© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Luxatio erecta of the hip in a 64-year-old man:
a case report
Kemal Gokkus, MD; Mehmet S Sahin, MD
Department of Orthopedics and Trauma, Baskent University Medical Faculty–Alanya Research and Practice Center, Turkey
Corresponding author: Dr Kemal Gokkus (kemalg@baskent.edu.tr)
Case report
In March 2021, a 64-year-old man who was injured
in a fall was brought to our emergency department.
He had lost his balance and fallen while harvesting
avocados from a tree. He reported severe right hip
and right lateral chest pain and was unable to move
his right hip. His vital signs were unremarkable. He
held his right hip in flexion and abduction (Fig 1a).
The limb was neurologically intact and good distal
arterial pulses were present. Plain anteroposterior
radiograph of the pelvis revealed an inferior
dislocation of the femoral head (Fig 1b).
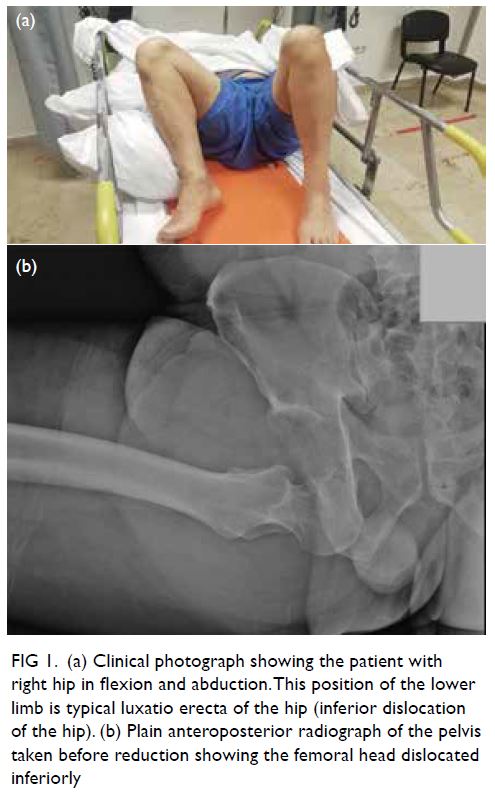
Figure 1. (a) Clinical photograph showing the patient with right hip in flexion and abduction. This position of the lower limb is typical luxatio erecta of the hip (inferior dislocation of the hip). (b) Plain anteroposterior radiograph of the pelvis taken before reduction showing the femoral head dislocated inferiorly
Computed tomography (CT) scan of the chest
(not shown) revealed an ipsilateral nondisplaced rib
(8-10) and scapular spine fractures. A CT scan of the pelvis (Fig 2) demonstrated an empty acetabulum
with no associated fractures. Later, the patient was
brought to the operating theatre and 0.5 mg/kg
propofol and 0.5 μg/kg remifentanil administered
intravenously for the first 90 s. Thereafter, further
doses of both propofol 0.25 mg/kg and remifentanil
0.25 μg/kg were administered. After 3 to 4 minutes
the patient was adequately sedated and pain-free.
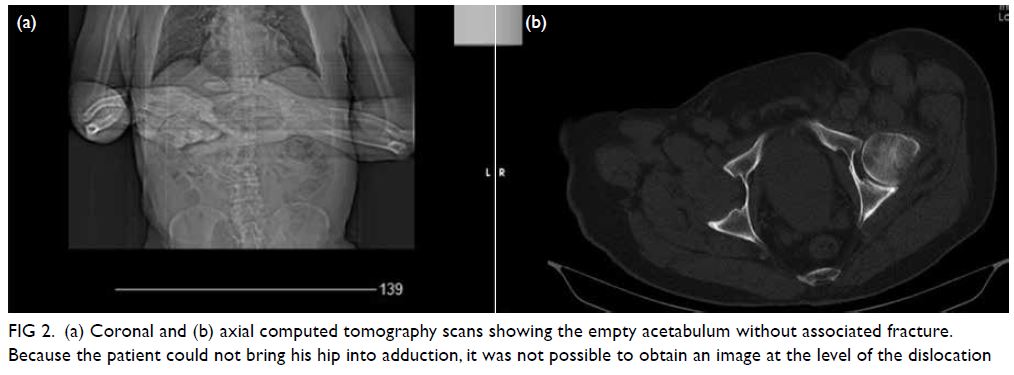
Figure 2. (a) Coronal and (b) axial computed tomography scans showing the empty acetabulum without associated fracture. Because the patient could not bring his hip into adduction, it was not possible to obtain an image at the level of the dislocation
The dislocation was reduced under sedation
and fluoroscopy by manual traction in the line of
deformity, initially followed by adduction of the
femur, resulting in an uneventful reduction (Video 1). Fluoroscopy confirmed that the hip range of
motion was safe after reduction; the hip was safe at
90° of flexion, 20° of adduction, 30° of abduction, and
30° of internal or external rotation.
After clinic follow-up the next day, the patient was discharged home and advised to remain on bed
rest for 3 weeks, and to use a walker (with toe-touch
weight-bearing) solely for going to the toilet.
To prevent heterotopic bone formation and
thromboprophylaxis, 25-mg indomethacin orally
3 times daily and 0.4-mL enoxaparin sodium daily
were prescribed for the first 2 weeks after surgery.
The use of indomethacin for prophylaxis is well
documented in the literature and its use to prevent
heterotopic ossification following treatment for
posterior hip dislocation with acetabular fractures
has been reported by Mitsionis et al.1 Deep venous
thrombosis has rarely been reported after an isolated
hip dislocation.1 Nevertheless, indomethacin for
prophylaxis was prescribed to our patient in view
of the need for prolonged bed rest and his relatively
advanced age.
At follow-up examination 3 weeks after
reduction, the patient was able to bear weight with a
mildly antalgic gait (Video 2). The observed antalgic
gait prompted us to be more conservative so the
patient was advised to avoid strenuous activity and
to use crutches with partial weight-bearing. At the
same visit, a post-reduction radiograph and CT scan
was performed to rule out chip or flake fractures of
the femoral head or acetabulum during reduction; if
hip pain persists, a magnetic resonance imaging scan
can be performed to look for evidence of a labral tear.
No associated acetabular or femoral head fracture
was observed (Fig 3). The patient will continue to be monitored for a year for possible aseptic necrosis
and myositis ossificans.
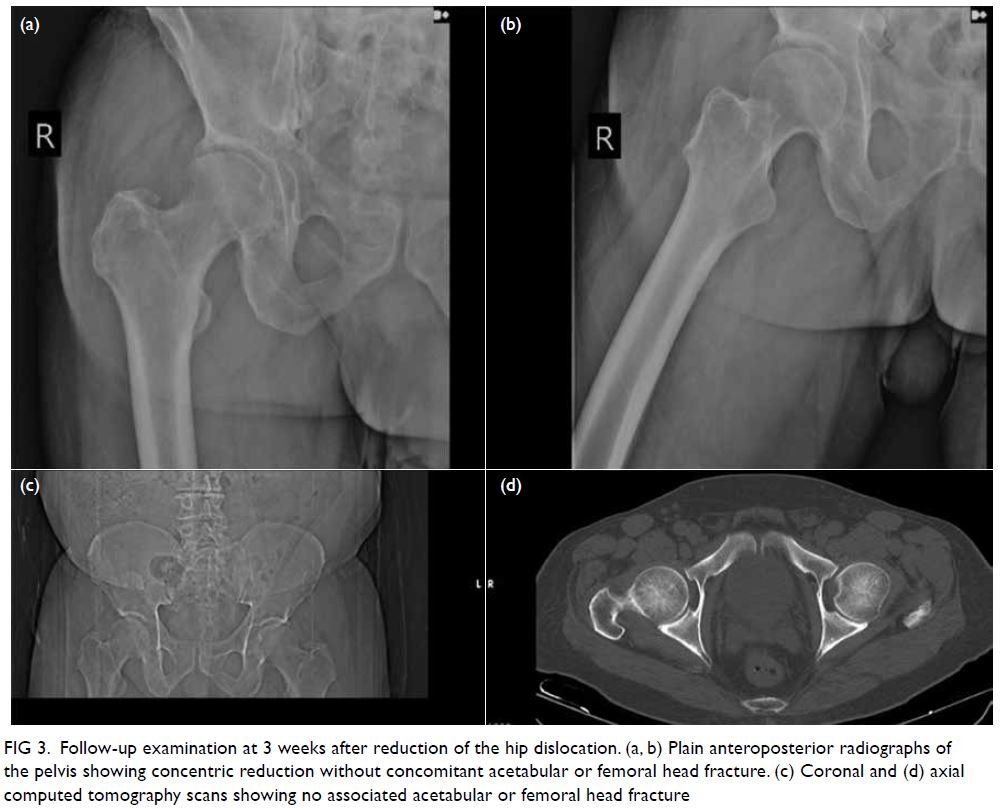
Figure 3. Follow-up examination at 3 weeks after reduction of the hip dislocation. (a, b) Plain anteroposterior radiographs of the pelvis showing concentric reduction without concomitant acetabular or femoral head fracture. (c) Coronal and (d) axial computed tomography scans showing no associated acetabular or femoral head fracture
Discussion
There are two types of inferior hip dislocation: obturator and ischial. Parvaresh et al2 analysed
acetabular development and concluded that between the ages of 12 and 16, the three ossification centres
and triradiate cartilage are ossified in both sexes. It is
realistic then to consider it an adult hip if the patient
is >16 years.2 Few cases of inferior (ischial type) hip
dislocation have been reported. We reviewed the
English-language literature search and found only
five reported cases of inferior hip dislocation in
adult patients (age >16 years).3 4 5 6 7 Among them, our patient is the oldest case reported with uneventful reduction.
Traumatic hip dislocation can cause
complications that include avascular necrosis
(6%-27% for early closed reduction), post-traumatic
osteoarthritis (17%-48%), heterotopic ossification
(up to 32%),1 8 and sciatic nerve injury (approximately 10%).9 To avoid complications, early and uneventful
reduction is critical. In our patient, reduction was
achieved within 2 hours of initial presentation.
Our patient may be the only case documented with
radiographic imaging performed before and after the
reduction (including CT) and video of the reduction
manoeuvre and a clinical video of the patient
(demonstrating the patient walking in the third week
after the reduction).
Brogdon and Woolridge10 described the
mechanism of ischial and obturator injury. In the
ischial type, the person falls on the trunk with the hip
flexed and lands on the flexed knee. The accumulated
force from further flexion of the upper trunk and
body weight may create the momentum to push
the femoral head inferiorly through the shallow and
relatively rimless inferior margin of the acetabulum.
Treatment consists of closed reduction under
sedation or general anaesthesia with axial traction,
together with gradual extension of the femur with
additional internal rotation manoeuvres.9
The common obturator type of dislocation
occurs when the femur is physically abducted and
twisted outwards when the patient slips or when
another force is applied. If the forcible abduction
and external rotation continue with flexion against
the pelvis, the femur is levered anteriorly out
of the acetabulum. Treatment comprises closed
reduction under sedation/general anaesthesia with
longitudinal traction in the direction of the femoral
axis and gentle adduction and flexion of the hip with
additional internal rotation manoeuvres.10
There is a strong consensus in the literature that CT examination be performed prior to reduction to
assess a probable acetabular wall fracture or head
split fracture of the femoral head.8 In the present case,
we could not complete all markings on the CT scan
because the abducted hip automatically blocked the
CT platform. Fortunately, we evaluated the anterior
and posterior acetabular walls and confirmed no
remnants in the acetabular fossa nor any fractures
on the acetabular walls. Based on the reduction and
stability confirmed by physical examination after the
reduction, radiographic examination after reduction
and CT was postponed until 3 weeks after reduction,
when the patient was allowed to fully weight bear for
the first time.
Inferior hip dislocation is rare and can
be successfully treated with closed reduction. Orthopaedic surgeons must be able to diagnose and
optimally treat this type of dislocation. This report
and videos serve as a teaching tool for this reduction
manoeuvre.
Author contributions
Concept or design: Both authors.
Acquisition of data: Both authors.
Analysis or interpretation of data: Both Gokkus.
Drafting of the manuscript: K Gokkus.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: Both authors.
Analysis or interpretation of data: Both Gokkus.
Drafting of the manuscript: K Gokkus.
Critical revision of the manuscript for important intellectual content: All authors.
Both authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
Both authors have no conflicts of interest to disclose.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patient was treated according to the principles of the Declaration of Helsinki. The patient provided informed consent for all treatments, procedures, and consent for
publication.
References
1. Mitsionis GI, Lykissas MG, Motsis E, et al. Surgical management of posterior hip dislocations associated with posterior wall acetabular fracture: a study with a minimum
follow-up of 15 years. J Orthop Trauma 2012;26:460-5. Crossref
2. Parvaresh KC, Pennock AT, Bomar JD, Wenger DR, Upasani VV. Analysis of acetabular ossification from the
triradiate cartilage and secondary centers. J Pediatr Orthop
2018;38:e145-50. Crossref
3. Kolar MK, Joseph S, McLaren A. Luxatio erecta of the hip. J Bone Joint Surg Br 2011;93:273. Crossref
4. Singh R, Sharma SC, Goel T. Traumatic inferior hip dislocation in an adult with ipsilateral trochanteric fracture. J Orthop Trauma 2006;20:220-2. Crossref
5. Walther MM, McCoin NS. Luxatio erecta of the hip. J Emerg Med 2013;44:985-6. Crossref
6. Tekin AÇ, Çabuk H, Büyükkurt CD, Dedeoğlu SS, İmren Y, Gürbüz H. Inferior hip dislocation after falling from height: a case report. Int J Surg Case Rep 2016;22:62-5. Crossref
7. Zeytin AT, Kaya S, Kaya FB, Ozcelik H. Traumatic inferior hip dislocation. J Med Cases 2015;6:238-9. Crossref
8. Yang RS, Tsuang YH, Hang YS, Liu TK. Traumatic dislocation of the hip. Clin Orthop Relat Res 1991;(265):218-27. Crossref
9. Cornwall R, Radomisli TE. Nerve injury in traumatic dislocation of the hip. Clin Orthop Relat Res 2000;(377):84-91.Crossref
10. Brogdon BG, Woolridge DA. Luxatio erecta of the hip: a critical retrospective. Skeletal Radiol 1997;26:548-52. Crossref

