details of neonatal deaths in multiple
pregnancies
The distribution of gestational ages at NND is shown in Table 4. In the ‘31 to 33 weeks’ group, the overall NND rate was significantly higher in the first decade
(19.23 per 1000 births) than in the second decade
(0 per 1000 births; P=0.035). In the ‘24 to 27 weeks’
group, the NND rate was significantly higher among
triplet pregnancies (545.45 per 1000 births) than
among twin pregnancies (215.38 per 1000 births;
P=0.031). Preterm birth before 34 weeks of gestation
in multiple pregnancies was significantly higher in
the first decade (18.5%) than in the second decade
(15.2%; P=0.006).
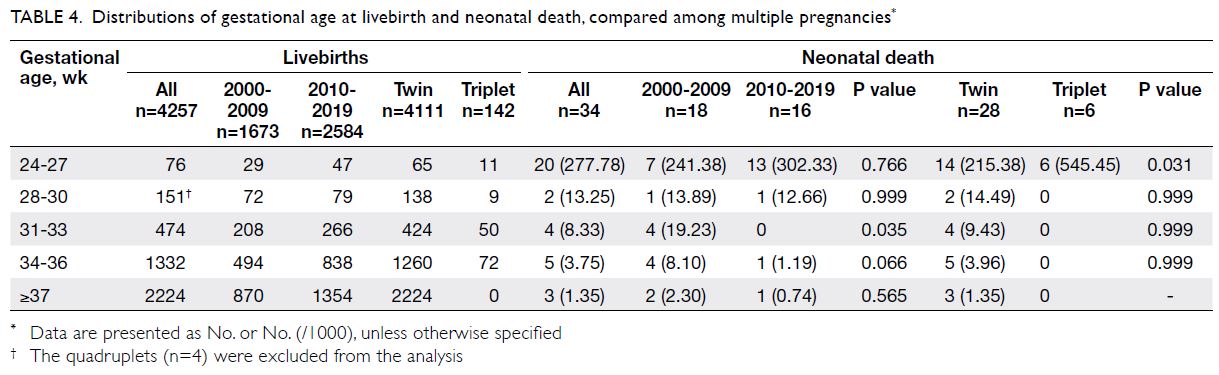
Table 4. Distributions of gestational age at livebirth and neonatal death, compared among multiple pregnancies
Regarding the causes of NND in multiple
pregnancies, prematurity (23; 67.6%) was the most
common cause, followed by congenital and genetic
abnormalities (8; 23.6%), birth asphyxia (2; 5.9%),
and sepsis (1; 2.9%) [Table 5 and Supplementary Fig b]. There were no significant differences in
the incidences of various causes of NND between
the first and second decades. However, a greater
proportion of NNDs in the MC group was caused
by prematurity, compared with the non-MC group
(11.24 per 1000 births vs 2.49 per 1000 births;
P=0.001) [Table 5].
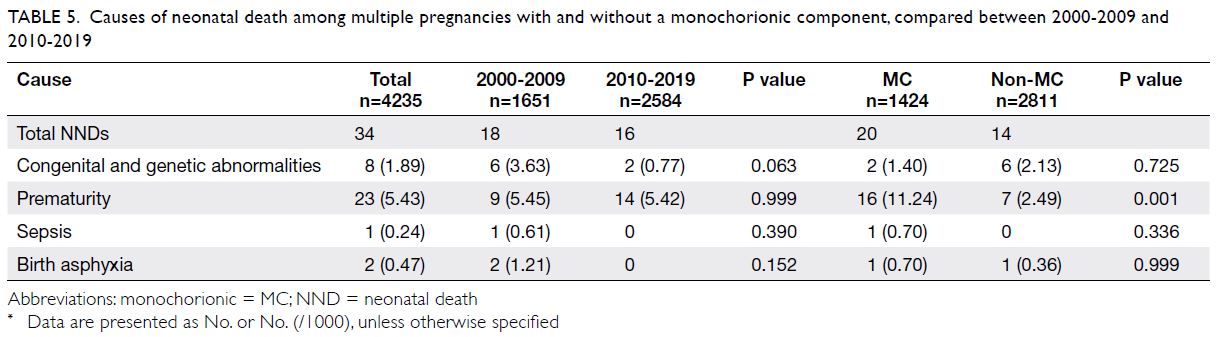
Table 5. Causes of neonatal death among multiple pregnancies with and without a monochorionic component, compared between 2000-2009 and 2010-2019
Changes in maternal demographics during
the study period
Between the first and second decades, there were several statistically significant trends in maternal
demographics, including a higher maternal age in
the second decade (31.6 ± 5.3 years vs 33.3 ± 5.2
years; P<0.001), as well as greater proportions of
mothers aged ≥35 years (29.7% vs 43.4%; P<0.001)
and ≥40 years (4.8% vs 8.0%; P=0.004). The overall
mean booking body mass index was significantly
lower in the second decade (23.1 ± 3.7 kg/m2 vs
22.7 ± 3.3 kg/m2; P=0.011). The prevalence of non-booked
cases was also significantly lower in the
second decade (11.2% vs 4.7%; P<0.001). Women of
Chinese ethnicity remained the predominant group
(96.9% vs 94.9%), but there was an increase in the
proportion of deliveries by women of Southeast
Asian ethnicity (1.3% vs 4.3%; P<0.001). The
proportions of nulliparous women were similar
(63.9% vs 67%; P=0.150). In the second decade, there
were higher prevalences of chronic hypertension
(0% vs 1.1%; P=0.006) and pre-eclampsia/gestational hypertension (8.5% vs 11.2%; P=0.043), as well
as an increase in the rate of caesarean delivery
(65.0% vs 81.0%; P<0.001). Other differences in the
prevalences of medical diseases are summarised in
Supplementary Table 2 of the Appendix.
Discussion
Changes in the types of multiple pregnancies
and their perinatal mortality rates
To our knowledge, this is the first large study concerning the epidemiology and patterns of
perinatal mortality in multiple pregnancies during
a 20-year period in Hong Kong. In the second
decade, there were significantly more non-MC
twin pregnancies, compared with the first decade;
this was mainly because of the widespread use of
artificial reproductive technology. However, there
was no change in the number of non-MC triplet or
quadruplet pregnancies; this finding was presumably
related to changes in artificial reproductive
technology practices that restricted the number of
embryo transfers, controlled ovulation induction, and
implemented fetal reduction (ie, from higher order
pregnancies to twin pregnancies).14 The probability
of a spontaneous MC twin pregnancy is generally
stable (~1 in 300).15 The increased prevalence of
MC twin pregnancies in this cohort is presumably
related to the increased number of referrals received
by the obstetric unit involved in this study, which is
a specialised centre for the treatment of complicated
twin pregnancies via fetoscopic laser coagulation of
anastomoses or radiofrequency ablation of umbilical
vessels for selective fetal reduction.14 16 17 18 19 Embryos
produced by artificial reproductive technology also
have a higher probability of spitting and forming
MC multiple pregnancies.20 Compared with the
perinatal mortality in singleton pregnancies during
the same period, which we previously reported,13
the respective perinatal mortality rates in twin
pregnancies and triplet pregnancies were 3.6-fold
and 10.0-fold higher (4.16 in 1000 births [singleton] vs 14.93 in 1000 births [twin] vs 41.67 in 1000 births
[triplet]; P<0.05). The total perinatal mortality rate
in twin pregnancies was 45.4% lower in the second
decade than in the first decade (25.32 per 1000 births
[2000-2009] vs 13.82 per 1000 births [2010-2019]).
This difference was considerably larger than the
15.2% reduction we previously observed in singleton
pregnancies (4.54 per 1000 births [2000-2009] vs
3.85 per 1000 births [2010-2019]).13
Changes in the stillbirth rates
The improvement in perinatal mortality in multiple
pregnancies was a combined effect of reductions
in SB and late NND. Compared with SB rates in
twin and triplet pregnancies in the same obstetric
unit between 1988 and 1992,21 the SB rate for twin
pregnancies substantially decreased from 23.2 per
1000 births (1988-1992) to 14.9 per 1000 births
(2000-2009) and 7.53 per 1000 births (2010-2019).
The SB rate for triplet pregnancies also substantially
decreased from 66.7 per 1000 births (1988-1992) to
15.2 per 1000 births (2000-2009) and 12.8 per 1000
births (2010-2019). Our findings are comparable to
results from the UK, where the national SB rate in
twin pregnancies decreased from 17.58 per 1000
births (2000) to 6.16 per 1000 births (2016).22
The decline in SB rates since 1990 can be
attributed to improvements in care, including
the introduction of fetoscopic laser coagulation
for TTTS (in 2002)17 18 and the establishment of a
specialised multiple pregnancy clinic with a standard
protocol for close ultrasonographic monitoring
(in the late 2000s). The establishment of this clinic
ensured better care for these high-risk multiple
pregnancies; the additional monitoring allowed
earlier recognition of complications and greater
access to timely treatment.23 However, the effect of
radiofrequency ablation of the umbilical vessels for
selective fetal reduction, introduced in 2011, was
not revealed in this study because many multiple
pregnancies were regarded as singleton pregnancies
after fetal reduction.14 16 19 24
In the second decade, the proportion of
non-MC multiple pregnancies increased from 62.6%
[1049/(1049+627)] to 68.4% [1780/(1780+824)]; this
also reduced the overall perinatal mortality rate.
Furthermore, non-MC multiple pregnancies had
lower rates of total mortality (11.31 in 1000 births
vs 32.39 in 1000 births; P<0.001), perinatal mortality
(10.25 in 1000 births vs 26.88 in 1000 births; P<0.001),
and SB (6.36 in 1000 births vs 18.61 in 1000 births;
P<0.001), compared with MC multiple pregnancies.
This is consistent with findings from the UK, where
the SB rates were 3-5 in 1000 births (dichorionic
twin pregnancies) and 18-26 in 1000 births (MC
twin pregnancies) during the period of 2013-2016.
Comparison with singleton pregnancies
Notably, approximately half of the SBs in multiple pregnancies occurred between 24 and 27 weeks
of gestation, whereas only 25% of SBs in singleton
pregnancies occurred in this range of gestational
ages.13 This difference suggests that the underlying
diseases associated with SB were more severe
(with earlier onset) in multiple pregnancies than
in singleton pregnancies. When comparing the
aetiologies of SB between singleton and multiple
pregnancies, the multiple pregnancies group had
higher rates of SB caused by fetal growth restriction
(3.04 in 1000 births vs 0.49 in 1000 births), pre-eclampsia/
hypertension (0.70 in 1000 births vs 0.19
in 1000 births), other maternal medical diseases
(0.47 in 1000 births vs 0.11 in 1000 births), and
TTTS (specific to MC multiple pregnancies). In the
second decade, the proportion of unexplained SBs
in multiple pregnancies was significantly lower than
in the first decade (40% [2000-2009] vs 10% [2010-2019]); this change was not observed in singleton
pregnancies (33.3% [2000-2009] vs 39.1% [2010-2019]). We presumed that the difference was mainly
related to the close monitoring provided in multiple
pregnancies.
Whereas SBs in singleton pregnancies were
associated with older maternal age and obesity,
SBs in multiple pregnancies were associated with
significantly younger maternal age, compared
with livebirths in multiple pregnancies. Moreover,
the proportion of mothers aged ≥35 years was
significantly lower among multiple pregnancies
with SBs than among multiple pregnancies with
livebirths. This difference presumably can be
attributed to the younger age of mothers with MC
multiple pregnancies compared with mothers who
had non-MC multiple pregnancies; moreover, a
greater proportion of non-MC multiple pregnancies
were produced by artificial reproductive technology.
Changes in neonatal death rates
As in singleton pregnancies, prematurity was the most common cause of NND in multiple pregnancies.13 There was a significantly lower rate of preterm birth
before 34 weeks of gestation in multiple pregnancies
during the second decade (15.2%) than in the first
decade (18.5%; P=0.006); accordingly, the rates of
late NND and total NND were lower in the second
decade. After stratification according to gestational
age at birth, the NND rate was significantly higher in
triplet pregnancies than in twin pregnancies among
deliveries between 24 and 27 weeks of gestation.
However, the NND rate did not significantly differ
between singleton pregnancies (197.53 per 1000
births) and twin pregnancies (215.38 per 1000 births;
P=0.743). Thus, there is an unclear effect of order
of pregnancy on the NND rate in extreme preterm
births; the degree of prematurity is the main factor
that affects the NND rate.
The rate of caesarean delivery was significantly
lower in the first decade than in the second
decade (65.0% vs 81.0%; P<0.001). This difference
was mainly related to an increase in the elective
caesarean delivery rate for multiple pregnancies
(23.7% vs 42.5%); the emergency caesarean delivery
rate was similar between the first and second
decades (41.3% vs 38.5%). Women with the first
twin in cephalic presentation and overall stable
condition were offered a trial of vaginal delivery
and elective caesarean delivery. Because there is a
generally consistent probability that the first fetus is
in cephalic presentation, the higher rate of elective
caesarean delivery was mainly related to patient
choice and preference.
Strengths and limitations
This is the first large analysis of the prevalence and causes of SB and NND among multiple
pregnancies in Hong Kong. Most data regarding
chorioamnionicity, gestational age at SB, and basic
maternal demographics are complete and accurate.
The 20-year study period also allowed comparisons
between the first and second decades. However,
because our obstetric unit is the major referral centre
for complicated MC cases, the number of MC cases
in this study was higher than the number of cases in a
nearby obstetric unit (0.6% vs 0.4% of all pregnancies);
moreover, total perinatal mortality was higher in our
obstetric unit (32.77 per 1000 births during 2010-2019 [Table 2], vs 19 per 1000 births during 2011-2018).25 Notably, the analysis by the other obstetric
unit excluded MC triplet pregnancies, monoamniotic
twin pregnancies, and cases complicated by TTTS
or lethal anomalies, all of which carried a high risk of
perinatal mortality.25 Furthermore, clinical practices
might have changed during the 20-year study period,
potentially influencing the classification of causes of
SB. For example, the change from karyotyping to
chromosomal microarray may have led to additional
genetic disease diagnoses.26 Additionally, some
multiple pregnancies were reduced to singleton pregnancies, either spontaneously or by medical
intervention, before 24 weeks of gestation; these
pregnancies were regarded as singleton pregnancies.
Therefore, the effect of fetal reduction in these cases
was unclear. Finally, although this large cohort
provided extensive data concerning perinatal
mortality among multiple pregnancies in Hong
Kong, the dataset was insufficient for statistical
evaluation of rare events. Nonetheless, these
findings provide a basis for a territory-wide review
of perinatal outcomes in multiple pregnancies.
Conclusion
The prevalence of multiple pregnancies increased from 1.41% in 2000-2009 to 1.91% in 2010-2019,
but the total perinatal mortality rate decreased
from 25.32 per 1000 births to 13.82 per 1000 births.
This change in the total perinatal mortality rate was
related to reductions in the rates of SB and NND,
which resulted from improvements in antenatal care
and neonatal intensive care.
Author contributions
Concept or design: SL Lau, TY Leung.
Acquisition of data: All authors.
Analysis or interpretation of data: SL Lau, STK Wong, WT Tse, TY Leung.
Drafting of the manuscript: SL Lau, TY Leung.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: SL Lau, STK Wong, WT Tse, TY Leung.
Drafting of the manuscript: SL Lau, TY Leung.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
Ethical approval was obtained from the Joint Chinese University of Hong Kong–New Territories East Cluster
Clinical Research Ethics Committee (Ref CRE 2017.442).
References
1. Collins J. Global epidemiology of multiple birth. Reprod Biomed Online 2007;15 Suppl 3:45-52. Crossref
2. Russo FM, Pozzi E, Pelizzoni F, et al. Stillbirths in singletons,
dichorionic and monochorionic twins: a comparison
of risks and causes. Eur J Obstet Gynecol Reprod Biol
2013;170:131-6. Crossref
3. Sherer DM. Adverse perinatal outcome of twin pregnancies
according to chorionicity: review of the literature. Am J
Perinatol 2001;18:23-37. Crossref
4. Hack KE, Derks JB, Elias SG, et al. Increased perinatal mortality and morbidity in monochorionic versus
dichorionic twin pregnancies: clinical implications of a
large Dutch cohort study. BJOG 2008;115:58-67. Crossref
5. Lewi L, Jani J, Blickstein I, et al. The outcome of
monochorionic diamniotic twin gestations in the era of
invasive fetal therapy: a prospective cohort study. Am J
Obstet Gynecol 2008;199:514.e1-8. Crossref
6. Lee YM, Wylie BJ, Simpson LL, D’Alton ME. Twin
chorionicity and the risk of stillbirth. Obstet Gynecol
2008;111:301-8. Crossref
7. Ananth CV, Chauhan SP. Epidemiology of twinning in
developed countries. Semin Perinatol 2012;36:156-61. Crossref
8. Manktelow BN, Smith LK, Seaton SE, et al; on behalf of the
MBRRACE-UK collaboration. MBRRACE-UK perinatal
mortality surveillance report. UK perinatal deaths for
births from January to December 2014. Available from:
https://www.npeu.ox.ac.uk/assets/downloads/mbrraceuk/
reports/MBRRACE-UK-PMS-Report-2014.pdf.
Accessed 1 Mar 2022.
9. Healthcare Quality Improvement Partnership Ltd.
MBRRACE-UK. Perinatal mortality surveillance
report 2018. Available from: https://www.hqip.org.uk/
resource/mbrrace-uk-perinatal-mortality-surveillancereport-
2018/. Accessed 1 Mar 2022.
10. Healthcare Quality Improvement Partnership Ltd.
CMACE and CEMACH reports. Stillbirth, neonatal and
post-neonatal mortality 2002-2003 from CEMACH.
Available from: https://www.hqip.org.uk/resource/cmace-and-cemach-reports/. Accessed 1 Mar 2022.
11. National Collaborating Centre for Women’s and Children’s
Health (UK). Multiple Pregnancy: The Management of
Twin and Triplet Pregnancies in the Antenatal Period.
London: RCOG Press; 2011.
12. Khalil A, Giallongo E, Bhide A, Papageorghiou AT,
Thilaganathan B. Reduction in twin stillbirth following
implementation of NICE guidance. Ultrasound Obstet
Gynecol 2020;56:566-71. Crossref
13. Wong ST, Tse WT, Lau SL, Sahota DS, Leung TY. Stillbirth
rate in singleton pregnancies: a 20-year retrospective study
from a public obstetric unit in Hong Kong. Hong Kong
Med J 2022;28:285-93. Crossref
14. Tse WT, Law LW, Sahota DS, Leung TY, Cheng YK. Triplet
pregnancy with fetal reduction: experience in Hong Kong.
Hong Kong Med J 2017;23:326-32. Crossref
15. Sperling L, Kiil C, Larsen LU, et al. Naturally conceived
twins with monochorionic placentation have the highest
risk of fetal loss. Ultrasound Obstet Gynecol 2006;28:644-52. Crossref
16. Ting YH, Poon LC, Tse WT, et al. Outcomes of
radiofrequency ablation for selective fetal reduction
before vs at or after 16 gestational weeks in complicated
monochorionic pregnancy. Ultrasound Obstet Gynecol
2021;58:214-20. Crossref
17. Lau TK, Leung TY, Fung TY, Leung TN. Treatment of
twin-twin transfusion syndrome by fetoscopic laser
photocoagulation. Chin Med J (Engl) 2004;117:1431-4.
18. Yang X, Leung TY, Ngan Kee WD, Chen M, Chan LW,
Lau TK. Fetoscopic laser photocoagulation in the
management of twin-twin transfusion syndrome:
local experience from Hong Kong. Hong Kong Med J
2010;16:275-81.
19. Lu J, Ting YH, Law KM, Lau TK, Leung TY. Radiofrequency ablation for selective reduction in complicated monochorionic multiple pregnancies. Fetal Diagn Ther 2013;34:211-6. Crossref
20. Saravelos SH, Zhang T, Chung JP, et al. Monochorionic
quadramniotic and triamniotic pregnancies following
single embryo transfers: two case reports and a review of
the literature. J Assist Reprod Genet 2016;33:27-32. Crossref
21. Lau TK, Li CY. A perinatal audit of stillbirths in a teaching
hospital in Hong Kong. Aust N Z J Obstet Gynaecol 1994;34:416-21. Crossref
22. Kurinczuk JJ, Draper ES, Field DJ, et al. Experiences with
maternal and perinatal death reviews in the UK—the
MBRRACE-UK programme. BJOG 2014;121 Suppl 4:41-6. Crossref
23. Pan M, Chen M, Leung TY, Sahota DS, Ting YH, Lau TK.
Outcome of monochorionic twin pregnancies with
abnormal umbilical artery Doppler between 16 and 20 weeks of gestation. J Matern Fetal Neonatal Med
2012;25:277-80.Crossref
24. Ting YH, Lao TT, Law KM, Cheng YK, Lau TK, Leung TY.
Pseudoamniotic band syndrome after in-utero intervention
for twin-to-twin transfusion syndrome: case reports and
literature review. Fetal Diagn Ther 2016;40:67-72. Crossref
25. Yu FN, Mak AS, Chan NM, Siu KL, Ma TW, Leung KY.
Prospective risk of stillbirth and neonatal complications
for monochorionic diamniotic and dichorionic diamniotic
twins after 24 weeks of gestation. J Obstet Gynaecol Res
2021;47:3127-35. Crossref
26. Hui AS, Chau MH, Chan YM, et al. The role of chromosomal
microarray analysis among fetuses with normal karyotype
and single system anomaly or nonspecific sonographic
findings. Acta Obstet Gynecol Scand 2021;100:235-43. Crossref

